What Exactly Is an Active Ingredient?
When you pick up a bottle of pain reliever, cold medicine, or allergy pill from the shelf, you’re not just buying a brand name. You’re buying a specific chemical that does the actual work inside your body. That chemical is the active ingredient. It’s the part of the medicine that relieves your headache, reduces your fever, or dries up your runny nose. Everything else - the color, the shape, the flavor, even the brand logo - is just packaging.
The U.S. Food and Drug Administration (FDA) requires every over-the-counter (OTC) medicine to list its active ingredient clearly on the Drug Facts label. This isn’t optional. It’s the law. And it’s there to protect you. Without knowing what’s in the pill or liquid, you could accidentally take too much - or mix two medicines that do the same thing, which can be dangerous.
The Drug Facts Label: Your Secret Weapon
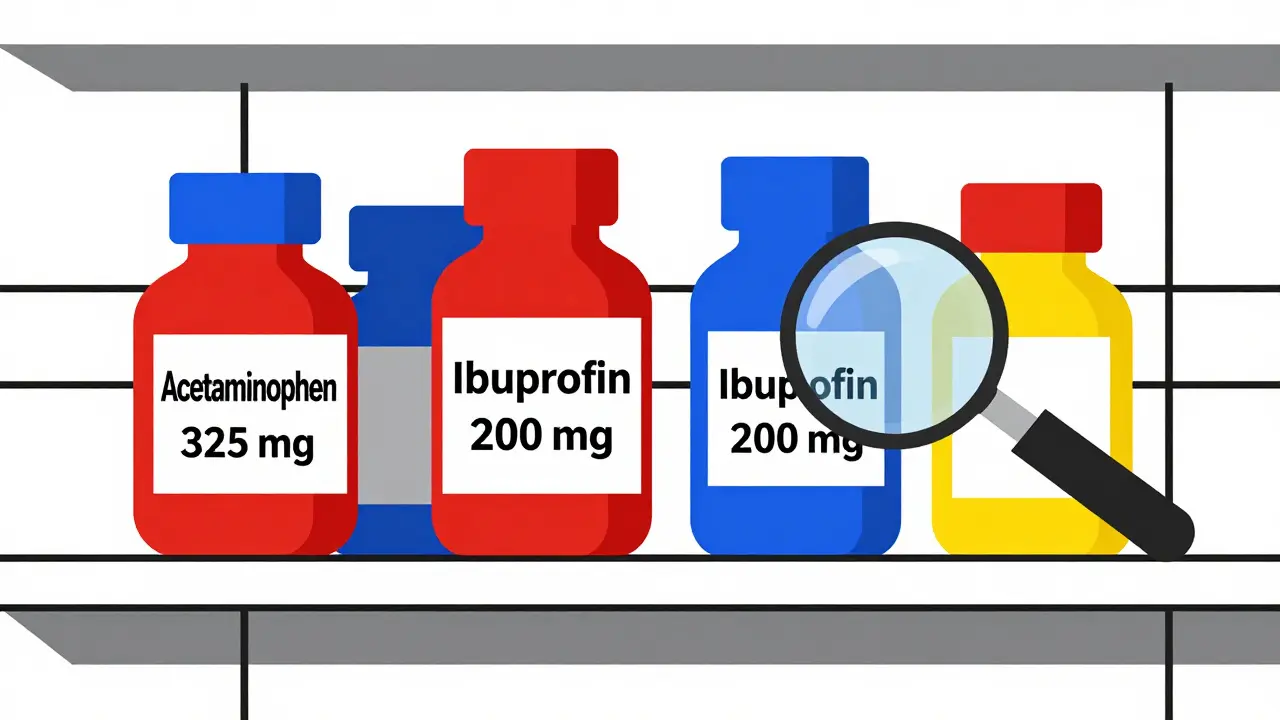
Look at the back of any OTC medicine bottle. The top section, right under the product name, is labeled Active Ingredient. That’s your first and most important stop. This section tells you exactly what chemical is doing the job and how much of it is in each dose.
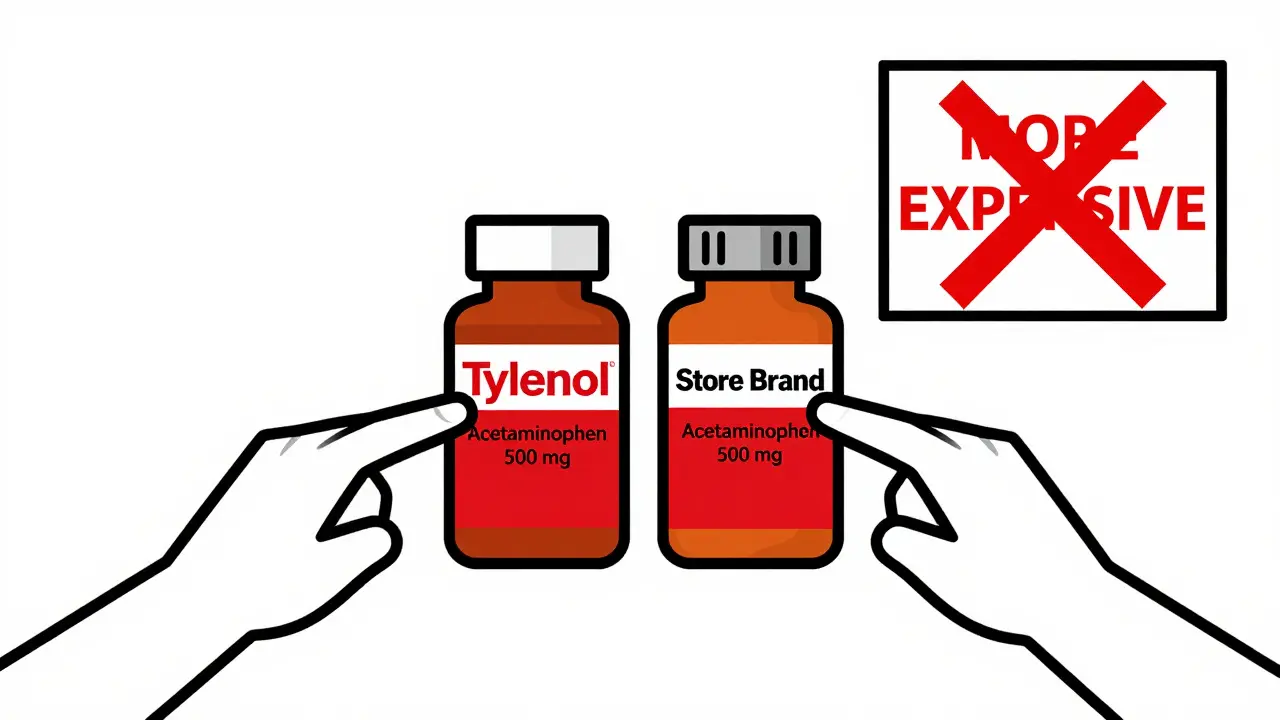
Here’s how it reads: acetaminophen 325 mg or ibuprofen 200 mg. That’s it. No fluff. No marketing. Just the name and the amount. The FDA requires this format so you can compare products across brands. Tylenol, Up&Up, and CVS Health all sell acetaminophen. The active ingredient is the same. The price is what’s different.
Many shoppers think different brand names mean different effects. They’re wrong. A store-brand ibuprofen and Advil have the same active ingredient, same dose, same effect. The only difference is the cost. Paying more for a name brand doesn’t mean you’re getting a stronger medicine - unless the active ingredient amount is higher, which it usually isn’t.
Why You Can’t Ignore the Numbers
It’s not enough to know that a medicine contains acetaminophen. You need to know how much. A single tablet might have 325 mg. Another might have 500 mg. A liquid might have 160 mg per 5 mL. If you take two of the 500 mg tablets, you’re hitting 1,000 mg - double the dose of the first.
That’s why overdoses happen. People take Tylenol for a headache. Then they take a cold medicine that also has acetaminophen. They don’t realize both contain the same active ingredient. By the time they feel sick, their liver is already under stress. In 2022, acetaminophen was the leading cause of acute liver failure in the U.S., and most cases were accidental.
The FDA limits OTC acetaminophen to 650 mg per tablet in combination products and 500 mg in single-ingredient tablets. But some older products still have higher doses. Always check the label. Never assume. The maximum daily dose for adults is 4,000 mg. Go over that, and you risk serious liver damage.
Common Active Ingredients and What They Do
You don’t need to memorize every chemical name. But knowing these five will help you make smarter choices:
- Acetaminophen - Pain and fever relief. Found in Tylenol, Excedrin, TheraFlu, and many cold medicines.
- Ibuprofen - Pain, fever, and inflammation. Found in Advil, Motrin, and store brands. Works better than acetaminophen for muscle aches or menstrual cramps.
- Naproxen sodium - Longer-lasting pain relief. Found in Aleve. Good for arthritis or back pain that lasts all day.
- Diphenhydramine - Allergy relief and sleep aid. Found in Benadryl, NyQuil, and ZzzQuil. Makes you drowsy - don’t drive after taking it.
- Dextromethorphan - Cough suppressant. Found in Robitussin, Delsym, and many multi-symptom cold products.
Notice how some ingredients do more than one thing? Diphenhydramine helps with allergies and sleep. That’s why nighttime cold medicines often cause drowsiness. Daytime versions avoid it. Always read the label to know what you’re signing up for.
Combination Products: The Hidden Danger
Multi-symptom cold and flu medicines are the most confusing. One pill might contain four active ingredients: acetaminophen for pain, dextromethorphan for cough, phenylephrine for congestion, and diphenhydramine for runny nose. That sounds helpful - until you realize you’re already taking acetaminophen for your headache.
A 2023 Consumer Reports survey found that 63% of adults couldn’t identify active ingredients just by looking at the product name. Only 28% knew that Aleve contains naproxen sodium. That’s not just ignorance - it’s a public health risk.
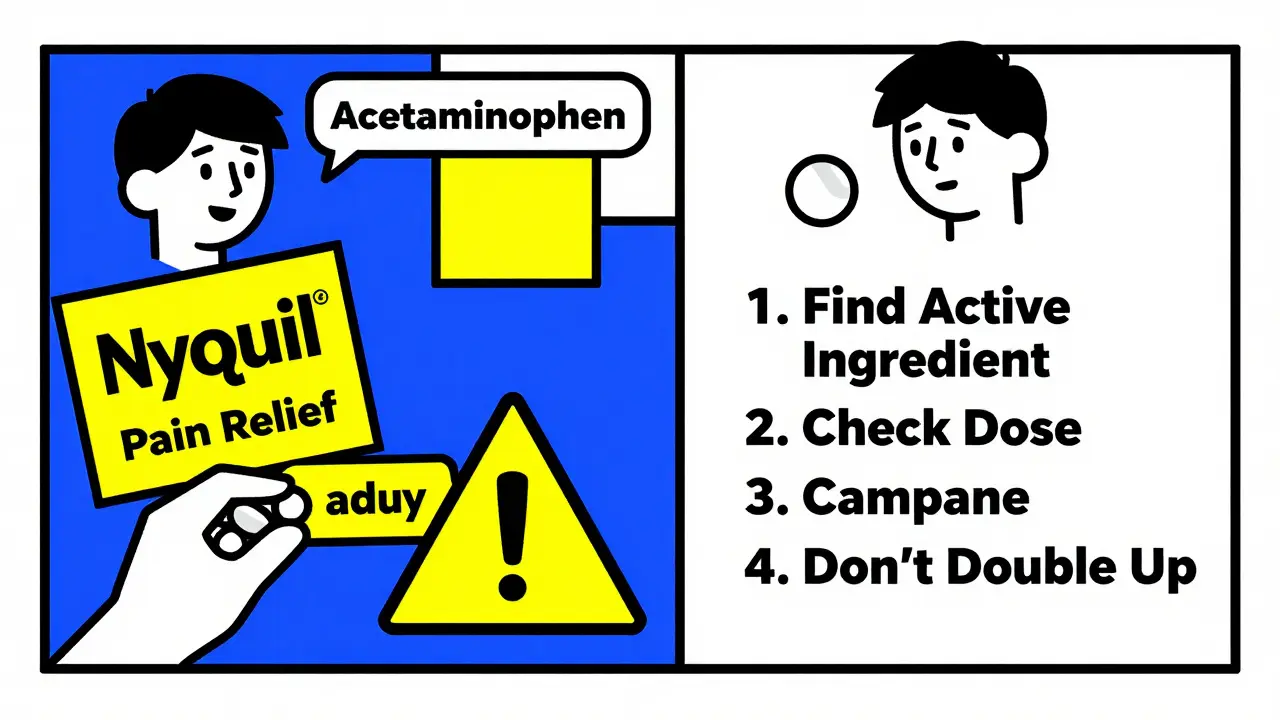
Here’s a real example: A man takes NyQuil for his cold. He also takes a store-brand pain reliever because his head still hurts. He doesn’t check the labels. Both contain acetaminophen. He ends up taking 3,000 mg in 12 hours - well over the safe limit. He wakes up vomiting, confused, and ends up in the ER. This happens more often than you think.
How to Avoid Mistakes: A Simple 4-Step Plan
You don’t need a pharmacy degree to stay safe. Just follow these steps every time you buy or take an OTC medicine:
- Find the Active Ingredient section. It’s always at the top of the Drug Facts label. Don’t skip to the Uses or Warnings - go straight here.
- Match the ingredient to your need. Are you treating pain? Fever? Cough? Allergies? Make sure the ingredient matches what you want to fix.
- Check the dose. Is it 200 mg? 325 mg? 500 mg? Write it down if you’re taking more than one product.
- Compare with other meds. Are you taking anything else? Even vitamins or supplements? Look at those labels too. If two products have the same active ingredient, don’t take them together.
Pro tip: Keep a small notebook or note on your phone listing all the active ingredients you take regularly. That way, when you’re at the store, you can quickly check if a new product duplicates something you’re already using.
What About Inactive Ingredients?
They’re not active - but they can still matter. Inactive ingredients are the fillers, dyes, flavors, and preservatives. They don’t treat your symptoms, but they can cause reactions. If you’re allergic to red dye #40, gluten, or certain sugars, check the Inactive Ingredients section.
One parent on a parenting forum shared that her toddler broke out in hives after taking Children’s Motrin. She didn’t realize the red dye in the liquid was the culprit. She switched to a dye-free version - and the rashes stopped. That’s why reading the whole label matters, even if you’re focused on the active ingredient.
The Bigger Picture: Why This Matters Now
The FDA is pushing hard to make OTC labels clearer. By 2026, all OTC medicines will need a QR code that links to a digital version of the Drug Facts label with even more detail - including allergen warnings and dosage reminders. This is a direct response to the thousands of preventable hospital visits each year.
Meanwhile, a $4.2 million public education campaign called Know Your Active Ingredients is running in pharmacies nationwide. Early results show a 19% drop in acetaminophen-related ER visits in stores that use the campaign materials. That’s not just marketing - it’s saving lives.
Final Thought: You’re in Control
OTC medicines are safe when used correctly. But they’re not harmless. The power to use them safely lies in your hands - literally. The next time you reach for a bottle, pause. Read the label. Don’t rely on memory. Don’t assume. Don’t rush. The active ingredient is the only thing that matters. Everything else is noise.
Can I take two different OTC medicines if they have different brand names?
Only if they don’t contain the same active ingredient. Brand names like Tylenol, Advil, and Aleve are just labels. The real difference is in the active ingredient. Taking two products with acetaminophen - even if one is called Tylenol and the other is called Cold & Flu Relief - can lead to a dangerous overdose. Always check the Active Ingredient section before combining any medicines.
Is generic OTC medicine as effective as name-brand?
Yes, if the active ingredient and dose are the same. Generic OTC drugs must meet the same FDA standards as brand-name versions. A store-brand ibuprofen with 200 mg per tablet works exactly like Advil. The only differences are price, packaging, and sometimes inactive ingredients like flavor or dye. Save money - and read the label to confirm the active ingredient matches.
Why do some OTC medicines have lower doses than prescription ones?
OTC medicines are designed for short-term, self-managed use. The FDA limits their active ingredient amounts to reduce the risk of misuse. For example, OTC ibuprofen is capped at 200 mg per tablet, while prescription versions can be 400-800 mg. This keeps daily doses safe for people who aren’t under a doctor’s supervision. If you need higher doses, talk to a healthcare provider.
What should I do if I accidentally take too much of an OTC medicine?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms to appear. For acetaminophen overdose, liver damage can start within hours - and may not show symptoms until it’s serious. Keep the medicine bottle handy so you can tell them the exact active ingredient and amount taken. If you’re unsure, go to the ER. Better safe than sorry.
Are there any active ingredients I should avoid completely?
Not if used as directed. But some ingredients require extra caution. Loperamide (Imodium) is an opioid that’s safe for occasional diarrhea but can cause fatal heart problems if taken in large doses. People have abused it to get high - and over 160 deaths have been linked to it since 2012. Also, avoid products with multiple active ingredients unless you have multiple symptoms. More ingredients = more chances for mistakes.




Solomon Ahonsi
February 1, 2026 AT 17:45Wow, another lecture on reading labels. Congrats, you just told everyone to not be dumb. I’ve been taking generic ibuprofen for years and never died. Your post reads like a FDA pamphlet someone forced you to write.
George Firican
February 2, 2026 AT 23:06There’s something deeply human about how we treat medicine like it’s magic - we trust the bottle, the color, the logo, as if the shape of the pill holds the cure. But the truth is far more mundane: it’s a molecule, a precise arrangement of atoms, doing its quiet job inside us. We don’t need branding. We don’t need hype. We just need to look. The label isn’t bureaucracy - it’s the last line of defense between us and harm. And yet, we glance at it like it’s a menu we’re too busy to read. Maybe the real crisis isn’t overdose - it’s our collective refusal to pause.
Matt W
February 4, 2026 AT 20:00This is actually super helpful. I used to just grab whatever was on sale until my buddy ended up in the ER from mixing Tylenol and NyQuil. Now I always check the active ingredient first - even if I’m in a hurry. Seriously, if you take more than one OTC med, write it down. It’s that simple. Thanks for laying it out like this.
Anthony Massirman
February 5, 2026 AT 22:14Same active ingredient = same effect. Stop overpaying.
Marc Durocher
February 6, 2026 AT 16:10Let me get this straight - you’re telling me that the reason people are overdosing isn’t because they’re stupid, but because they’re assuming the brand name means something different? And we’re surprised by this? I once bought ‘Allergy Relief’ thinking it was just for sneezing… turns out it had enough diphenhydramine to knock out a horse. Welcome to the jungle, folks.
Chinmoy Kumar
February 7, 2026 AT 10:45Bridget Molokomme
February 8, 2026 AT 05:32So let me get this straight - you’re telling me that I’ve been paying $12 for Advil when I could’ve been paying $2 for the exact same thing? And I thought I was being a smart shopper. Thanks for the reality check, I’m going to go buy 1000 ibuprofen and throw a party.
Brittany Marioni
February 10, 2026 AT 01:57PLEASE, for the love of all that is holy, read the label. I’ve seen people take Tylenol, then take a cold medicine, then take another cold medicine - and then wonder why they’re vomiting at 3 a.m. It’s not a mystery. It’s not complicated. It’s just… laziness. The Drug Facts label is not optional. It’s your lifeline. Don’t skip it. Don’t assume. Don’t be the person in the ER asking, ‘Wait, was that in there too?’
Monica Slypig
February 10, 2026 AT 16:54Why do we even need this post? In America, we have the best medical system in the world - if you can’t read a label, maybe you shouldn’t be allowed to buy medicine. This isn’t rocket science. It’s third-grade science. If you can’t handle this, maybe move to a country where people actually know what they’re putting in their bodies.
Becky M.
February 11, 2026 AT 12:02just wanted to say… this was really helpful. i’m from a country where otc meds are sold like candy and i didn’t realize how different it is here. i always just picked the one with the cute packaging. now i know to look for the active ingredient first. thanks for taking the time to write this - it matters more than you know.