Type 2 diabetes: what to watch and what to do every day
If you or someone close to you has type 2 diabetes, you need clear, practical steps — not fluff. This guide explains common signs, how blood sugar is measured, basic medicines, and daily actions that actually help. Read it like a checklist you can use today.
Quick signs, tests, and targets
Common symptoms include frequent urination, thirst, tiredness, slow-healing cuts, and blurred vision. A simple blood test can confirm diabetes: fasting plasma glucose, random glucose, or an A1c (HbA1c). Targets vary by person, but many doctors aim for an A1c under 7% for most adults. If you’re older or have other health issues, your doctor may set a different goal.
Checking your own blood sugar with a meter or continuous glucose monitor (CGM) helps you see how food, activity, and meds affect you. Keep a short daily log: number, time, and what you ate. That small habit gives your doctor useful data fast.
Medication basics and safety
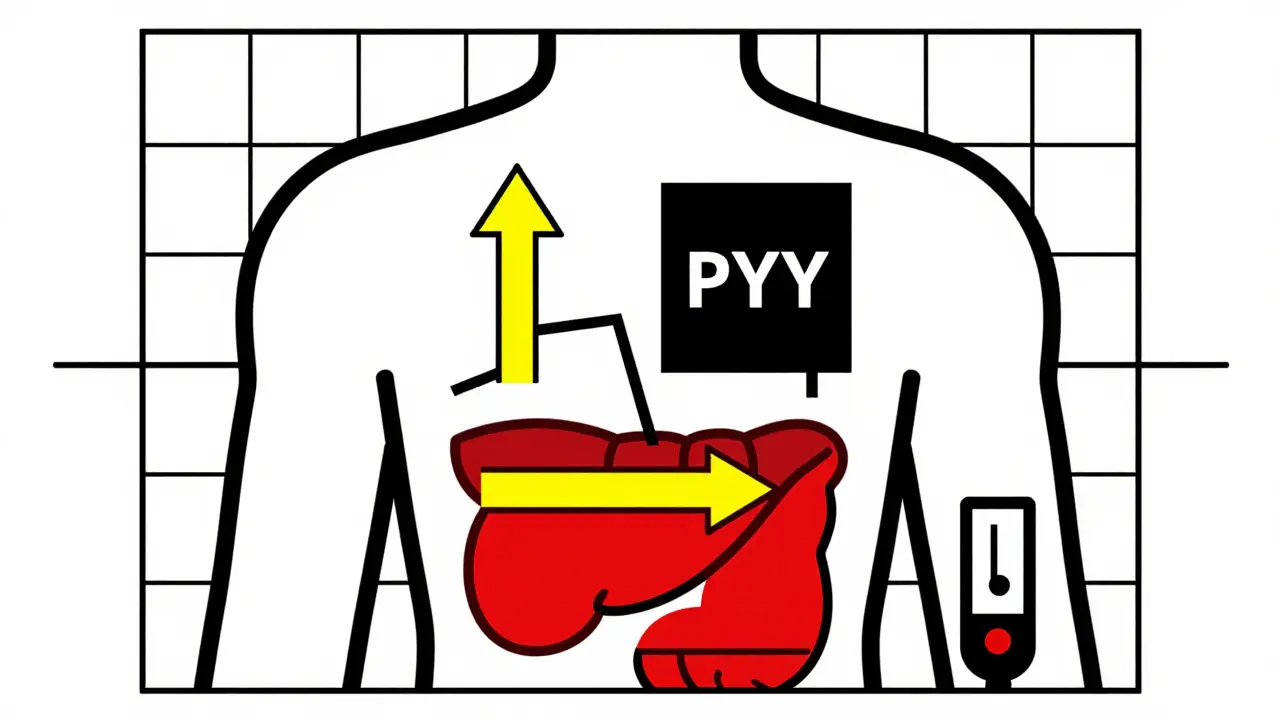
Metformin is usually the first medication doctors try. It lowers liver glucose production and helps insulin work better. If metformin alone isn’t enough, other options include DPP‑4 inhibitors (like sitagliptin), SGLT2 inhibitors, GLP‑1 receptor agonists, and sometimes insulin. Each drug class has benefits and possible side effects; discuss them with your provider.
If you order medication online, be careful. Use pharmacies that require a prescription, show contact details, and have clear reviews or certification. Never buy from sites that skip prescriptions or offer suspiciously low prices — real savings come with verified safety.
Watch for common medication flags: stomach upset with metformin, increased urination with SGLT2 drugs, or low blood sugar if you use insulin or sulfonylureas. Report symptoms promptly and keep an up-to-date list of all medicines for every clinic visit.
Daily habits matter as much as pills. Aim for consistent meals, portion control, and fiber-rich foods. Walk 30 minutes most days — even short brisk walks after meals help lower blood sugar. Losing 5–10% of body weight often improves blood sugar control and reduces medication needs.
Also pay attention to sleep and stress. Poor sleep raises blood sugar; chronic stress can too. Try simple steps: regular sleep times, short breathing breaks, and swapping one sugary drink a day for water or unsweetened tea.
Finally, protect your feet and eyes. Check feet daily for cuts or blisters. Get yearly eye exams and routine blood pressure and cholesterol checks — diabetes affects the whole body. Use these concrete steps with your medical team to stay in control and avoid surprises.
Metabolic Surgery Outcomes: Weight Loss and Diabetes Remission
Feb 10 2026 / Health and WellnessMetabolic surgery offers the most effective path to long-term weight loss and type 2 diabetes remission, outperforming medication and lifestyle changes. Learn who benefits most, how it works, and what to expect after surgery.
VIEW MORE
Exploring 2024 Alternatives to Metformin for Effective Diabetes Management
Oct 28 2024 / MedicationsThis article delves into six alternatives to Metformin, each offering unique benefits for managing Type 2 diabetes. From DPP-4 inhibitors like Januvia to GLP-1 receptor agonists such as Victoza and Ozempic, these medications provide various mechanisms to control blood sugar levels effectively. Additionally, options like Invokana and Jardiance offer the added benefit of promoting weight loss while reducing cardiovascular risks. Glucotrol XL stands out for being cost-effective, although it may lead to hypoglycemia and weight gain.
VIEW MORE