You might be surprised to learn that more than three million prescriptions for prednisolone go out each year across Australia, making it one of the most relied-on medications for treating serious inflammation, immune system flare-ups, and loads of other stubborn health conditions. Still, it’s not exactly a drug people chat about at a barbecue. Prednisolone sort of just shows up, does its thing, and slips out quietly—unless you know what to look for. So why is it hiding in plain sight? Let’s pull back the curtain.
What Is Prednisolone and Why Do Doctors Prescribe It?
Prednisolone is a steroid—no, not those muscle-building ones you see in gym scandals, but a synthetic corticosteroid. Its job is to copy your body’s own hormone called cortisol, pumped out by your adrenal glands. When your immune system starts acting up, maybe attacking your own body or going nuts during allergies or asthma, cortisone-based steroids like prednisolone calm everything down.
Doctors turn to prednisolone when they want inflammation slashed fast. We’re talking treatments for asthma, bad allergic reactions, autoimmune diseases (like lupus or Crohn’s), certain cancers, and even some skin flare-ups. In fact, in the emergency room, they reach for ¬prednisolone when someone’s swelling so much it’s dangerous—think severe allergic reactions with swelling throat, wheezy chests, or even brain swelling due to injury.
A quick fact: kids get it a lot for asthma flare-ups or croup. It’s not fun, but it works fast—often cutting recovery times in half. Studies in 2022 showed that in children with croup, a single dose could reduce symptoms within two hours. It’s also a staple for those with autoimmune conditions, making it possible for them to live more normal lives with far less pain. In Australia, prednisolone is available in tablets, syrups, and sometimes as an injectable solution, depending on what needs fixing.
How Prednisolone Works Inside the Body
To get why people swear by (and sometimes curse) prednisolone, you really need to know what’s happening in your body after you take it. Prednisolone grabs onto special receptors in your cells—the same ones natural cortisol uses. When it connects with these, it gives marching orders: “Chill out.”
This makes immune cells less rowdy. They stop spitting out signals that cause swelling, redness, warmth, and pain. Think of it as calling off an overenthusiastic crowd at a football match—nobody gets hurt, the field stays intact. It also muzzles parts of the immune system that can cause allergies or even attack your own tissues. Here’s the flip side: all this calming means your immune system’s defense shield isn’t working at full blast. If you’re around someone with a nasty flu, your body might not have as strong a guard as usual. That’s why doctors keep you on the lowest dose that does the job—any more than you need, and you’re at higher risk of infections.
Prednisolone doesn’t act immediately if you swallow a tablet. It takes about one to two hours to hit peak levels in your blood. But when given by injection (say, in a hospital), it can work much faster. For chronic problems, like certain skin conditions or autoimmune diseases, it’s a long game—you might be on prednisolone for weeks or months, and the dose gets lowered in careful steps to let your body adjust. There’s research out of Monash University showing that the risks of stopping suddenly can be severe—adrenal glands can go on strike, and you get headaches, weakness, and worse. Gradual tapering is key.

Side Effects: What You Need to Watch Out For
No medicine is perfect, and prednisolone is a classic example of a “double-edged sword.” The stuff works wonders, but it doesn’t always play nice, especially if you stick with it for a long time. Here’s where you need to pay attention.
Short-term side effects can sneak up quickly. You might notice your appetite jumps—some people say they’re suddenly hungry enough to eat half the fridge. Other folks find their mood takes a rollercoaster ride, with bursts of energy or irritability. Sleep’s another victim; tossing and turning all night isn’t rare. Liquid prednisolone can taste awful—some hint at a bitter, metallic tang—which makes it rough for kids or anyone with a sensitive palate.
Stick with prednisolone longer, and bigger problems can pop up:
- Weight gain—especially with a rounder face, also called “moon face.”
- Weaker bones (osteoporosis), so falls or knocks could turn into broken bones
- Higher blood sugar levels that some people don’t notice until they develop diabetes
- Blurry vision or even cataracts with extended use
- Thin skin that bruises or cuts easily
- Muscle weakness
- Increased risk of infections, since the immune system is a bit “sleepy”
- In kids, slowed growth if used at high doses for ages
One sneaky side effect? Prednisolone can hold onto salt and water in your body, causing swelling in your feet or ankles, and even raising your blood pressure. If you have a heart condition, this isn’t just uncomfortable—it can be dangerous. People with a history of mental health issues also need to watch for mood swings or agitation.
Here’s a snapshot of the most common side effects and how often they pop up, based on hospital-based studies in Sydney:
| Side Effect | Frequency |
|---|---|
| Increased appetite | Almost everyone on high doses |
| Insomnia | 4 out of 10 adults |
| Weight gain | About 30% |
| Mood disturbance | 20-30% |
| Infections | 10-15% |
| High blood sugar | 15% |
If you notice any weird symptoms while taking prednisolone—especially things like fever, confusion, or vision changes—don’t just wait it out. Talk to your doctor. Catching problems early makes them way easier to handle.
Getting Prednisolone Dose and Timing Right
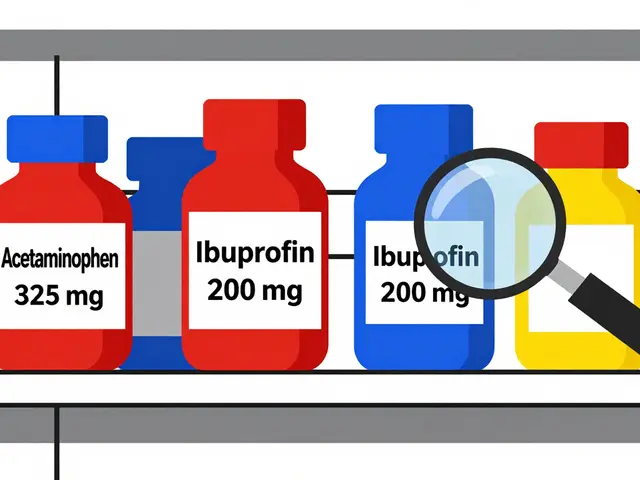
Few things matter as much with prednisolone as how much you take and when. Doctors always aim for the smallest dose that still gets the job done. Too little and your condition flares up. Too much, and you’ll probably get more side effects.
For adults, the range is huge—sometimes just 5mg daily for milder inflammation, but 40mg, 60mg, or even more for emergencies. All depends on what you’re treating. Kids’ doses are based on their weight. If you need to take it for longer than a few weeks, your doctor will taper the dose down slowly. Why? Your adrenal glands need to “wake up” and start making cortisol again. Stopping suddenly can leave you dangerously low on cortisol, which can be life-threatening.
The timing can also make a difference. Taking your dose in the morning means it matches your body’s normal cortisol rhythm, with less risk of insomnia or mood crashes. If you have trouble with the tablet form, there’s liquid or syrup—sometimes easier for kids or adults who struggle swallowing pills. Because prednisolone can upset your stomach, try taking it with food or milk. That simple trick can lower your chance of heartburn or nausea.
Stay in touch with your doctor. Share if you miss a dose, have trouble taking the medicine, or notice side effects. Adjusting the treatment is normal and doesn’t mean you’re failing. If you need vaccines, tell your GP. Some live vaccines aren’t safe while on steroids. Got dental work coming up? Let your dentist know—you heal slower, so infections are riskier now. If you’re traveling, pack extra tablets and a letter from your doctor; border officials or airport staff might check your medication.

Tips for Living Well with Prednisolone
This medicine can be life-changing, but only if you manage it smartly. Here are practical tips I’ve gathered from pharmacists, Aussie doctors, and folks who’ve been through long-term courses.
- Stick to Your Plan: Don’t tinker with your dose solo—even if you feel amazing. Running out suddenly is risky.
- Track Your Moods: Some people get irritable or down on prednisolone. Keep a diary, or ask family to flag changes. If things get rough, don’t hesitate to call your doctor for backup.
- Eat Smart: Go easy on salty foods (like chips, crackers, processed meats)—prednisolone already makes you hold onto salt. Eat fruit, veg, and whole grains to fight weight gain and keep your bones strong. Dairy or calcium-fortified alternatives are a plus to protect against bone thinning.
- Get Moving: Even light exercise, like a daily walk, helps balance the muscle weakness and keeps bones healthy. If you’re often tired, start small and build up.
- Watch Out for Infections: With a dampened immune system, wash your hands more, avoid people who are clearly ill, and don’t skip your flu shot unless your doctor says otherwise.
- Sleep Hygiene: Take prednisolone in the morning if possible; steer clear of caffeine after lunch, and set a steady bedtime—this helps tackle the sleeplessness so common with steroids.
- Sun Safety: Prednisolone thins your skin. Use good sunscreen, even in winter, and cover up if you’re outside for long periods.
- Bone Checks: If you’re on prednisolone for more than a few months, ask your doctor about a DEXA scan (a bone density test). These scans are available across major hospitals in Sydney and recommended if you’re over 50 or have broken a bone before.
- Chat to Your Pharmacist: They can give you tips on swallowing tablets, spacing doses, and what to do if you’re ever sick and can’t take the medicine orally.
Some folks wear a medical alert bracelet that says they’re on long-term steroids. In an emergency, this alerts ambulance or hospital staff, so they know your body might not react to stress or infections in the usual way.
There’s no shame in asking questions or setting your own boundaries. Every person’s response to prednisolone is different. Don’t compare yourself too harshly to anyone else, whether it’s your mate or a patient you read about online.
To wrap up, prednisolone is one of the real workhorses of modern medicine. It’s sharp, powerful, and surprisingly common. If you know how it ticks, stay on top of your health, and play it smart with food, activity, and checkups, prednisolone can get your symptoms under control and give you the breathing room you need—even if that means a few more doctor visits or a trickier grocery list. So next time you see that tiny tablet, remember: there’s a lot of science (and a bit of risk) packed inside. Use it with respect, and it just might change your life for the better.



Rafael Lopez
May 30, 2025 AT 00:16When you’re prescribed prednisolone, the first step is to confirm the exact milligram strength; never guess the dose, and always read the label carefully, because a 5 mg tablet is not interchangeable with a 20 mg tablet; take the medication in the morning, ideally with food, to mimic the body’s natural cortisol rhythm; if you miss a dose, take it as soon as you remember unless it’s almost time for the next dose, in which case skip the missed one-do not double‑up; monitor your blood sugar and blood pressure regularly, especially if you have a history of diabetes or hypertension; keep a short diary of any mood changes, appetite spikes, or sleep disturbances, and bring this record to every follow‑up appointment; and finally, never stop the drug abruptly-tapering under a doctor’s supervision is essential to avoid adrenal insufficiency.
Craig Mascarenhas
June 6, 2025 AT 22:16It is clear that big pharma pushes prednisolone without telling you the hidden agenda it carries in your body they want you dependent on cheap steroids while the side effects pile up unnoticed we must stay vigilant and question every prescription
aarsha jayan
June 14, 2025 AT 20:16Hey folks, imagine your body as a bustling marketplace and prednisolone as the calm mediator that steps in when the stalls start shouting-its gentle hand can soothe the chaos of inflammation, letting you breathe easier and smile brighter; think of it as a rainbow after a storm, a vivid reminder that science can be both powerful and compassionate.
Rita Joseph
June 22, 2025 AT 18:16One practical tip is to pair your prednisolone course with calcium‑rich foods like yoghurt, broccoli, or fortified almond milk; this helps counteract the bone‑weakening risk, especially if you’re on the drug for several weeks; also, stay hydrated and aim for at least 30 minutes of light activity each day to keep muscles strong and mood steady.
abhi sharma
June 30, 2025 AT 16:16Great, another steroid that makes you gain a sausage belly.
mas aly
July 8, 2025 AT 14:16I hear you, dealing with nightly insomnia from a morning dose can feel like a betrayal from your own body; try shifting the pill to mid‑morning with a solid breakfast and see if the sleep improves, and remember to check in with your GP before making any changes.
Abhishek Vora
July 16, 2025 AT 12:16While many patients focus solely on the immediate anti‑inflammatory benefits of prednisolone, it is crucial to recognize the endocrinological cascade that ensues; the suppression of the hypothalamic‑pituitary‑adrenal axis is not merely a side effect but a profound physiological alteration that demands careful tapering; neglecting this can precipitate adrenal crisis, a potentially fatal event; therefore, a structured reduction schedule, monitored by endocrine specialists, is indispensable.
maurice screti
July 24, 2025 AT 10:16Prednisolone, in the grand tapestry of pharmacological interventions, occupies a niche that is both celebrated and reviled.
Its synthetic elegance mirrors the endogenous cortisol, offering rapid attenuation of inflammatory cascades that would otherwise rend tissues.
Yet, the very potency that renders it indispensable also begets a litany of iatrogenic sequelae that the lay public scarcely imagines.
From the subtle insidiousness of insomniac nights to the flamboyant emergence of moon‑face, the spectrum of side effects is as diverse as it is disconcerting.
Medical practitioners, in their benevolent haste to quell acute exacerbations, sometimes overlook the necessity of patient education regarding these risks.
A thorough discussion, replete with dosage charts, tapering protocols, and lifestyle adjustments, is not a mere formality but an ethical imperative.
Consider, for instance, the calcium metabolism derangement; without prophylactic supplementation, the patient may embark upon a silent trajectory toward osteoporosis.
Moreover, the glucocorticoid‑induced hyperglycemia can masquerade as type‑2 diabetes, complicating the clinical picture.
The immunosuppressive veil cast by prednisolone predisposes individuals to opportunistic infections that would otherwise be vanquished by a robust immune response.
One cannot ignore the psychological dimension-mood swings, irritability, and even psychosis have been documented in susceptible cohorts.
Hence, a multidisciplinary approach, enlisting endocrinologists, nutritionists, and mental health professionals, often yields the most favorable outcomes.
Patients are advised to maintain a daily log, noting not only physical symptoms but also emotional fluctuations.
Such diligent record‑keeping furnishes clinicians with the granular data required to fine‑tune dosages.
In the realm of long‑term therapy, periodic bone density scans and ophthalmologic examinations become non‑negotiable safeguards.
Ultimately, prednisolone is a double‑edged sword, wielded with precision it can restore quality of life; wielded recklessly, it may erode the very health it seeks to preserve.
Abigail Adams
August 1, 2025 AT 08:16It is astonishing how readily clinicians prescribe prednisolone without a rigorous assessment of the patient’s baseline risk factors; such cavalier prescribing betrays a profound lack of prudence that undermines the therapeutic relationship.
Belle Koschier
August 9, 2025 AT 06:16I understand the concern raised, but let’s remember that prednisolone can be life‑saving when used correctly; open dialogue between doctor and patient, coupled with careful monitoring, usually mitigates the risks mentioned.
Allison Song
August 17, 2025 AT 04:16Medicine, in many ways, reflects the balance between intervention and natural healing; when a tool like prednisolone is introduced, it reshapes that equilibrium, prompting us to reconsider the definitions of health and necessary compromise.
Joseph Bowman
August 25, 2025 AT 02:16Interesting point about the pharma push, but have you considered that the very institutions promoting prednisolone may be part of a larger agenda to keep us dependent on synthetic solutions, subtly steering public health policy away from holistic approaches?