Opioid Treatment Medication Guide
How can we help you choose the best treatment option?
There's no one-size-fits-all answer for opioid use disorder treatment. This guide helps you understand which medication might be more appropriate based on your individual circumstances and needs. Take this quick quiz to learn more about how methadone and buprenorphine compare for your situation.
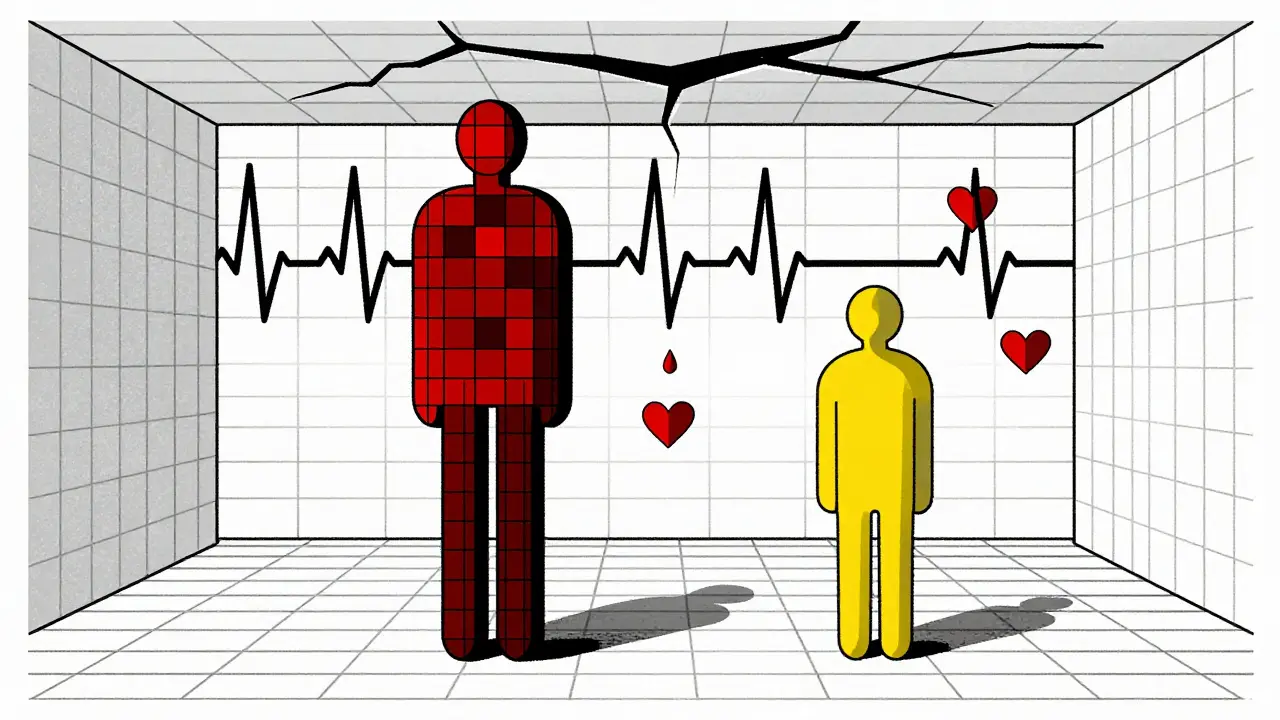
When someone is fighting opioid use disorder, choosing the right medication can mean the difference between staying in recovery and relapsing. Methadone and buprenorphine are two of the most effective tools available, but they come with very different side effect profiles. Neither is perfect. Both can make life harder in some ways-even as they save it in others. Understanding what these side effects really feel like, how often they happen, and which ones are dangerous is not just helpful-it’s essential.
What Methadone Does to Your Body
Methadone is a full opioid agonist. That means it fully activates the same brain receptors as heroin or fentanyl, but without the highs and crashes. It’s been used for decades to stabilize people with severe opioid dependence. But because it’s so strong, the side effects are often noticeable-and sometimes overwhelming.
Most people on methadone report feeling drowsy, especially in the first few weeks. About 18% to 28% say they’re so sleepy they can’t focus at work or drive safely. Some describe it as feeling like they’re walking through thick fog all day. Constipation is another major issue. Around 25% to 40% of users need laxatives daily. One Reddit user wrote, “I haven’t had a normal bowel movement in six months. I’m on three different meds just to go.”
Then there’s the heart risk. Methadone can stretch out the QT interval on an EKG-a sign of irregular heartbeat. At doses over 100mg per day, this happens in up to 35% of patients. That’s not just a lab result. It can lead to sudden cardiac arrest, especially if someone is also taking other meds like antidepressants or antibiotics. Doctors now recommend an EKG before starting methadone and again after a few weeks if the dose is high.
Sexual side effects are rarely discussed but very common. Around 30% of long-term methadone users report trouble getting or keeping an erection. Libido drops. For many, this isn’t just embarrassing-it’s deeply isolating. And unlike some side effects, this one doesn’t fade with time.
Respiratory depression is the biggest fear. Methadone slows breathing. At high doses, especially during the first weeks of treatment, that can be deadly. Overdose risk is highest in the first 4 weeks, and it’s 2.5 times higher than with buprenorphine. Mixing methadone with alcohol, benzodiazepines, or sleep aids multiplies that risk by 300% to 400%.
What Buprenorphine Feels Like
Buprenorphine is different. It’s a partial agonist. Think of it like a dimmer switch instead of an on/off button. It eases cravings and stops withdrawal, but doesn’t produce the same intense opioid effect. That’s why it’s safer-but also why some people feel it doesn’t work well enough.
The most common complaint? Mouth problems. If you’re taking Suboxone (buprenorphine + naloxone) as a film under the tongue, you’ll likely get numbness, tingling, or soreness in your mouth. About 25% to 35% of users report this. Some say it feels like their tongue is asleep. Swallowing the film instead of letting it dissolve cuts absorption by up to 60%, so proper technique matters.
Headaches are another big one. Around 30% to 40% of buprenorphine users get them regularly. Not just mild ones-some are constant and sharp. One patient on Healthgrades wrote, “I took Suboxone for three months. Every day, my head felt like it was being squeezed. I couldn’t sleep.”
But the biggest frustration for many is the ceiling effect. Buprenorphine’s effects max out around 16-24mg per day. For someone with high opioid tolerance-say, someone who used fentanyl daily for years-that dose might not be enough. They might still have cravings. They might still use on the side. One user said, “Suboxone kept me from going into withdrawal, but I still thought about heroin every hour. I felt stuck.”
Respiratory depression is far less likely with buprenorphine. Because of its ceiling effect, even if someone takes 100mg, their breathing won’t slow to dangerous levels. That’s why it’s safer for home use. But here’s the catch: if you take buprenorphine too soon after using another opioid, you can trigger sudden, intense withdrawal-called precipitated withdrawal. It happens in 15% to 25% of first-time users who don’t wait long enough.

Which One Is Safer?
Safety isn’t just about overdosing. It’s about living well while on treatment.
Methadone has a higher risk of death during the first month. That’s why it’s given in supervised clinics, where you have to show up every day. You can’t miss a dose. You can’t take extra. That structure helps, but it’s also a burden. People lose jobs. Miss family events. Feel stigmatized.
Buprenorphine can be prescribed by a doctor in an office. You get a 30-day supply. You can travel. You can skip a day without crashing. But that freedom comes with a downside: people sometimes skip doses, or worse-sell their pills. Diversion rates for buprenorphine are about 2.8%, compared to just 0.2% for methadone.
Retention rates tell another story. In a 2024 study, 81.5% of people stayed on methadone after two years. Only 11.2% stayed on buprenorphine. That doesn’t mean buprenorphine doesn’t work-it means many people stop because the side effects are too much, or the dose isn’t strong enough.
And then there’s the cognitive toll. Both drugs can make you feel foggy. But methadone hits memory and attention harder. One study found methadone users scored 25-30% worse on visual memory tests than buprenorphine users. That’s not just inconvenient-it affects your ability to hold a job, study, or even remember to take your meds.
Real People, Real Side Effects
Numbers don’t tell the whole story. Real people share what it’s like.
On Reddit, methadone users talk about feeling like “a zombie.” One man said, “I went from shooting up every day to sitting on the couch all day. I didn’t feel high, but I didn’t feel alive either.”
Buprenorphine users say something different: “It didn’t fix my cravings. It just made my mouth numb.”
One woman on Healthgrades wrote: “I was on methadone for a year. I stopped because I couldn’t have sex anymore. I was so tired I couldn’t play with my kids. I didn’t feel like myself.”
Another said: “I switched to Suboxone because I didn’t want to go to a clinic every day. But now I’m still using heroin on weekends because Suboxone doesn’t take the edge off.”
These aren’t rare stories. They’re common. And they show that side effects aren’t just physical-they’re emotional, social, and deeply personal.
How to Manage These Side Effects
Side effects aren’t inevitable. They can be managed.
For constipation: Drink more water. Eat fiber. Try magnesium supplements. Don’t wait until you’re bloated and in pain. Start early.
For drowsiness: Don’t drive or operate heavy machinery for the first two weeks. Talk to your provider about adjusting your dose. Sometimes splitting it into two smaller doses helps.
For mouth issues with buprenorphine: Let the film dissolve completely under your tongue. Don’t eat or drink for 15 minutes before or after. Use a humidifier at night. Talk to your dentist about dry mouth.
For heart risks with methadone: Get an EKG before starting and again after 2-4 weeks. Tell your doctor about every other medication you take-even over-the-counter ones.
For cravings that won’t go away: Counseling helps. So does peer support. Medication alone isn’t enough. You need to rebuild your life, not just stop using.
And always carry naloxone. Even if you’re on buprenorphine, you’re still at risk if you use other drugs. Naloxone can save your life.
Which One Should You Choose?
There’s no one-size-fits-all answer.
If you’ve tried buprenorphine and it didn’t work-if you still crave opioids, still use, still feel trapped-methadone might be your next step. It’s more effective for high-tolerance users, especially those with fentanyl use.
If you’re new to treatment, live in a place without easy access to clinics, or have a history of heart problems or addiction to benzodiazepines, buprenorphine is often the safer start.
Some people switch. Start with buprenorphine. If it doesn’t work, move to methadone. That’s not failure. That’s strategy.
The goal isn’t to pick the “best” drug. It’s to pick the one that lets you live the life you want.
Side effects matter. But so does survival. So does stability. So does hope.






Meghan Hammack
January 9, 2026 AT 17:36I’ve been on buprenorphine for 14 months and honestly? My mouth feels like it’s been stuffed with cotton for a year. But I’m alive. I’m working. I’m seeing my niece grow up. That numb tongue? Worth it.
Jeffrey Hu
January 11, 2026 AT 01:43Everyone’s acting like these side effects are some kind of secret. Newsflash: opioids mess you up. Methadone makes you sleepy, buprenorphine makes your tongue feel like a dead fish. You knew this going in. Stop whining and get your life together.
RAJAT KD
January 12, 2026 AT 19:31My brother died on methadone. Heart stopped at 82mg. No one told us about QT prolongation. This post saved me from making the same mistake. Thank you.
Heather Wilson
January 13, 2026 AT 22:48Let’s be real: 81.5% retention on methadone vs 11.2% on buprenorphine? That’s not a treatment gap-that’s a failure of willpower. People quit because they’re lazy, not because the drug doesn’t work. If you can’t handle a little constipation or a dull headache, maybe you’re not ready to recover.
Micheal Murdoch
January 15, 2026 AT 19:04There’s no ‘right’ drug. Only the one that lets you breathe again. I was on methadone for two years. Felt like a ghost. Switched to buprenorphine-mouth went numb, headaches hit hard-but I started painting again. I started talking to my mom. That’s recovery. Not the absence of side effects. The presence of life.
Lindsey Wellmann
January 16, 2026 AT 19:23😭 I just want to feel sexy again… I’ve been on methadone 3 years. No libido. No spark. My husband left. I don’t blame him. But I miss me. 🌹
Alicia Hasö
January 17, 2026 AT 04:21To everyone who says ‘just push through’-you haven’t lived it. I lost my job because I couldn’t stay awake. I missed my daughter’s recital because I was too dizzy to drive. I cried in the bathroom at the clinic because I felt like a burden. This isn’t weakness. This is the cost of survival. And we deserve better than shame. We deserve care that sees the whole person-not just the addiction.
If you’re on this path, you’re already a warrior. Don’t let anyone make you feel small for needing help. You’re not broken. You’re rebuilding.
And yes, the constipation is brutal. I started chia seeds and magnesium. Changed my life. Small wins matter.
You are not alone. I see you. I’m here.
Jenci Spradlin
January 19, 2026 AT 01:58u/6664 you’re a dick. Not everyone has the luxury of ‘willpower.’ Some of us are homeless, on SSDI, or have trauma that makes ‘just trying harder’ impossible. Methadone saved my life. Buprenorphine gave me back my teeth. Stop blaming people for surviving.
Aron Veldhuizen
January 20, 2026 AT 18:49Is it not ironic that we’ve turned a pharmacological solution into a moral referendum? Methadone is a full agonist-so it’s ‘too strong.’ Buprenorphine is a partial agonist-so it’s ‘not enough.’ We want a drug that’s both perfectly safe and perfectly effective. But biology doesn’t care about our preferences. The opioid crisis didn’t arise because people were weak. It arose because capitalism turned pain into profit. And now we punish the wounded for needing medicine. We are not healing. We are ritualizing suffering.
Matthew Maxwell
January 21, 2026 AT 00:25People on buprenorphine who still use heroin? That’s not treatment failure. That’s choice. You don’t get to be a junkie and call yourself ‘in recovery.’ If you’re using on weekends, you’re not sick-you’re addicted to the high. Get real.
tali murah
January 23, 2026 AT 00:03Oh wow, a 10-page essay on how ‘side effects are deeply personal.’ Groundbreaking. Did you also mention that breathing is important? That water is wet? This post reads like a pharmaceutical ad written by a grad student who’s never held a real job. Everyone knows methadone makes you sleepy. Everyone knows buprenorphine gives you headaches. What’s new?
Ashley Kronenwetter
January 23, 2026 AT 05:54Thank you for writing this with such clarity and compassion. I’m a nurse who works in addiction medicine. I see the stigma every day. This post gives me something I can hand to families who think their loved one is ‘just choosing to be lazy.’ You’ve given them language. You’ve given them hope.