Esophagitis management: practical steps to ease inflammation
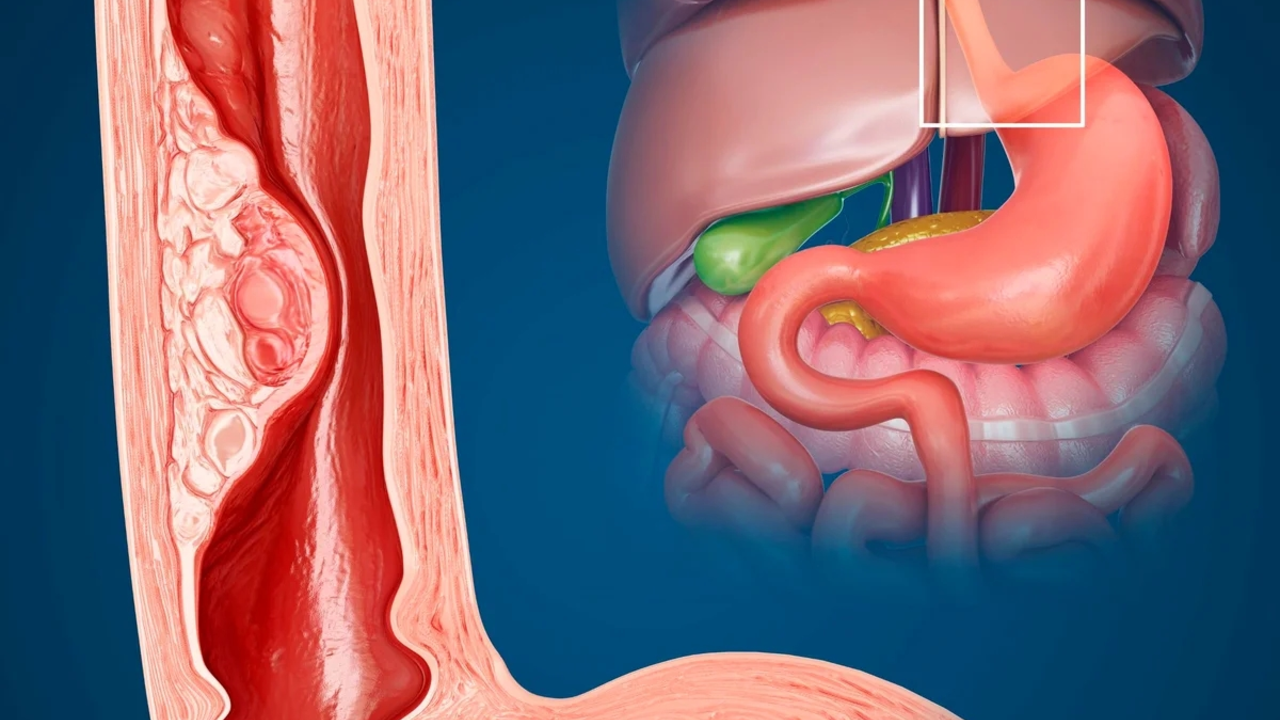
Burning behind the breastbone, pain when you swallow, or food getting stuck — these are the signs many people ignore until they worsen. Esophagitis means the esophagus lining is inflamed. Causes include acid reflux (GERD), infections, medications that irritate the lining, and allergic eosinophilic esophagitis. Management depends on the cause, but you can start helping your esophagus today.
Quick at-home moves that help
First, change what and how you eat. Cut spicy, acidic, and fatty foods that trigger reflux. Skip late-night meals; stop eating two to three hours before bed. Eat smaller portions and chew slowly. Raise the head of your bed 6–8 inches or use a wedge pillow to keep stomach acid down while you sleep. If you smoke, quit — smoking delays healing. Losing even 5-10% of body weight can reduce pressure on the stomach and lower reflux.
Stay upright for at least 30 minutes after meals. Avoid tight clothes that squeeze your abdomen. Swap caffeine and carbonated drinks for water or herbal tea. If you take pills that irritate the esophagus (like some antibiotics, bisphosphonates, or potassium supplements), take them with a full glass of water and remain standing for a few minutes.
Medical treatments and when to see a doctor
If lifestyle tweaks aren’t enough, medications can speed recovery. For acid-related esophagitis, proton pump inhibitors (PPIs) like omeprazole or pantoprazole reduce acid and allow the lining to heal. H2 blockers such as famotidine can help milder cases or be added at night. For suspected infectious causes, doctors may prescribe fluconazole for Candida, acyclovir for HSV, or antivirals for CMV after testing.
Allergic (eosinophilic) esophagitis often needs topical steroids like budesonide slurry and dietary changes guided by an allergist. Severe narrowing (stricture) from long-term inflammation may require endoscopic dilation to widen the esophagus. If you have weight loss, severe pain, inability to swallow liquids, or vomiting, see a doctor quickly — these are warning signs that need urgent evaluation.
Doctors usually confirm the diagnosis with endoscopy and sometimes biopsies to rule out infections, eosinophilic disease, or cancer. Follow-up matters: some people need ongoing PPI therapy, and others require a step-down plan once symptoms improve. Keep a simple diary of foods and symptoms to share with your clinician — it often reveals triggers faster than guessing.
Quick tip: don’t self-prescribe long-term acid suppression without medical advice. PPIs are effective but should be reviewed regularly. With the right mix of diet changes, protective steps, and medical care, most cases of esophagitis improve and pain fades within weeks. If symptoms persist, push for testing — untreated inflammation can lead to scarring and swallowing problems.
Bring a list of medications and a food log to your appointment. Ask your doctor how long you should stay on acid blockers and whether testing for allergies or infections is needed. If you’re prescribed a steroid slurry or antifungal, follow directions exactly. Getting treated early cuts risk of strictures and makes swallowing easier sooner and improves daily comfort.
How to Manage Erosive Esophagitis Symptoms at Work
Jun 28 2023 / Health and WellnessManaging erosive esophagitis symptoms at work can be quite a challenge, but with a few tips, it's doable. First, it's important to stick to a diet that minimizes acid reflux, which means avoiding spicy and fatty foods, and having smaller, more frequent meals. Drinking plenty of water helps too. It's also crucial to take breaks and avoid stressful situations as stress can worsen symptoms. Lastly, always have your prescribed medication on hand and take it as directed by your doctor.
VIEW MORE