Breast cancer — what to watch for and what to do next
About 1 in 8 women in the U.S. will develop invasive breast cancer in their lifetime. That number sounds scary, but knowing the basics makes a huge difference. Here I’ll give clear, practical steps you can use now: how to spot signs early, what screening actually does, how hormones matter, and how to get prescription meds safely if you need them.
Screening and common signs
Screening saves lives. Most guidelines recommend regular mammograms starting around age 40–50 depending on your risk. If you’re younger and have a family history or BRCA mutation, talk to your doctor about earlier screening and MRI. Don’t wait: get a baseline exam and keep track of changes.
What to look for at home: a new lump, thickening in one breast, nipple changes (inversion, discharge), or noticeable skin changes like puckering. Pain alone is rarely the only sign, but any persistent change deserves a checkup. If you find something, call your provider and ask for diagnostic imaging—don’t assume it’s nothing.
Treatment basics, hormones, and medication safety
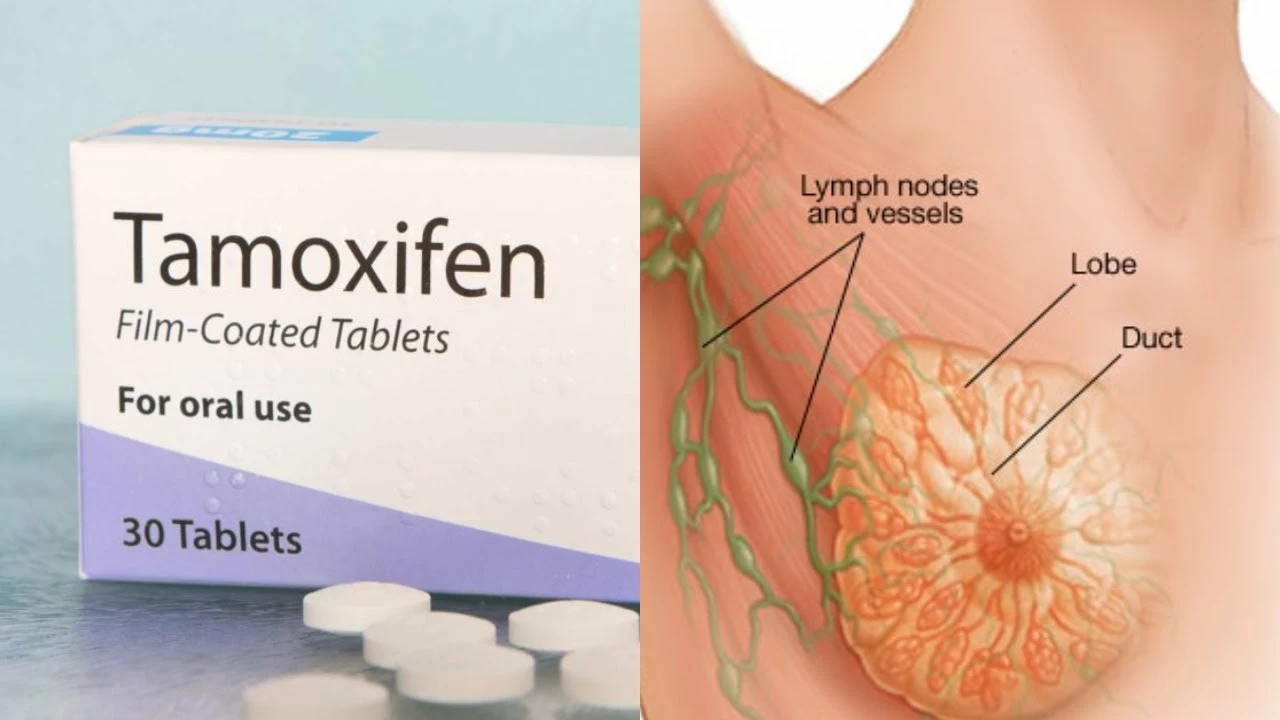
Treatment depends on type and stage. Options include surgery (lumpectomy or mastectomy), radiation, chemo, targeted drugs, and hormone therapy. Hormone-receptor–positive cancers respond to endocrine therapy: tamoxifen for premenopausal women and aromatase inhibitors for postmenopausal women. These drugs lower recurrence risk but have side effects—hot flashes, bone changes, blood clot risks—so discuss trade-offs with your oncologist.
Hormones matter beyond treatment. How your body metabolizes estrogen affects risk; diet, liver health, and certain supplements can change estrogen breakdown. Our article "Estrogen Metabolism Hacks" covers foods and habits that help. If you take supplements or non-prescription remedies, tell your care team—some interact with cancer meds.
If you need prescriptions, be careful when buying online. Use licensed pharmacies, check for contact info, verify prescriptions are required, and avoid sites that sell controlled drugs without a doctor. We have guides on safe online pharmacies and how to spot scams—use them before ordering anything important like endocrine drugs or supportive meds.
Genetic testing can change management. If you have a strong family history or early-onset cancer, ask about BRCA and other gene panels. Positive results change screening schedules and may make preventive surgery or different drug choices worth discussing.
Small lifestyle steps add up: limit alcohol, maintain healthy weight, exercise regularly, and get sleep. These moves won’t prevent every case, but they lower risk and help recovery if cancer appears. And finally, get a second opinion if treatment decisions feel rushed. You deserve clear answers and a plan you trust.
Need more detailed reads? Check our articles on estrogen metabolism, choosing online pharmacies safely, and treatments like tamoxifen. Talk to your doctor, bring questions, and keep records—being proactive gives you the best shot at catching and treating breast cancer early.
Anastrozole vs. Tamoxifen: Which is Better for Breast Cancer Patients?
May 29 2023 / OncologyAs a breast cancer patient, I've been researching the differences between Anastrozole and Tamoxifen to determine which treatment is better. Both are hormonal therapies used to prevent recurrence, but they work in distinct ways. Anastrozole is an aromatase inhibitor, while Tamoxifen is a selective estrogen receptor modulator. Recent studies have shown that Anastrozole may be more effective in reducing recurrence rates, with fewer side effects. However, the choice between these two treatments should be made with the guidance of a healthcare professional, taking into consideration the patient's individual circumstances and preferences.
VIEW MORE