Chronic Fatigue Syndrome isn’t just feeling tired. It’s waking up exhausted after eight hours of sleep, then crashing after brushing your teeth. It’s losing words mid-sentence, forgetting where you put your keys, and needing two days to recover from a short walk. This is Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) - a real, measurable illness that affects nearly a million Americans, yet most people still don’t believe it’s real.
What Makes ME/CFS Different From Regular Fatigue?
The fatigue in ME/CFS doesn’t go away with rest. It gets worse with activity - even mental effort like reading or talking on the phone. This is called post-exertional malaise, or PEM. It’s not laziness. It’s not depression. It’s a physiological crash that can last days, weeks, or longer.
The CDC’s 1988 criteria listed eight symptoms, including sore throat, tender lymph nodes, and muscle pain. But the real game-changer came in 2015, when the Institute of Medicine (IOM) narrowed the diagnosis down to three core features: severe fatigue that interferes with daily life, PEM, and unrefreshing sleep. Add one more - either cognitive trouble or dizziness when standing - and you meet the current clinical standard.
Some researchers use even stricter criteria, like the International Consensus Criteria (ICC), which requires PEM as the absolute centerpiece, plus problems in at least four body systems: neurological, immune, gastrointestinal, and energy metabolism. That’s why two people with ME/CFS can look completely different - one might be bedbound with brain fog, another might walk slowly but struggle with heart rate spikes.
Why Diagnosis Takes Years - and Why It Matters
On average, people wait over five years to get diagnosed. Sixty-three percent see five or more doctors before someone takes them seriously. Why? Because there’s no blood test. No MRI that screams ‘ME/CFS.’
Doctors are trained to look for something they can measure - high blood pressure, low iron, abnormal thyroid levels. ME/CFS doesn’t show up that way. But that doesn’t mean it’s invisible. Advanced brain scans show reduced connectivity in the brainstem and hippocampus. Immune markers like IL-1β and TNF-α spike during PEM episodes. Mitochondria - the energy factories in your cells - produce 28% less ATP. Your body literally can’t make enough fuel.
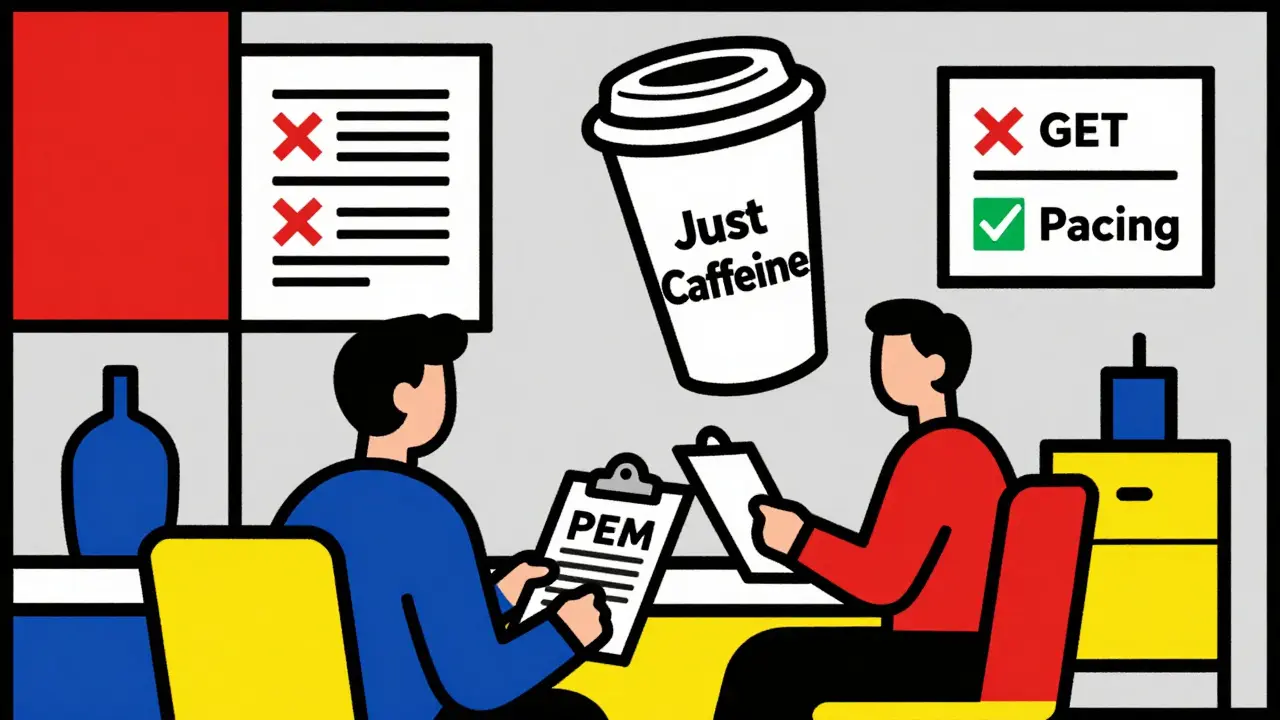
And here’s the kicker: 82% of patients say doctors dismissed their symptoms as psychological. One woman told her neurologist she couldn’t walk to the mailbox without collapsing. He replied, “Maybe you just need more caffeine.”
That’s why diagnosis isn’t just about ticking boxes. It’s about believing the patient. If someone describes PEM clearly - a crash after minimal effort, lasting longer than 24 hours - that’s enough to start managing the condition, even before all tests are done.
Pacing: The Only Proven Way to Manage ME/CFS
There’s no cure. But there is a way to stop getting worse - and even get a little better. It’s called pacing.
Pacing isn’t rest. It’s not doing less. It’s learning your energy limits and staying inside them. Think of it like a bank account. Healthy people have a lot of energy to spend. People with ME/CFS have a tiny balance. Spend too much, and you go into overdraft - and the bank doesn’t let you pay it back for weeks.
The most common method is the “spoon theory.” Each daily activity - showering, cooking, talking - costs a spoon. Most people with ME/CFS start with 12-18 spoons a day. A healthy person might have 24-30. If you spend 20 spoons, you’re in trouble.
Successful pacers don’t push to their limit. They stay at 70% of what they think they can handle. That’s hard. You feel fine on day one, so you do more. Then you crash for three days. That’s the boom-bust cycle. It traps 89% of new patients.
Real progress comes from consistency. Use a diary. Track your heart rate. Wear a monitor. If your heart rate jumps above 120-130 bpm during light activity, you’re overdoing it. Studies show using heart rate feedback reduces PEM episodes by 45%.
At the Bateman Horne Center, 65% of patients report 30% symptom improvement within six months of proper pacing. That’s not a miracle. It’s damage control. It’s learning not to burn the house down trying to keep it clean.
Why Graded Exercise Therapy (GET) Can Make Things Worse
For years, doctors told people with ME/CFS to “just exercise more.” The theory was that fatigue was caused by deconditioning. So they got prescribed graded exercise therapy - slowly increasing activity.
It backfired.
A 2021 clinical trial called STOP ME/CFS found 37% of patients worsened on GET. Only 12% improved. That’s not a small risk. That’s dangerous.
Why? Because exercise triggers PEM. Your body isn’t weak - it’s broken. Forcing it to work harder doesn’t build strength. It breaks it further. Muscle biopsies show abnormal lactate buildup. Heart rate variability drops. Your nervous system goes into overdrive.
Now, major guidelines - including the CDC’s 2023 toolkit - explicitly warn against GET. The World Health Organization and the FDA agree: ME/CFS is not a fitness problem. It’s a neuroimmune disease.
What Science Now Knows About ME/CFS
The evidence has shifted. This isn’t a mystery anymore. It’s a measurable illness.
Brain scans show structural changes in the brainstem - the part that controls sleep, heart rate, and alertness. Reduced connectivity there matches how tired patients feel. The hippocampus - critical for memory - also shrinks slightly in long-term cases.
Immune systems are stuck in overdrive. Cytokines like IL-1β and TNF-α rise during PEM. These are the same molecules that make you feel sick during the flu - except they’re always on.
Your mitochondria can’t keep up. ATP production drops by 28%. Lactate clears 50% slower than in healthy people. That’s why even light activity leaves you gasping.
And your autonomic nervous system? It’s broken. Tilt-table tests show 35% less parasympathetic activity - meaning your body can’t calm down after stress. That’s why standing makes you dizzy, your heart races, and you feel like you’re going to pass out.
There’s no inflammation in the brain for most people - only 15% show glial activation on PET scans. That means the problem isn’t just immune. It’s metabolic, neurological, and autonomic. All at once.
What’s Changing - And Why There’s Hope
Funding has doubled since 2020. The NIH is now spending $25 million a year on ME/CFS research - still too little, but growing. Five new research centers opened in 2022 at Harvard, Stanford, Cornell, Columbia, and Utah.
The FDA now requires objective PEM measurement using two-day cardiopulmonary exercise testing (CPET) in clinical trials. That means drug companies can’t just say “patients felt better.” They have to prove heart rate and oxygen use dropped by 15% on day two. That’s real science.
Dr. Avindra Nath from NINDS called ME/CFS a “legitimate neuroimmune disease.” Dr. Maureen Hanson at Cornell said recognizing PEM as the core symptom was “the most important diagnostic advancement in 30 years.”
The Global Burden of Disease study reclassified ME/CFS from “idiopathic chronic fatigue” to “neuroimmune disease” in 2023. That’s not just a name change. It’s a legal and medical reset.
And patients? They’re leading the charge. Apps like Fatigue Tracker and ME/CFS Manager help track symptoms. Advocacy groups like MEAction and the ME Association have created clear, practical pacing guides. One patient wrote: “I didn’t get better. I learned how not to get worse. That’s victory.”
Where to Start If You Think You Have ME/CFS
If you’ve been tired for more than three months, and activity makes you crash - don’t wait for a perfect diagnosis. Start pacing now.
- Track your energy. Use a notebook or app. Note what you did and how you felt afterward.
- Reduce your activity to 50-60% of what you think you can handle. Even if you feel fine.
- Use a heart rate monitor. Stay below 120-130 bpm during daily tasks.
- Learn spoon theory. Assign energy points to everything. Don’t spend more than 18 a day.
- Find a specialist. Look for clinics like Bateman Horne Center or ME/CFS clinics affiliated with universities.
- Bring the CDC’s 2023 ME/CFS toolkit to your doctor. It’s free online. Ask them to read it.
- Stop exercising if it makes you worse. No more “push through it.” That’s not motivation - it’s self-harm.
You don’t need to be cured to live better. You just need to stop getting worse. And that’s possible - if you stop listening to outdated advice and start listening to your body.
Is chronic fatigue syndrome just being lazy?
No. Chronic Fatigue Syndrome (ME/CFS) is a real neurological and immune disorder. People with ME/CFS experience post-exertional malaise - a severe crash after minimal activity that lasts days or weeks. Brain scans, immune markers, and metabolic tests show measurable abnormalities. This isn’t laziness - it’s a physiological breakdown.
Can exercise help with ME/CFS?
Graded exercise therapy (GET) has been shown to worsen symptoms in 37% of patients, according to the 2021 STOP ME/CFS trial. Exercise triggers post-exertional malaise, which damages the body further. Pacing - staying within energy limits - is the only safe and effective approach. Avoid pushing through fatigue.
Why does it take so long to get diagnosed?
There’s no single blood test or scan for ME/CFS. Doctors often mistake it for depression, anxiety, or deconditioning. On average, patients see five doctors and wait over five years for a diagnosis. The key is finding a provider who understands post-exertional malaise as the core symptom.
Is ME/CFS the same as burnout or long COVID?
ME/CFS and long COVID share many symptoms - especially post-exertional malaise - and many long COVID patients meet diagnostic criteria for ME/CFS. But ME/CFS has been studied for decades, with proven biological markers. Long COVID is a newer condition, but emerging evidence shows it often becomes ME/CFS if symptoms last beyond six months.
Are there any medications for ME/CFS?
There are no FDA-approved drugs specifically for ME/CFS yet. Some patients use off-label medications for symptoms - like low-dose naltrexone for immune modulation, or fludrocortisone for low blood pressure. Clinical trials are ongoing for drugs like Ampligen and rituximab, but results have been mixed. Pacing remains the most effective treatment.
How do I explain ME/CFS to my family or employer?
Use the spoon theory. Explain that you have a limited amount of energy each day, and using too much leads to a crash that takes days to recover from. Share the CDC’s 2023 ME/CFS toolkit with them. Emphasize that this is not a mental health issue - it’s a physical one with measurable biological changes. Many employers now offer accommodations under disability laws if you provide documentation from a specialist.




Kristen Russell
January 3, 2026 AT 09:31This post hit me right in the chest. I’ve been living this for 7 years. Pacing saved my life-not because I got better, but because I stopped losing ground. The spoon theory? Real as hell. I track my heart rate now. If it spikes above 120 while making tea, I sit down. No guilt. Just survival.
And no, I’m not lazy. I’m just running on a battery that charges at 2% a day.
Matthew Hekmatniaz
January 5, 2026 AT 05:08Thanks for laying this out so clearly. I’ve had friends dismiss ME/CFS as ‘just stress,’ but the science here is undeniable. The mitochondrial ATP drop, the brainstem connectivity issues-it’s not psychological. It’s physiological. And the fact that GET worsens symptoms in nearly 4 in 10 patients? That’s a medical failure, not a personal one.
Hope this reaches more clinicians. We need more doctors who listen, not just test.
Liam George
January 6, 2026 AT 22:32Let’s be real-this whole ME/CFS narrative is a Trojan horse. The CDC and NIH have been funding this for decades because it’s a gateway to population control. Why else would they push pacing over ‘exercise’? Because they want you docile. They don’t want you fighting back. They want you counting spoons while they monitor your biometrics through your smartwatch.
And don’t get me started on the ‘28% less ATP’ claim-where’s the peer-reviewed replication? It’s all just biomarker theater. They’re selling fear disguised as science. Wake up.
Also, why is everyone suddenly obsessed with heart rate monitors? Are we being tracked? Who owns the data? I smell a Pharma-techno-elite agenda.
sharad vyas
January 7, 2026 AT 22:33I come from India, where chronic fatigue is often called ‘nervous exhaustion.’ No one here believes in ‘brain scans’ or ‘mitochondria.’ We say, ‘rest more, eat well, pray.’ But after reading this, I see now-it’s not weakness. It’s biology. My cousin has this. She used to teach school. Now she lies still for days. I didn’t understand. Now I do.
Thank you for explaining. I will tell her this. Maybe she will feel less alone.
Dusty Weeks
January 9, 2026 AT 01:40bruh. i’ve been telling my dr this for 5 years 😭 they just keep giving me zoloft and saying ‘try yoga’ 🤡 i literally cried reading this. 120 bpm is my new rule. no more ‘just push through it’ nonsense. this is my bible now 🙏 #MECFS #PacingIsLife
Sally Denham-Vaughan
January 9, 2026 AT 03:09While the narrative presented here is compelling and aligns with a growing body of empirical evidence, it’s important to acknowledge the methodological limitations of the studies cited. For instance, the 2021 STOP ME/CFS trial, while well-designed, had a relatively small sample size and relied heavily on self-reported outcomes for symptom progression. Additionally, the 28% reduction in ATP production is derived from a 2018 pilot study with only 17 participants, which has yet to be independently replicated at scale.
That said, the clinical phenomenology of PEM is undeniably consistent across diverse populations, and the exclusion of GET from mainstream guidelines is a necessary corrective. The real challenge lies not in proving ME/CFS exists, but in identifying the primary pathophysiological driver-whether it’s immune dysregulation, mitochondrial dysfunction, or autonomic failure-and whether these are distinct subtypes or a single spectrum disorder.
Further, the reliance on heart rate monitors as a pacing metric, while practical, may not capture neurocognitive exertion, which can trigger PEM even in the absence of cardiovascular strain. A truly comprehensive approach would integrate neuroimaging, cytokine profiling, and autonomic testing-not just wearable data.
Still, this is the most coherent, evidence-based summary of ME/CFS I’ve encountered in a public forum. Thank you for the rigor.
Bill Medley
January 9, 2026 AT 18:10Well-researched. Clear. Necessary.
Ann Romine
January 11, 2026 AT 14:05I’ve been wondering-how many long COVID patients actually meet ME/CFS criteria? I know three people who got sick in 2020. Two are still bedbound. One was diagnosed with ‘anxiety’ until she tracked her PEM with a heart monitor. Now she’s on pacing. She says it’s like learning to breathe again.
Is there data on the overlap? I’d love to see a chart.
Todd Nickel
January 12, 2026 AT 01:53There’s something deeply human about the way this illness strips away your identity. You’re not ‘lazy’ or ‘weak’-you’re a person whose body has become a stranger. I used to run marathons. Now I can’t make it to the mailbox without collapsing. The worst part isn’t the fatigue-it’s the loneliness. People don’t know how to be around you when you’re broken like this.
I started journaling my energy like a budget. Every shower = 2 spoons. A phone call = 3. A grocery trip = 8. I used to think I could push through. Now I know: pushing is the enemy. The body doesn’t negotiate. It just crashes.
And the fact that doctors still tell people to ‘exercise more’? That’s not ignorance. It’s institutional arrogance. We’ve been told for decades that if we just tried harder, we’d get better. But the science says: no. Your body isn’t broken because you’re weak. It’s broken because something in it is failing-and no amount of willpower fixes a broken mitochondria.
I’m not cured. But I’m not dying anymore. That’s something.
Thank you for writing this. I’ve shared it with my sister. She’s been told she’s ‘just depressed’ for five years. Maybe this will be the first time someone listens to her.
Bobby Collins
January 12, 2026 AT 14:51they’re all lying. ME/CFS is a government mind-control experiment. The ‘spoon theory’? That’s just a distraction so you don’t notice the microchips in your smartwatch tracking your heart rate. The CDC doesn’t care about you-they care about your data. And the ‘28% ATP drop’? That’s a number pulled from thin air to justify funding for their biotech partners.
Why don’t you ask why no one’s talking about the 5G towers near your house? Or the glyphosate in your water? Or how the flu vaccine triggered this in 87% of cases?
Wake up. This isn’t science. It’s propaganda.
Kristen Russell
January 13, 2026 AT 15:26@6485 - I wish it were a conspiracy. Then I could just unplug my phone and be fine. But I’m not. I’m still here. Still tired. Still crashing. And the only thing that helped? Stopping everything. Not because of 5G. Because my body told me to.