Ethnicity-Based Drug Response Calculator
Drug Response Risk Assessment
This tool estimates potential differences in drug response based on ethnicity and common genetic factors. It's designed to help clinicians consider pharmacogenomic principles when prescribing.
Results
Key Genetic Factors
Clinical Recommendations
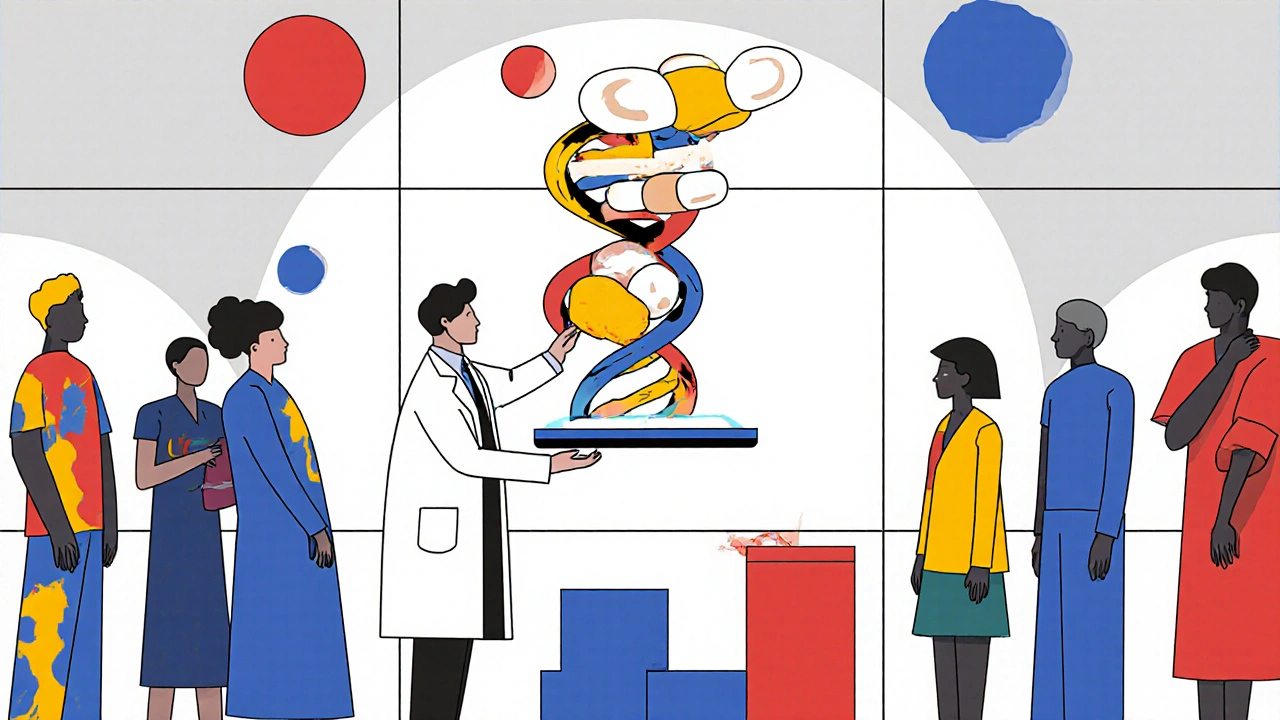
When a prescription is written, the same pill can act very differently in two patients just because they come from different ancestral backgrounds. Ethnicity and drug response is the observed variation in how drugs are absorbed, metabolized, and cleared among racial and ethnic groups, driven largely by genetic polymorphisms in enzymes, transporters, and drug targets. Understanding those variations is the cornerstone of modern Pharmacogenomics, a field that aims to match the right drug to the right person instead of a one‑size‑fits‑all approach.
Why genetics matters more than skin colour
Race is a social construct, but the genetic ancestry that often correlates with self‑identified ethnicity can explain why certain groups experience side‑effects or reduced efficacy. For example, the CYP2C19*2 loss‑of‑function allele appears in roughly 15‑20% of East Asians but only 2‑5% of African Americans. That single difference alters the antiplatelet effect of clopidogrel, making the drug less protective for many Asian patients unless a genotype‑guided alternative is chosen.
Key drug‑metabolizing enzymes
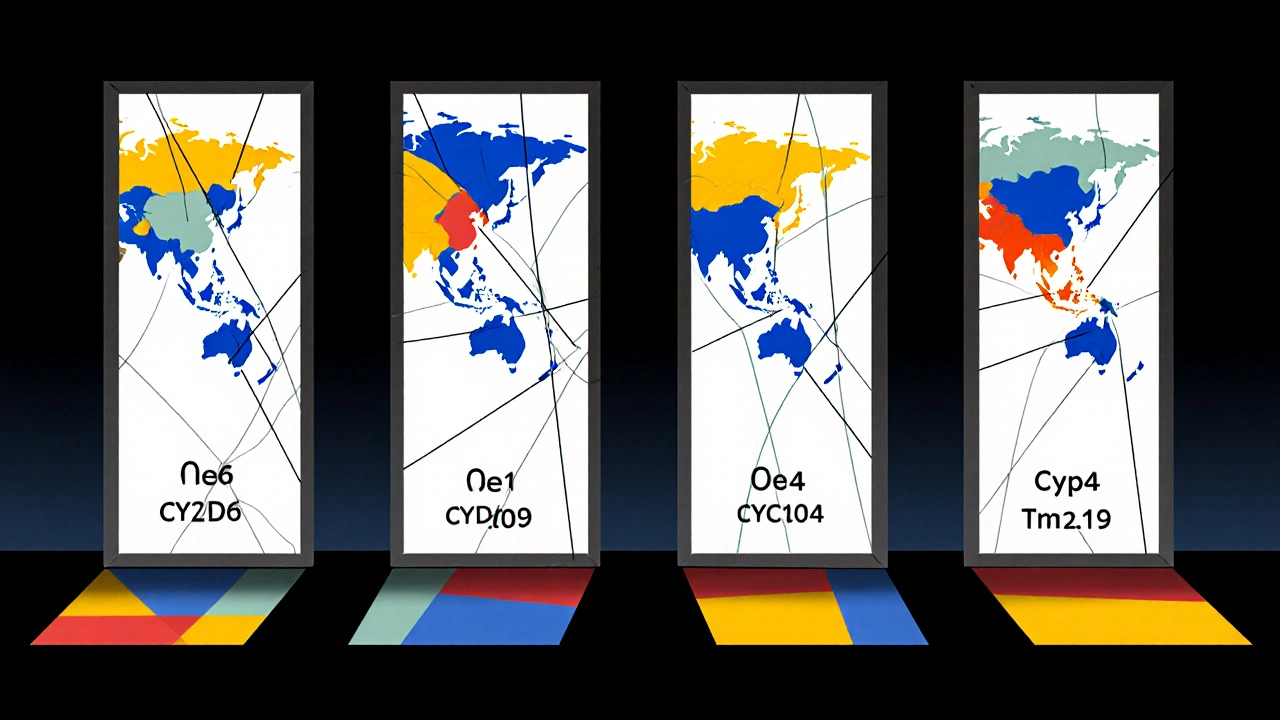
Four cytochrome P450 (CYP) enzymes dominate the metabolism of about 70% of cardiovascular and psychiatric drugs. Their allele frequencies differ sharply across continents:
- CYP2D6: extensive gene duplication in some Middle‑Eastern populations creates ultrarapid metabolizers, leading to sub‑therapeutic levels of metoprolol.
- CYP2C9: the *3 allele is common in European ancestry (≈7%) but rare in African ancestry, affecting warfarin dose calculations.
- CYP3A4: modest activity differences, yet the *22 variant is more frequent in Europeans, influencing statin exposure.
- CYP2C19: highlighted above for clopidogrel; also impacts proton‑pump inhibitor metabolism.
Notable drug‑ethnicity interactions
Beyond enzymes, a handful of genetic markers dictate severe adverse reactions:
| Marker | Most affected ethnic groups | Drug(s) impacted | Clinical consequence |
|---|---|---|---|
| HLA‑B*15:02 | Han Chinese, Thai, Malaysian (10‑15%) | Carbamazepine | Up to 1,000‑fold higher risk of Stevens‑Johnson syndrome |
| G6PD deficiency | African American males (10‑14%), Sub‑Saharan African, Mediterranean (5‑30%) | Primaquine, Dapsone, Sulfa drugs | Hemolytic anemia, potentially fatal |
| CYP2C19*2 | East Asians (15‑20%) | Clopidogrel | Reduced antiplatelet effect, higher cardiovascular event risk |
| CYP2C9*2 / *3 | European ancestry (≈7‑10%) | Warfarin | Over‑anticoagulation if standard dosing used |
Cardiovascular drugs also show ethnic trends. African Americans typically respond 30‑50% less to ACE inhibitors, prompting the FDA‑approved isosorbide dinitrate/hydralazine combo specifically for self‑identified African‑American patients with heart failure. Yet 30‑40% of that population still benefits from ACE inhibitors, underscoring the overlap between groups.
Clinical guidelines that incorporate ethnicity
The Clinical Pharmacogenetics Implementation Consortium (CPIC) now publishes 27 gene‑drug guidelines, many of which flag ethnicity. For instance, CPIC recommends using alternative antiplatelet agents (ticagrelor or prasugrel) when a patient carries CYP2C19 loss‑of‑function alleles. The American Heart Association’s 2023 statement pushes for genotype‑driven dosing of anticoagulants rather than race‑based dosing, arguing that ancestry panels predict warfarin dose more accurately than self‑reported race.
Implementation in practice still needs training. A 2022 survey found clinicians spend 8-12 hours mastering pharmacogenomic reports, and a typical health system requires 3-6 months to embed decision‑support tools into electronic health records.
Barriers and future directions
Despite rapid market growth-the global pharmacogenomics market hit $8.3 billion in 2022-several hurdles remain:
- Under‑representation: only ~19% of genome‑wide studies include non‑European participants, limiting the accuracy of allele frequency data for many groups.
- Cost: comprehensive panels run $1,200‑$2,500, a barrier for community hospitals where only 37% offer testing.
- Mixed ancestry: patients with blended heritage may not fit any single ethnic label, requiring full‑genome ancestry estimation.
Emerging solutions include polygenic risk scores that combine dozens of variants, showing 40‑60% better dosing predictions than single‑gene tests. Large‑scale biobanks like the NIH All of Us program aim to fill diversity gaps, already enrolling 3.5 million participants with 80% from minority groups.
Practical take‑aways for prescribers
- Ask about genetic testing before prescribing high‑risk drugs (e.g., carbamazepine, warfarin, clopidogrel).
- When testing isn’t available, consider known ethnic trends: avoid ACE inhibitors as first‑line in African‑American heart‑failure patients unless genetic data suggest otherwise.
- Use CPIC or other reputable guideline tables to translate genotype results into dosing recommendations.
- Document both self‑identified race and genetic ancestry when possible; this data improves future research.
- Stay updated on FDA label changes-many now require genotype warnings instead of race‑based warnings.
By blending genetic insight with an understanding of social determinants, clinicians can move from blanket ethnicity shortcuts to truly personalized therapy.
How does ethnicity differ from genetic ancestry?
Ethnicity is a self‑identified cultural label, while genetic ancestry reflects the actual DNA segments inherited from different population groups. Ancestry can be measured with genome sequencing, providing a more precise predictor of drug‑metabolizing variants than ethnicity alone.
Should I test every patient for CYP variants?
Not yet. Targeted testing is most cost‑effective for drugs with strong genotype‑response links, such as clopidogrel (CYP2C19), warfarin (CYP2C9/VKORC1), and carbamazepine (HLA‑B*15:02). Many institutions are moving toward pre‑emptive panels that include these genes.
What are the risks of using race as a prescribing cue?
Relying on race can oversimplify complex genetics, miss within‑group variability, and reinforce health disparities. It may lead to suboptimal drug choices for individuals who don’t fit the average profile of their self‑identified group.
Is pharmacogenomic testing covered by insurance?
Coverage varies. Private insurers increasingly reimburse panels for high‑risk drugs, while Medicare covers testing for specific indications such as clopidogrel in acute coronary syndrome. Checking local policies is essential.
How can I stay current with ethnicity‑related drug guidelines?
Subscribe to CPIC updates, follow FDA label revisions, and join professional societies that publish annual pharmacogenomics newsletters. Many hospitals embed guideline alerts directly into electronic health records.



Barbara Ventura
October 26, 2025 AT 16:11Reading through the data on CYP variations, it’s clear that population genetics isn’t just academic trivia, it directly shapes drug efficacy, especially for clopidogrel, metoprolol, and warfarin, and that’s something clinicians need to internalise, because a one‑size‑fits‑all script can leave patients under‑treated or over‑exposed, the allele frequencies you quoted are a good reminder that East Asian groups carry a higher burden of CYP2C19*2, while African‑American cohorts have distinct CYP2D6 copy‑number profiles, so when you see a prescription, think beyond the label, think about the genotype, and maybe push for pre‑emptive testing where feasible, the cost barrier is real, but the long‑term savings in avoided adverse events can be substantial.
Miracle Zona Ikhlas
October 26, 2025 AT 16:36The key takeaway is to match genotype with drug choice whenever possible. A quick check of CYP2C19 status can prevent clopidogrel failures in many Asian patients. Keeping guidelines handy, like CPIC tables, makes this process smoother.
naoki doe
October 26, 2025 AT 17:10From a pharmacogenomic standpoint, the data you presented underscores the necessity of integrating ancestry panels into routine labs; however, rolling that out in a community clinic demands resources and staff training, which many practices still lack. That said, even a simple questionnaire about family origin can flag patients who might benefit from targeted testing.
sarah basarya
October 26, 2025 AT 17:26Honestly, it’s mind‑boggling how many prescribers still rely on vague “race‑based” heuristics when the science is literally at their fingertips! The HLA‑B*15:02 risk for Stevens‑Johnson syndrome is a perfect example of how a single allele can turn a routine carbamazepine prescription into a life‑threatening gamble. If you ignore those markers, you’re basically playing roulette with patient lives.
Samantha Taylor
October 26, 2025 AT 18:00One cannot overstate the irony of a health system that touts personalized medicine while clinging to outdated racial proxies. The CPIC guidelines, published over a decade ago, already delineate precise gene‑drug pairs, yet many clinicians persist in prescribing ACE inhibitors to African‑American heart‑failure patients without genetic confirmation. This paradox becomes even more glaring when insurance companies reimburse genotype panels for clopidogrel but balk at covering warfarin testing. Moreover, the market data indicating an $8.3 billion pharmacogenomics sector does little to convince a skeptical physician who sees only the upfront cost. The literature you cited on under‑representation of non‑European genomes is a stark reminder that our predictive models are built on a skewed foundation. Consequently, the allele frequency estimates for CYP2C9*3 in African populations remain speculative at best. The All of Us initiative, while commendable, still has a long road ahead before its findings translate into bedside decisions. In practice, most hospital formularies lack auto‑alerts for HLA‑B*15:02, leaving clinicians to rely on memory. The subtle but crucial difference between self‑identified ethnicity and genetic ancestry is often glossed over in medical curricula. A deeper appreciation of this nuance could prevent countless adverse drug reactions. The FDA’s recent label updates for carbamazepine illustrate a move toward genotype‑specific warnings, yet those changes are buried beneath dense regulatory language. It would be far more effective to embed concise, actionable alerts directly into electronic health records. If we continue to treat “race” as a convenient shortcut, we risk perpetuating health disparities under the guise of efficiency. Ultimately, the goal should be a healthcare ecosystem where a patient’s DNA, not their zip code, dictates therapy. Until that vision materialises, we are merely rearranging deck chairs on the Titanic of imprecision.
Joe Langner
October 26, 2025 AT 18:33Wow, that was a marathon of insight, and I’m totally with you on needing more DNA‑driven alerts; even if my keyboard’s got a mind of its own, I think we can all agree the future’s bright when we stop guessing based on skin tone and start looking at the genome, rite?
Ben Dover
October 26, 2025 AT 19:06The presented allele frequency matrices warrant a rigorous statistical appraisal; however, the omission of confidence intervals for each population undermines the robustness of the conclusions, suggesting that the authors may have over‑interpreted the applicability of these data to clinical decision‑making frameworks.
Katherine Brown
October 26, 2025 AT 19:23While the previous comment rightly highlights methodological gaps, it is equally pertinent to acknowledge that the integration of pharmacogenomic data into prescribing algorithms remains constrained by limited sample diversity, a factor that should temper any extrapolation to broader patient cohorts.
Tony Stolfa
October 26, 2025 AT 19:56Look, if you’re gonna keep tossing around fancy gene names without telling doctors how to actually use them, you’re just spitting out jargon for the sake of sounding smart, and that’s not helpful at all.
Joy Dua
October 26, 2025 AT 20:13Indeed, the cacophony of technical terminology can obscure practical guidance; a succinct, vividly illustrated roadmap would serve clinicians far better than a labyrinth of esoteric references.
Holly Kress
October 26, 2025 AT 20:46Mindful documentation of both self‑identified race and genetic ancestry is essential.