When life feels like a pressure cooker, the brain pays the price. Researchers now link everyday stressors to a higher chance of developing Alzheimer's disease, the most common form of dementia. Understanding that link helps you act before memory loss sets in.
What is Alzheimer’s disease?
Alzheimer's disease is a progressive neurodegenerative disorder characterized by accumulation of amyloid‑beta plaques and tau protein tangles, leading to loss of neurons and cognitive decline. It accounts for about 60‑70% of dementia cases worldwide and currently has no cure.
Defining chronic stress
Chronic stress refers to prolonged activation of the body's stress response systems, especially the hypothalamic‑pituitary‑adrenal (HPA) axis, which releases cortisol over weeks or months. Unlike a short‑term scare, chronic stress keeps the brain in a heightened state of alert.
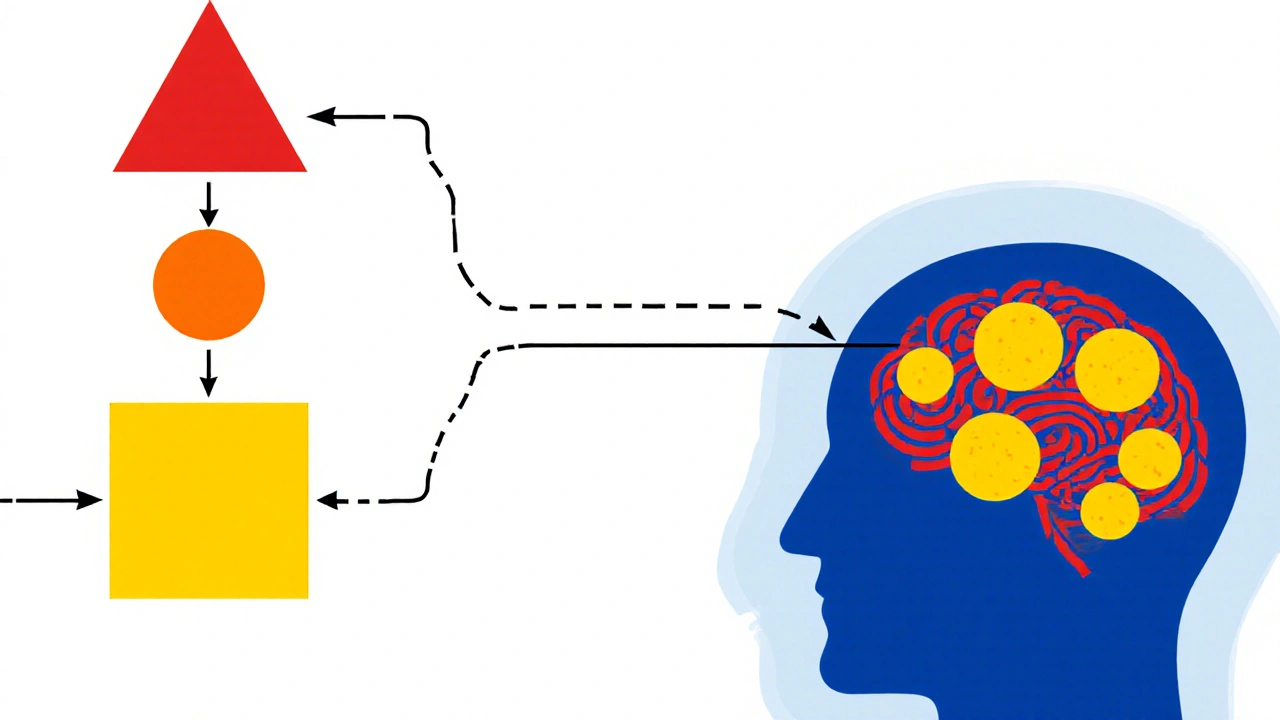
How stress talks to the brain
The HPA axis acts like a messenger route. When you perceive a threat, the hypothalamus signals the pituitary gland, which then tells the adrenal glands to pour out cortisol. In a healthy system, cortisol spikes and then drops. Under chronic stress, cortisol stays elevated, and that has several knock‑on effects:
- Cortisol overload damages neurons in the hippocampus, the region that stores new memories.
- High cortisol weakens the blood‑brain barrier, letting inflammatory proteins flood the brain.
- It spurs oxidative stress, which erodes cell membranes and DNA.
Key biological players linking stress and Alzheimer’s
Scientists have identified several molecules that sit at the crossroads of stress and Alzheimer’s pathology:
- Cortisol - high levels correlate with greater amyloid‑beta deposition in imaging studies.
- C‑reactive protein (CRP) - a marker of systemic inflammation that predicts faster cognitive decline.
- Glucocorticoid receptors - when overstimulated, they change how neurons process amyloid‑beta.
Evidence from human studies
Large cohort studies provide a clear picture. The 2023 Australian Longitudinal Study of Ageing tracked 7,500 adults for 15 years. Participants reporting high perceived stress had a 1.6‑fold increased risk of developing Alzheimer’s‑type dementia, even after adjusting for age, education, and APOE ε4 status.
Neuroimaging adds weight. A 2024 PET scan analysis of 1,200 seniors showed that those with chronically elevated cortisol levels had 23% more amyloid‑beta plaque burden than low‑cortisol peers.
Animal models reinforce the link
Mouse models engineered to overproduce amyloid‑beta reveal that chronic restraint stress accelerates plaque formation by 30% and worsens tau hyperphosphorylation. When researchers gave these mice a stress‑blocking drug that normalizes cortisol, plaque growth slowed dramatically.
Mitigating stress to lower Alzheimer’s risk
While you can’t erase a genetic predisposition like APOE ε4, you can tame the stress response. Here are practical steps backed by data:
- Physical exercise - 150 minutes of moderate aerobic activity per week lowers cortisol and improves hippocampal volume.
- Meditation and mindfulness - randomized trials show a 12% reduction in CRP after 8 weeks of daily practice.
- Sleep hygiene - 7-8 hours of quality sleep restores HPA balance and promotes amyloid clearance.
- Social engagement - strong social networks buffer stress hormones and are linked to a 20% lower dementia incidence.
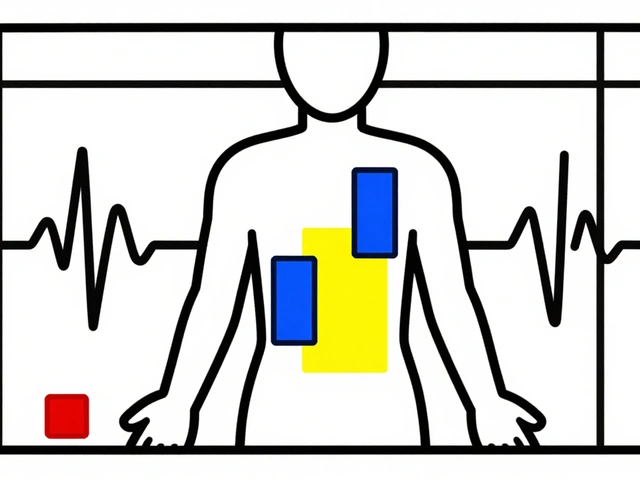
Comparing stress biomarkers and Alzheimer’s risk
| Biomarker | Typical Level (high stress) | Effect on brain | Associated risk increase |
|---|---|---|---|
| Cortisol | 15‑20µg/dL (saliva) | Hippocampal atrophy, blood‑brain barrier leakage | 1.5‑1.7× |
| CRP | >3mg/L | Neuroinflammation, tau phosphorylation | 1.3× |
| IL‑6 | >5pg/mL | Microglial activation | 1.2× |
Common misconceptions
Many think stress only hurts mental health, not brain cells. The science proves otherwise: stress hormones directly poison neurons. Another myth is that only “extreme” trauma matters. Everyday pressures-tight deadlines, caregiving, financial worries-can accumulate enough cortisol to tip the scale.
Future research directions
Upcoming trials examine drugs that specifically block glucocorticoid receptors in the brain. If successful, they could become the first disease‑modifying therapy targeting the stress pathway. Meanwhile, longitudinal studies using wearable cortisol monitors aim to map real‑time stress spikes to later amyloid imaging.
Take‑away checklist
- Recognize chronic stress as a modifiable dementia risk factor.
- Monitor stress levels-consider saliva cortisol tests if you’re over 50.
- Adopt at least two lifestyle habits that lower cortisol (exercise, meditation, sleep).
- Stay socially active and seek professional help for prolonged anxiety.
- Discuss stress management with your doctor during routine health checks.
Frequently Asked Questions
Can occasional stress cause Alzheimer’s?
Short bursts of stress trigger a normal cortisol spike that the brain recovers from quickly. It’s the long‑lasting, unrelenting stress that raises dementia risk.
Is there a test to measure stress‑related Alzheimer’s risk?
Doctors can order saliva or blood cortisol tests, and combine them with CRP or IL‑6 measurements. When paired with genetic screening for APOE ε4, these labs give a clearer risk picture.
Do anti‑anxiety medications lower Alzheimer’s risk?
Some studies suggest that SSRIs may reduce neuroinflammation, but evidence on direct dementia prevention is still mixed. Medication should complement, not replace, lifestyle changes.
How much exercise is enough to combat stress?
Guidelines recommend at least 150minutes of moderate aerobic activity a week-think brisk walking, cycling, or swimming. Adding two strength sessions can further stabilize cortisol.
Can diet influence the stress‑Alzheimer’s link?
Yes. Diets rich in omega‑3 fatty acids, antioxidants, and low in refined sugars reduce inflammation and may blunt cortisol spikes. The Mediterranean pattern is the most studied.
By treating stress as a serious health threat, you not only improve daily well‑being but also give your brain a fighting chance against Alzheimer’s. Start small, stay consistent, and watch the protective benefits add up.




Miriam Rahel
October 17, 2025 AT 13:57The hypothalamic‑pituitary‑adrenal axis functions as the central mediator of stress‑induced neurodegeneration. Chronic elevation of cortisol compromises hippocampal neurogenesis and accelerates amyloid‑beta aggregation, as documented in longitudinal PET studies. Moreover, glucocorticoid receptor hyper‑sensitivity alters tau phosphorylation pathways, thereby compounding tauopathy. Epidemiological data from the Australian cohort substantiate a statistically significant hazard ratio for high‑perceived stress after adjusting for APOE ε4 status. Consequently, therapeutic strategies that attenuate cortisol synthesis merit rigorous clinical investigation.
Samantha Oldrid
October 20, 2025 AT 12:10Oh sure, because sipping kale smoothies will magically erase decades of cortisol exposure. Meanwhile, the pharma lobby quietly waits to sell you the next “stress‑shield” pill.
lisa howard
October 23, 2025 AT 10:26Imagine waking up every morning with the weight of the world pressing down on your skull, as if an invisible hand is squeezing the very essence of your thoughts. You rush through traffic, answer endless emails, and still feel the hollow echo of a dread that never truly subsides. That relentless drumbeat is not merely a mental nuisance; it is a biochemical tyrant that hijacks the HPA axis and drowns your hippocampus in cortisol. Each spike carves micro‑lesions into memory circuits, turning simple recollections into jagged fragments. Over weeks and months those fragments coalesce into the very plaques and tangles that define Alzheimer’s pathology. Scientists have observed a 23 % increase in amyloid load among seniors with chronically elevated cortisol, a figure that should make any health‑conscious citizen sit up straight. The blood–brain barrier, once a vigilant sentinel, becomes porous under stress, allowing inflammatory proteins to infiltrate and wreak havoc. Oxidative stress follows, corroding cellular membranes like rust on an abandoned bridge. Even your immune cells, tasked with cleaning up debris, become confused and start attacking healthy neurons. You might think meditation or a jog will fix it, but the reality is that only sustained, multimodal interventions can recalibrate the system. Regular aerobic exercise expands hippocampal volume, while mindfulness practices have been shown to shave off measurable units of CRP. Social engagement, too, acts as an emotional buffer, reducing the cortisol surge that would otherwise cascade unchecked. Yet, in our culture that glorifies hustle, taking the time to breathe becomes an act of rebellion. So, if you value your future self’s ability to recall your grandchildren’s names, you must start treating chronic stress as a medical emergency now, not later. The brain does not forgive neglect, and the cost of inaction is far steeper than any temporary inconvenience.
Cindy Thomas
October 26, 2025 AT 07:43While the data are compelling, it’s worth remembering that stress isn’t a monolith; acute challenges can actually sharpen cognition, whereas the insidious, unrelenting kind does the opposite :). A balanced lifestyle that mixes stress exposure with recovery periods appears to be the sweet spot for neuroprotection.
Kate Marr
October 29, 2025 AT 06:00Our great nation thrives when we protect our brains 🇺🇸🧠. Prioritize exercise, sleep, and community to keep the stress monster at bay 💪.
James Falcone
November 1, 2025 AT 04:16Look, if you want the country to stay strong, you gotta keep your noggin in top shape. Cutting stress out with a quick run or a cold beer isn’t just personal-it’s patriotic.
Frank Diaz
November 4, 2025 AT 02:33One might argue that the modern preoccupation with “stress management” is merely a veneer for deeper existential malaise. The relentless pursuit of productivity masks a collective avoidance of the void, and the brain, being the ultimate repository of meaning, suffers the collateral damage. When cortisol rises, it is not merely a hormone but a symptom of a society that has lost its philosophical anchor. Thus, the solution is not merely yoga mats or treadmill miles, but a re‑examination of purpose itself. Until we confront the emptiness, biochemical cascades will continue to erode the very substrate of consciousness.
Mary Davies
November 7, 2025 AT 00:50Could it be that merely watching the sunrise each day might gently coax the HPA axis back into harmony? The notion feels almost poetic, yet science hints that light exposure regulates cortisol rhythms, offering a subtle, non‑pharmacologic reprieve.
Valerie Vanderghote
November 9, 2025 AT 23:06Honestly, I’m still stunned that people think they can ignore the silent siege their bodies endure. You sit at your desk, scroll endless feeds, and convince yourself that a latte will shield you from all that hormonal havoc-but cortisol doesn’t care about your espresso preferences. It seeps into every synapse, whispering doubts while you’re distracted by memes, and before you know it, the hippocampus is a battlefield. I’ve watched friends binge‑watch series for hours, then complain about memory lapses; the pattern is too clear to dismiss. The best antidote, in my opinion, is a ruthless schedule overhaul: three solid workouts a week, a strict lights‑out hour, and genuine face‑to‑face conversations that demand emotional honesty. If you keep feeding the stress monster with excuses, you’ll only watch it grow, gnawing at the very essence of who you are. So pull the plug on the nonsense, and start treating your brain like the priceless heirloom it truly is.
Michael Dalrymple
November 12, 2025 AT 21:23It is essential to recognize that stress reduction is not a fleeting task but a sustained commitment to cognitive stewardship. By integrating regular aerobic activity, mindful meditation, and robust social networks, one cultivates a neuroprotective milieu conducive to longevity. I encourage you to adopt incremental goals: begin with a thirty‑minute brisk walk thrice weekly, followed by guided breathing exercises. Over time, these practices synergistically attenuate cortisol, fortify hippocampal volume, and diminish inflammatory markers. Such disciplined stewardship of the mind honors both personal well‑being and the broader responsibility we share for societal health.
Emily (Emma) Majerus
November 15, 2025 AT 19:40hey you dont need to be perfect just start small like 10min walk daily it helps a ton
Virginia Dominguez Gonzales
November 18, 2025 AT 17:56Picture your mind as a garden; each moment of calm waters the seedlings of memory, while relentless stress scorches the soil. When you tend to that garden with exercise, mindfulness, and laughter, you not only preserve the blossoms of recall but also invite new possibilities to flourish.
Alexis Howard
November 21, 2025 AT 16:13stress link to alzheimer’s? overhyped no solid proof
Winston Bar
November 24, 2025 AT 14:30Alright folks, let’s cut through the melodrama and face facts: the hype machine loves to spin stress into a villainous boogeyman just because it sells clicks. Sure, cortisol is a hormone and chronic elevation isn’t glamorous, but the causal chain to amyloid plaques is far from airtight. I’ve seen studies cherry‑pick cohorts, ignore confounders, and then parade “significant” p‑values like trophies. Meanwhile, the average person is left with a laundry list of lifestyle tweaks that feel more like corporate wellness propaganda than actionable science. If you truly want to protect your brain, focus on proven basics-balanced nutrition, regular physical activity, and mental stimulation-rather than chasing every new “stress‑blocking” fad that pops up on your feed. Remember, the brain is resilient; it doesn’t crumble at every pressure cooker moment, but it does appreciate a steady, compassionate environment.