Why Look Beyond Albuterol? Surprising Reasons You Might Need an Alternative
When it comes to asthma, albuterol is the name most people instantly recognize. You’ve probably seen the little blue inhaler peeking out of backpacks, purses, or basketball shorts. It works well for many, but here’s the kicker: it doesn’t work the same for everyone. Some folks build a tolerance, others get jittery or their heart pounds out of their chest, and a few just don’t get the relief they’re hoping for. And get this—using it too often can actually make asthma symptoms worsen over time. No one tells you that in the commercials.
Most doctors say if you’re relying on your rescue inhaler more than twice a week, it’s time to step back and look for options. Don’t wait until you’re stuck wheezing and staring at an empty canister before finding a backup plan. Thankfully, the asthma world isn’t just “one size fits all,” and there’s a real variety when it comes to fast-acting inhalers that can help. Sometimes, finding exactly what works takes a little trial and error—or as my wife Juliana puts it, “the world’s least fun game of roulette.” And believe me, with two asthmatic kids and a pollen count that feels like it’s out to get us, we’ve played.
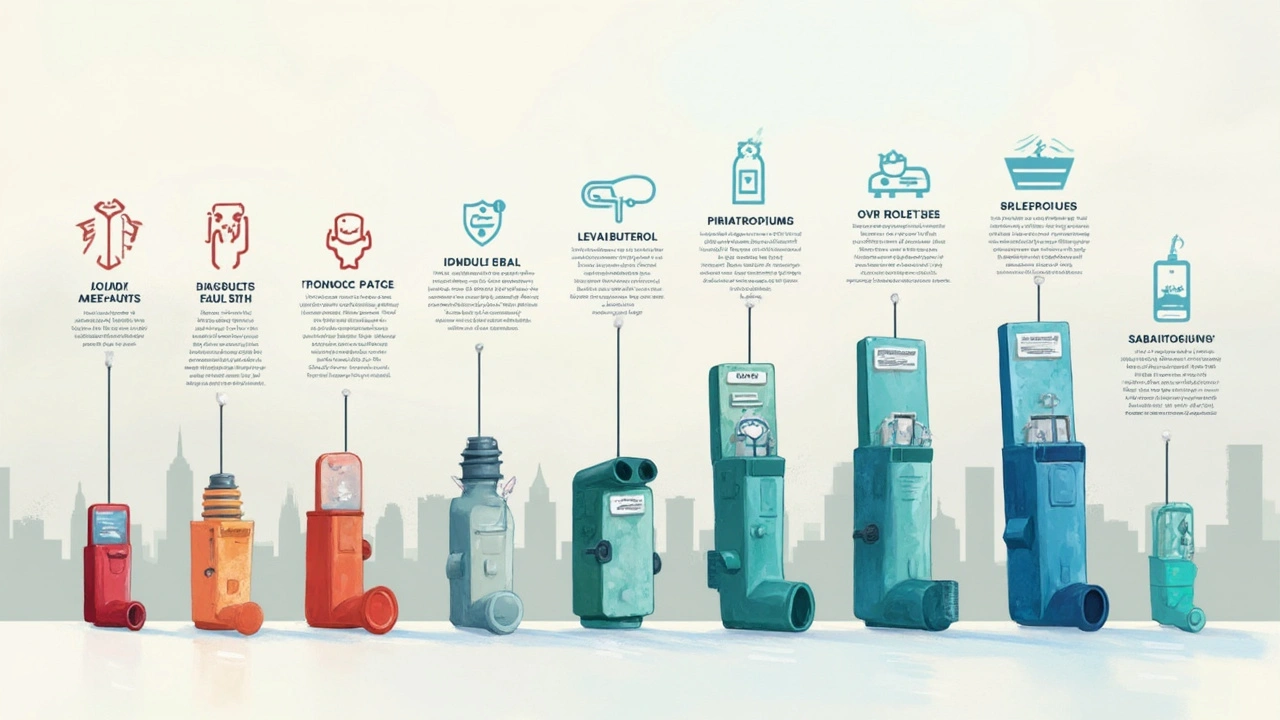
Now, if you’ve ever wondered what’s out there besides Ventolin or ProAir, you’re about to be pleasantly surprised. There are at least eight fast-acting asthma relief inhalers worth knowing, and some come with rare side benefits like fewer jitters or longer-lasting relief. For those times when plain albuterol just doesn’t cut it—or maybe you’re looking to avoid those annoying side effects—the right alternative can save the day. So, let’s get genuinely practical about what’s available and how each one stacks up.
Meet the Challengers: Levalbuterol, Ipratropium, and Pirbuterol Take Center Stage
First up, levalbuterol. It sounds almost identical to albuterol, right? The big difference is in the details. Levalbuterol (brand name Xopenex) is a single-isomer formulation, which means you get the "active" part of albuterol minus some of the stuff your body doesn’t really need. If that sounds geeky, think of it as a more precise tool—it often causes fewer racing heartbeat episodes and less shakiness, especially for kids and older adults. In the ER, docs sometimes switch people to levalbuterol when they complain of feeling too wired after regular albuterol. Anecdotal trick: folks with heart problems tend to do better on it, though always talk to your doctor before substituting. Typical dose? 1-2 puffs every 4-6 hours as needed. Some pharmacies report it’s pricier than albuterol, but insurance coverage is improving.
Now, ipratropium (brand name Atrovent) isn’t your classic “rescue” med—at least, not solo. But in combination with albuterol, it really pulls its weight, especially during severe asthma attacks or those long, nagging coughs that just won’t quit. Ipratropium is actually an anticholinergic drug, so it works a bit differently by relaxing airway muscles and decreasing mucus. In an ER setting, I’ve seen it bring down stubborn symptoms when albuterol alone stalls out. Ever wondered why paramedics sometimes pull out a combo inhaler? That’s why. It’s not usually the first inhaler you get for mild asthma, but when things get rough—think severe attacks or viruses that make breathing a total nightmare—Atrovent can be a game-changer.
Let’s talk about pirbuterol (Maxair). This one’s flown under the radar lately. Pirbuterol is a **SABA**—short-acting beta-agonist—much like albuterol, but some people swear by its smooth, fast kick. It’s delivered by an “autohaler,” so if you’re the type who struggles to remember when to push and when to breathe in, Pirbuterol’s “auto-trigger” does the thinking for you. Unfortunately, Maxair Autohaler disappeared from pharmacies in the US a few years back because of environmental regulations (those CFC propellants got the boot). But in other parts of the world or through specialized suppliers, it can still be found. Don’t count it out if you’ve had luck with it before—it’s worth talking to your doctor about overseas options, especially if nothing else feels right.
Here’s an interesting quick shot: A study in the Journal of Allergy and Clinical Immunology found levalbuterol had a 20% reduction in tremor compared to albuterol, but cost remains a barrier for many families. And ipratropium? It’s especially helpful for asthma triggered by cold air or exercise, so for those chasing after a runaway dog or braving a winter run, it might be the trick that keeps your lungs in the game.
The Power Duos: Exploring SABA-LABA Combos for Fast and Long Relief
Let’s talk combos. SABA-LABA inhalers combine a short-acting beta-agonist (like albuterol) with a long-acting one (like formoterol). These inhalers hit quick to open airways but have some staying power, too—sort of like having both an emergency airbag and shock absorbers in your car. One standout is the formoterol-budesonide combo (Symbicort), now approved in some countries as both a daily controller and a rescue inhaler. If you’re tired of juggling different inhalers for “now” and “later,” these combos bring serious convenience. You use them as needed in a pinch, plus they keep working for hours after, slamming the brakes on late-phase asthma symptoms that often sneak up after the initial attack calms down.
The global GINA asthma guidelines now say that using a SABA-LABA for both rescue and control—the “single maintenance and reliever therapy” (SMART)—can reduce severe asthma attacks by nearly half in certain patients. That’s huge. The only catch: these combos aren’t for everyone. Kids under 12, folks with heart rhythm problems, and those who’ve had bad side effects from steroids need to talk it through with a doctor. Still, if you spend more time counting rescue puffs than sheep at night, SABA-LABA combos might offer the stability you’ve been missing.
Don’t overlook the other pairings either. There’s vilanterol-fluticasone (Breo Ellipta) and salmeterol-fluticasone (Advair), each with their own flavor of fast-and-sustained action. Vilanterol’s unique trick is its once-daily dosing, which means fewer interruptions to your routine. Just make sure you understand which drugs in your inhaler act fast versus which provide long-term protection—it’s easy to get mixed up and overuse the wrong one when symptoms hit.
One pro tip from our family pharmacist: if you ever run out of your classic albuterol inhaler and only have a combo rescue inhaler like Symbicort in hand, know your dose. It’s different from your maintenance dose, so double-check with your healthcare provider or at least keep the instructions tucked in your phone’s favorites.
Going Off the Beaten Path: Uncommon Fast-Acting Inhaler Choices That Work
You may not have heard of these, but terbutaline, fenoterol, and even inhaled magnesium sulfate have carved out space in the asthma toolkit worldwide. Terbutaline (Bricanyl) gets prescribed across Europe and parts of Asia, especially for patients who find albuterol too stimulating. Its main claim to fame? Similar bronchodilation, but fewer side effects in some users. It’s tablet form is helpful for people who struggle to master inhaler technique, which, let’s face it—can be notoriously tricky, especially for younger kids or the elderly.
Fenoterol used to be much more common, but was phased out in some countries after concerns about sudden asthma deaths when overused in the 1990s. It’s still an option in certain places for those who haven’t tolerated other SABAs. This just highlights an important point: even "fast-acting" doesn’t mean “take as much as you want.'' Frequent overuse can make asthma worse and increase risk of a hospital trip. My buddy Chris, who’s spent too many nights in urgent care, now swears by tracking every inhaler puff so he doesn’t overdo it—something his doctor insists on.
Another wild card is nebulized magnesium sulfate. Hospitals sometimes use it in severe asthma attacks that don’t respond to standard inhalers. Studies show it can relax airways and help avoid intubation, but it’s not something you can use at home—instead, think of it as a last line of defense in ER settings. Not exactly convenient, but worth knowing these backup tools exist.
And if you’re searching for a deeper dive, check out this resource for an in-depth breakdown of alternatives to albuterol. It covers even more on options and what doctors think about each, and has some real-world reviews that helped me rethink our own family’s asthma action plan.

The Real-World Angle: Tips, Mistakes, and What Asthma Patients Need to Know
I’ve seen it plenty—people get a prescription, try a new inhaler once, and either write it off or toss it in their drawer. Fast-acting asthma relief isn’t just about the drug, but about using it right. Here’s what I wish everyone knew: inhaler technique matters just as much as the medication inside. Even adults who’ve had asthma since grade school mess it up. A 2023 survey of adults with chronic asthma showed nearly 55% used their inhalers incorrectly, losing almost half the medicine to the air.
If you struggle to time your breath or can’t feel the spray, ask for a spacer. It’s not just for kids—using a spacer can double the amount of medication actually reaching your lungs. And if you’re trying a new inhaler, bring it with you to your next appointment. Practice spraying into the air (not toward your face, trust me on this) while your provider checks your form.
Another real-world tip: track symptoms with a simple phone note or asthma diary. If you need more than two doses a week, or your inhaler lasts less than a month, talk to your doctor. This isn’t about being a “bad patient”—it’s about making sure you don’t miss a better solution that could fit your life and symptoms better.
I’ve learned from Juliana and our crew that sometimes the best fix isn’t what’s most popular, but what fits your specific triggers and habits. Someone who only has flares during cold winter air might find ipratropium crucial, while another person swears by levalbuterol for after-exercise breathing trouble. Don’t let anyone make you feel stuck. The options exist—you just have to speak up and ask for them.
Insurance is its own maze. For people in the States, out-of-pocket costs can be wild—one month, a generic levalbuterol refill is $20, the next it’s $80. There are assistance programs and coupons online that can help. Sometimes pharmacies have discount plans for cash payers, so don’t be shy about asking the counter staff. And if a med isn’t covered, your doctor may have to “prior authorize” it—don’t accept a hard no before double checking.
Here’s a table comparing fast-acting inhaler costs and frequency of side effects, just for context:
| Medication | Estimated Monthly Cost (US) | Common Side Effects (Jitters/Heart) |
|---|---|---|
| Albuterol | $15-50 | High |
| Levalbuterol | $30-90 | Lower |
| Ipratropium | $25-60 | Low |
| Pirbuterol | Varies (Limited US Availability) | Medium |
| SABA-LABA Combo | $60-200 | Medium |
Remember, what works best for your friend or neighbor may not work the same for you—and that's okay. Work closely with your provider, keep an open line with your pharmacist, and don’t give up after one less-than-perfect experience. The best asthma plan is always customized.





Heather Wilkinson
April 30, 2025 AT 03:25Hey everyone! 🌟 If you’re juggling albuterol and looking for smoother options, you’ve come to the right place. I’ve been there, trying to keep my kids’ inhalers stocked without the jitters. Levalbuterol can be a game‑changer for those who feel the usual shake. And don’t forget a spacer – it really helps the medication reach the lungs. Keep a symptom diary; it’s amazing how patterns pop out. 💪
Henry Kim
May 5, 2025 AT 22:18Your points really resonate. I’ve seen how a simple technique tweak can cut down on unnecessary doses. Staying calm and breathing steadily is often underrated.
Neha Bharti
May 11, 2025 AT 17:12Mindfulness of breath mirrors the balance we seek in treatment; a clear mind often leads to clearer lungs.
Samantha Patrick
May 17, 2025 AT 12:05I found that checking the inhaler’s expiration date is key – some of us forget and end up with less med. Also, dont skimp on the spacer, it makes a big diffrence.
Ryan Wilson
May 23, 2025 AT 06:58It’s surprising how many people overlook such basic steps; ignoring device maintenance is practically neglecting your own health. You should really take responsibility and not blame the medicine for side effects that stem from improper use.
EDDY RODRIGUEZ
May 29, 2025 AT 01:52Alright, folks, strap in because the inhaler world isn’t just blue cans and sighs – it’s a battleground of options! From levalbuterol’s precision to ipratropium’s combo power, you’ve got an arsenal at your fingertips. Don’t settle for the first thing that pops out of a pharmacy; explore the lineup and own your breathing!
Christopher Pichler
June 3, 2025 AT 20:45Sure, because everyone loves a new acronym – SABA‑LABA sounds like a secret code for 'let’s confuse patients even more.' Yet the data shows SMART therapy can halve severe attacks, if you can parse the terminology.
VARUN ELATTUVALAPPIL
June 9, 2025 AT 15:38Indeed!!!, the sheer volume of abbreviations-SABA, LABA, SMART, GINA-can be overwhelming; however, it’s precisely these guidelines, meticulously crafted, that empower clinicians, patients, and researchers alike, to navigate the complex pharmacologic landscape, isn’t it?;
April Conley
June 15, 2025 AT 10:32Skip the hype and try a spacer.
Sophie Rabey
June 21, 2025 AT 05:25Oh, absolutely, because a simple spacer magically eliminates all pharmacologic nuances-best‑case scenario, right?
Bruce Heintz
June 27, 2025 AT 00:18Glad you’re all sharing tips! 😊 Remember, consistency with your inhaler technique beats occasional heroics any day.
richard king
July 2, 2025 AT 19:12The theater of respiration is set, and each puff is a dramatic entrance-choose your prop wisely, lest the curtain fall prematurely.
Dalton Hackett
July 8, 2025 AT 14:05When it comes to inhaler technique, the devil truly lies in the details. First, always shake a metered‑dose inhaler for at least five seconds – a shaky hand can waste medication.
Second, exhale fully before you place the mouthpiece, then seal your lips tightly; any leakage means less drug reaches the lungs.
Third, coordinate your breath: inhale slowly over three to five seconds while pressing down the canister. A rapid inhale turns the aerosol into a mist that deposits in the mouth instead of the bronchial tree.
Fourth, hold your breath for about ten seconds after the puff; this pause allows maximal absorption.
Fifth, if you’re using a spacer, give the device a good shake and wait a couple of seconds before inhaling – it helps settle the medication.
Sixth, clean your inhaler and spacer regularly; residue can clog the nozzle and alter dosing.
Seventh, keep a log of each use – a simple phone note can reveal patterns of over‑use before they become dangerous.
Eighth, be aware of cost: generic albuterol may be cheap, but levalbuterol and combo devices can spike your pharmacy bill dramatically.
Ninth, check your insurance each year; many plans renegotiate formularies and a previously covered inhaler might become a copay nightmare.
Tenth, don’t forget to ask your pharmacist about discount cards – they can shave off 30‑40% of the price.
Eleventh, if you feel jittery after a dose, consider a lower‑dose formulation or a different agent like ipratropium, especially if you have a cardiac history.
Twelfth, always have a rescue inhaler on hand, even if you’re on a daily controller – asthma can strike without warning.
Thirteenth, educate family members on how to use your device; in an emergency, they’ll be your lifeline.
Fourteenth, review your action plan with your clinician at least annually – guidelines change and new options appear.
Fifteenth, remember that over‑reliance on any rescue inhaler may indicate uncontrolled asthma; discuss step‑up therapy with your doctor.
Sixteenth, stay calm during attacks – anxiety worsens bronchospasm, so breathing techniques are a valuable adjunct.
In short, mastery of technique, vigilance about cost, and regular professional review are the pillars of effective asthma management.
William Lawrence
July 14, 2025 AT 08:58Really? You think more expensive meds are always better I doubt it but okay
Grace Shaw
July 20, 2025 AT 03:52Dear community members, I would like to extend my sincere appreciation for the diligent discourse surrounding alternative rapid‑acting bronchodilators. It is evident that the nuanced considerations of pharmacokinetic profiles, patient‑specific comorbidities, and socioeconomic factors warrant a comprehensive and methodical approach. Moreover, the recent GINA recommendations underscore the importance of individualized therapy, rather than a one‑size‑fits‑all paradigm. I encourage each of you to continue sharing evidence‑based experiences, as collective wisdom enhances our capacity to tailor treatment plans effectively. Let us remain vigilant in evaluating both efficacy and safety, particularly when navigating newer combination inhalers. Finally, please remember that open communication with healthcare providers is paramount to achieving optimal asthma control.
Sean Powell
July 24, 2025 AT 03:25Your formal note is spot on – we all need that balanced view. Lets keep sharing ideas across cultures & languages, it only makes the convo richer.