The U.S. Food and Drug Administration (FDA) doesn’t just approve generic drugs and walk away. Once a generic medication hits the market, its safety journey is just beginning. With nearly 90% of all prescriptions filled in the U.S. being generics, the stakes couldn’t be higher. These drugs are cheaper, widely used, and often taken daily by millions - so even rare side effects can add up. The FDA’s job after approval is to watch for problems that didn’t show up in clinical trials. And they’ve built a system to do exactly that.
How Generics Are Approved - And Why That’s Not Enough
Before a generic drug gets approved, it must prove it’s bioequivalent to the brand-name version. That means it delivers the same active ingredient at the same rate and amount in the body. These studies usually involve 24 to 36 healthy volunteers. That’s not enough to catch every possible reaction. Real people have different health conditions, take other medications, or react differently because of genetics, age, or liver function. A side effect that shows up in one in 10,000 users won’t be seen in a trial of 30 people. That’s why the FDA knows: approval doesn’t mean safety is fully known.The Systems Behind the Scenes
The FDA doesn’t rely on guesswork. It uses real data from real people. The main tool is the FDA Adverse Event Reporting System (FAERS) - a massive database that collects reports of side effects, overdoses, and medication errors. In 2022 alone, FAERS processed over 2 million reports. These come from doctors, pharmacists, patients, and drugmakers. A team of epidemiologists, pharmacists, and data scientists in the FDA’s Office of Surveillance and Epidemiology reviews every report flagged as unusual. But FAERS is passive. It waits for someone to report a problem. To get ahead of issues, the FDA also runs the Sentinel Initiative. This system taps into electronic health records from over 100 million patients across hospitals, clinics, and insurers. Instead of waiting for reports, Sentinel actively scans for patterns - like a sudden spike in kidney injuries linked to a specific generic blood pressure pill. It’s like having a national early-warning system.Manufacturing Quality Isn’t Optional
A drug can be bioequivalent but still be unsafe if it’s made poorly. The FDA inspects factories - both in the U.S. and overseas - to make sure they follow Current Good Manufacturing Practices (cGMP). In 2022, inspectors conducted about 1,200 domestic and 600 foreign inspections. They don’t just check paperwork. They look at how raw materials are stored, how batches are mixed, and whether contamination is controlled. One bad batch can affect thousands of pills. That’s why unannounced inspections happen. A plant in India or China might be inspected one month and then again six months later without warning. The Office of Pharmaceutical Quality (OPQ) also reviews impurities - chemical byproducts that can form during manufacturing. Even tiny amounts of certain impurities can be toxic over time. The FDA sets strict limits based on long-term studies. If a generic manufacturer’s impurity levels exceed those limits, the FDA can block the drug or demand changes.
What Happens When Something Goes Wrong?
When a safety signal pops up - whether from FAERS, Sentinel, or a complaint from a doctor - the FDA doesn’t panic. They investigate. The Office of Generic Drugs (OGD) forms a special team including scientists, clinicians, and chemists. They look at all the data: how many reports, how severe, how consistent. They check if it’s isolated to one manufacturer or affects all versions of the drug. If they confirm a risk, they have tools:- Label updates: Adding new warnings about risks like liver damage or allergic reactions.
- Dear Healthcare Provider letters: Direct emails or notices to doctors about specific concerns.
- Voluntary recalls: The company pulls the batch off shelves.
- Market withdrawal: Rare, but happens if the drug’s risks outweigh its benefits.
Why This Matters More Than You Think
Generic drugs save the U.S. healthcare system over $1 trillion every decade. But they’re not all the same. The top 10 companies control 65% of the U.S. market. That means if one manufacturer cuts corners, it could affect millions. The FDA’s system is built to catch those risks before they become epidemics. Complex generics - like inhalers, patches, or injectables - are harder to copy exactly. Their safety depends on how the drug is delivered, not just how much is in the pill. The FDA has ramped up monitoring for these since 2022 under GDUFA III, the latest funding and oversight agreement with drugmakers. These fees, which brought in $65.7 million annually, help fund the surveillance teams.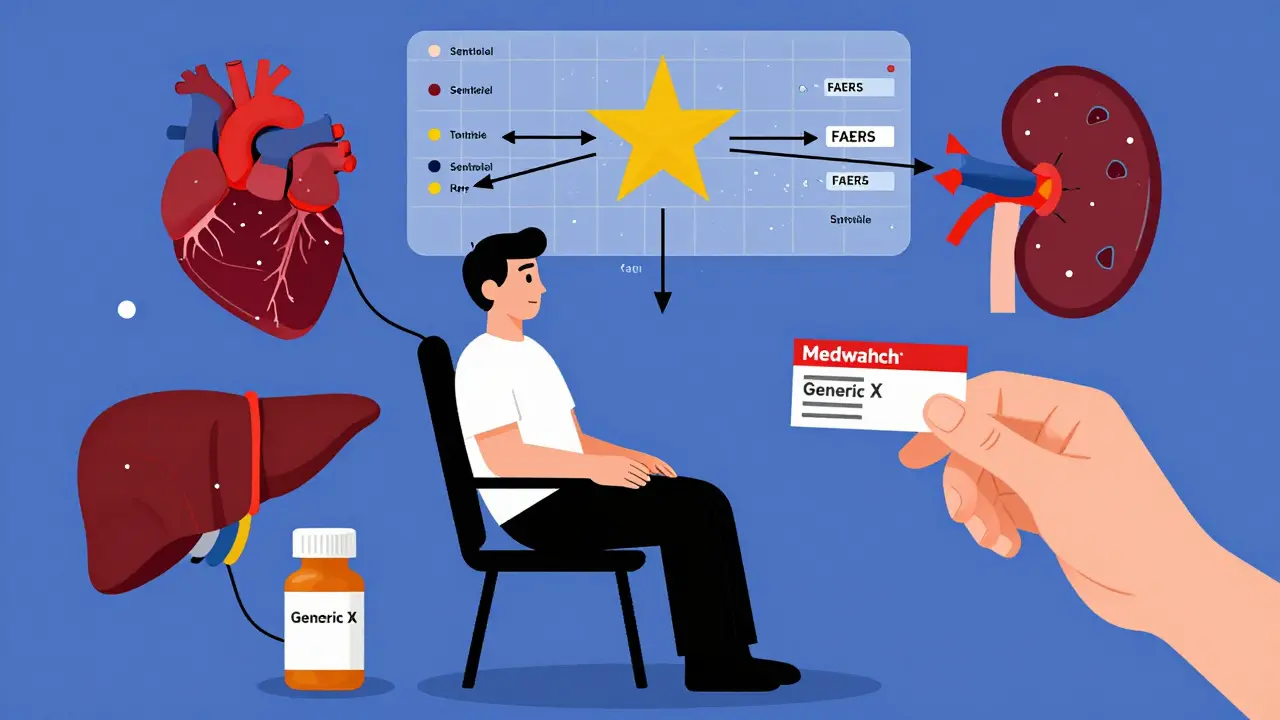
Where the System Still Falls Short
No system is perfect. Experts point to two big gaps: First, underreporting. Studies suggest only 1% to 10% of adverse events are ever reported. Most patients don’t know how to report. Doctors are busy. That means the FDA might miss early warning signs. Second, therapeutic equivalence. Two generics can be bioequivalent but behave differently in certain patients - especially those with kidney disease or on multiple medications. The FDA can’t test every combination. They rely on post-market data, which takes time to accumulate. Still, the system has improved dramatically since the 1990s. Before 2012, there was no dedicated funding or structure for generic drug safety. Now, it’s a full-time mission with dedicated teams, advanced data tools, and clear authority.What You Can Do
If you take a generic drug and notice something unusual - dizziness, rash, nausea, or a change in how you feel - talk to your doctor. Then report it. You can file a report through the FDA’s MedWatch portal. It takes five minutes. Your report might be the one that triggers a safety review. Also, know your drug. If you switch from one generic to another and feel different, tell your pharmacist. Not all generics are identical in how they’re made - even if they’re labeled the same.What’s Next
By 2025, the Sentinel Initiative aims to cover 100 million patients - nearly one-third of the U.S. population. The FDA is also testing artificial intelligence to spot patterns faster. They’re working with tech companies to analyze real-time data from wearable devices and pharmacy records. The goal isn’t perfection. It’s prevention. Every year, thousands of people avoid serious harm because someone noticed a pattern, reported it, and the FDA acted.Are generic drugs as safe as brand-name drugs?
Yes - when they’re made correctly. The FDA requires generics to meet the same standards for quality, purity, and strength as brand-name drugs. The main difference is in inactive ingredients, which rarely cause issues. Post-market monitoring ensures any problems are caught quickly. Studies show generic drugs perform just as well and are just as safe as their brand-name counterparts.
Can I trust generics made overseas?
The FDA inspects foreign manufacturing plants just like U.S. ones. In fact, over half of all generic drugs sold in the U.S. are made overseas, mostly in India and China. The FDA conducts about 600 inspections a year in foreign facilities. If a plant fails inspection, the FDA can block imports. You’re not taking a risk just because the drug was made abroad.
Why do I feel different when I switch generics?
Even though two generics have the same active ingredient, their inactive ingredients - like fillers, dyes, or coatings - can vary. For most people, this doesn’t matter. But for those with sensitivities, or those taking drugs with narrow therapeutic windows (like thyroid meds or blood thinners), small differences can affect how the drug is absorbed. If you notice a change in how you feel after switching, tell your doctor and pharmacist. You may be able to stick with one brand of generic.
How does the FDA decide which generics to monitor more closely?
The FDA prioritizes drugs that are taken by large numbers of people, have narrow therapeutic windows (small differences in dose can cause harm), or are linked to recent reports of side effects. They also watch generics that are newly approved or made by manufacturers with past compliance issues. Complex formulations - like extended-release pills or inhalers - get extra attention because they’re harder to copy exactly.
What’s the difference between FAERS and Sentinel?
FAERS is a database of voluntary reports - doctors, patients, or companies submit side effect reports. Sentinel is an active surveillance system that scans electronic health records from millions of patients to find patterns automatically. FAERS tells you what people report. Sentinel tells you what’s actually happening in real time across healthcare systems. Together, they give a fuller picture.
Drug safety doesn’t end at approval. It’s a continuous watch. And for the millions of Americans who rely on affordable generics, that watch is more important than ever.