Getting your medication right isn’t just about taking it - it’s about taking it correctly, consistently, and on time. For people managing asthma, COPD, diabetes, or chronic pain, inhalers, patches, and injectables are lifelines. But here’s the hard truth: nearly half of all patients don’t use them as prescribed. That’s not laziness. It’s not ignorance. It’s usually a mix of confusion, discomfort, cost, or just plain forgetfulness.
Take inhalers. Many people think they’re using them right - until a doctor checks. Studies show up to 70% of asthma and COPD patients use their inhalers incorrectly. They don’t hold it right, don’t breathe in deep enough, or skip doses when they feel fine. Patches? Skin irritation, forgetting to change them, or removing them too early kills their effectiveness. Injectables? Fear of needles, complex dosing, or apps that crash make people stop.
The good news? There are real, proven ways to fix this. Not just fancy gadgets - but smart, simple, human-centered strategies that actually work.
Why Adherence Matters More Than You Think
Skipping a dose of your inhaler might seem harmless. But over weeks and months, it adds up. Poor adherence is linked to more ER visits, hospital stays, and even early death. In the U.S. alone, non-adherence causes about 125,000 deaths each year and costs the system between $100 billion and $289 billion. That’s not just a number - it’s people. Your neighbor. Your parent. Maybe you.
For inhalers, poor use means uncontrolled asthma. For patches, it’s unstable blood sugar or pain levels. For injectables like insulin or biologics, missed doses can trigger dangerous complications. The goal isn’t just to take the medicine - it’s to get the full benefit. And that only happens when you use it right, every time.
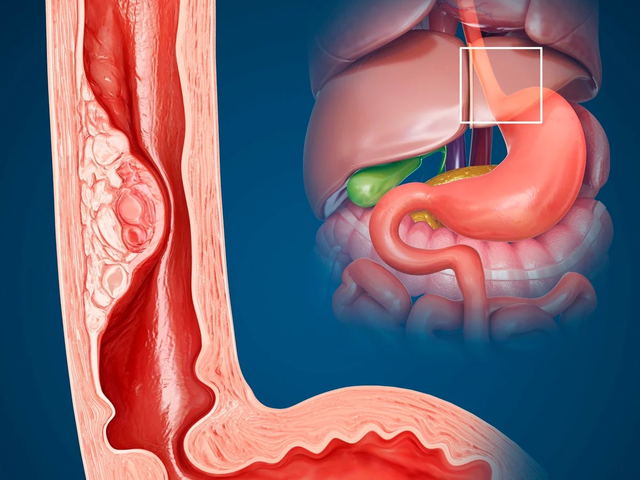
Fixing Inhaler Use: Technique Matters More Than Frequency
Most people think the problem with inhalers is forgetting. It’s not. The real issue is technique. A 2021 study found that 40% of patients who thought they were using their inhaler correctly were actually doing it wrong. They didn’t coordinate the press-and-breathe timing. They didn’t hold their breath after inhaling. They didn’t rinse their mouth after steroid inhalers.
Here’s what actually helps:
- Get a demonstration - twice. Ask your pharmacist or nurse to show you how to use it. Then ask them to watch you do it. Do this again in a month. Technique slips fast.
- Use a spacer. If you’re using a metered-dose inhaler (MDI), a spacer (a plastic tube that attaches to the inhaler) makes it way easier. It holds the puff so you don’t have to time it perfectly. Even better - it reduces throat irritation.
- Try a smart inhaler. Devices like Propeller Health or Teva’s AirDuo RespiClick attach a tiny sensor to your inhaler. It tracks when and how often you use it, and sends reminders to your phone. In trials, users improved adherence by 35%. But here’s the catch: 20% of people stop using them after 6 months because the app glitches or the reminders feel nagging.
- Set a daily habit. Link inhaler use to something you already do - brushing your teeth, eating breakfast, or turning off the lights. Habit stacking works better than alarms.
One user on Reddit said, “I used to miss doses all the time. Now I use my inhaler right after I brush my teeth. I haven’t missed one in 8 months.” Simple. But powerful.
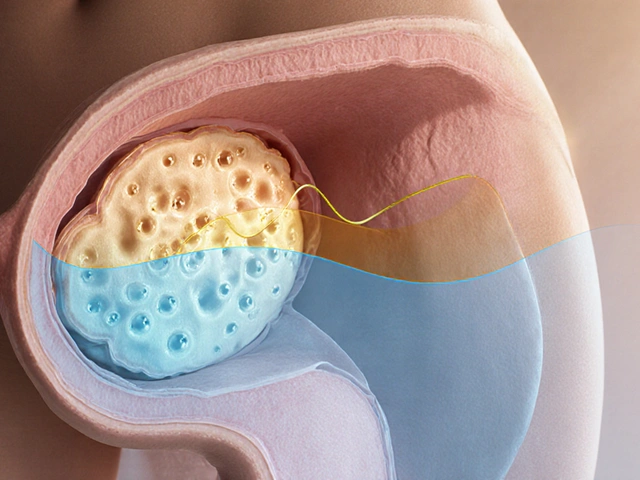
Improving Patch Adherence: Skin, Schedule, and Simplicity
Patches are supposed to be easy. Stick it on, forget it. But they’re trickier than they look. Skin irritation, peeling, sweating, or just forgetting to change it every 1-7 days (depending on the patch) breaks the chain.
Here’s how to make patches stick - literally and figuratively:
- Rotate application sites. Don’t put the patch on the same spot every time. Use your upper arm, back, or thigh - rotate weekly. This reduces skin redness and itching.
- Use adhesive aids. If your patch falls off, try medical-grade adhesive sprays or transparent film dressings (like Tegaderm). They’re cheap, available at pharmacies, and help patches stay on through showers and sweat.
- Set a calendar alert. Patch changes need to be timed. If you change it every Monday and Thursday, set a recurring phone reminder. Don’t rely on memory.
- Try extended-release versions. If you’re on a daily patch and struggling, ask your doctor about a weekly version. For example, some pain patches now last 7 days. Fewer changes = fewer chances to mess up.
- Check for skin reactions. If your skin burns, itches, or peels, don’t just power through. Talk to your doctor. You might need a different patch or a topical cream to soothe the area.
A 2022 survey found that 73% of insulin patch users liked how discreet they were. But 31% stopped using them because of skin problems. That’s fixable - with the right prep and communication with your care team.
Mastering Injectables: From Fear to Routine
Injectables - insulin, biologics, or hormone therapies - are often the hardest to stick with. Fear of needles, pain, complex dosing, or confusing apps make people avoid them.
Here’s what works:
- Use smart pens. Novo Nordisk’s connected insulin pens track every injection - time, dose, location. They sync with an app and send alerts if you miss a dose. In studies, users improved dose accuracy by 27%. But 22% of older users found the app too complicated. If you’re not tech-savvy, ask for a simpler version or use the pen without the app - it still records data internally.
- Practice with a trainer. Many manufacturers give free training pens that don’t contain medicine. Use them to get comfortable with the click, the pinch, the push. It reduces anxiety.
- Store them right. Some injectables need refrigeration. Keep them in a labeled container in the fridge with a note: “Insulin - Do Not Throw Out.”
- Link to a routine. Like inhalers, tie your injection to a daily habit. Morning coffee? After dinner? Pick one and stick to it.
- Ask about long-acting options. If you’re on daily injections, ask if a weekly or monthly version is available. For example, some diabetes meds now last a month. Fewer shots = better adherence.
One patient said, “I used to dread my insulin shots. Then I started doing them while watching my favorite show. Now it’s just part of the evening. I don’t even think about it anymore.”
Technology Can Help - But It’s Not a Magic Fix
Smart devices are everywhere now. Sensors in inhalers. Ingestible chips in pills. Connected pens. They sound like sci-fi. And they do help - but not for everyone.
Here’s the reality:
- They work best when paired with human support. A 2023 study found that patients who got both a smart inhaler AND a pharmacist check-in every two weeks had 40% better adherence than those who got the device alone.
- They’re expensive. A smart inhaler sensor costs $100-$300 a year. Insurance rarely covers it unless you’re in a Medicare Advantage plan - and even then, only 29% of those plans do.
- They can lie. A smart inhaler tracks when you press the button. But it can’t tell if you actually inhaled the medicine. One expert says these devices overestimate true adherence by 15-20%.
- They can stress you out. Constant reminders can make people anxious. One user said, “The app kept buzzing. I felt like I was being monitored. I turned it off.”
Technology should support - not replace - human connection. Use it as a tool, not a prison.
The Real Secret: Personalized Support
The most effective way to improve adherence isn’t an app. It’s not a sensor. It’s a conversation.
Dr. Richard B. Martinello from Yale says adherence has five parts: affordability, accessibility, acceptability, awareness, and activation. That means:
- Affordability: Can you pay for it? Ask about generics, patient assistance programs, or mail-order pharmacies.
- Accessibility: Can you get it? Is the pharmacy close? Can you refill without a 3-day wait?
- Acceptability: Do you hate the way it feels? The smell? The needle? Talk to your doctor. There might be alternatives.
- Awareness: Do you understand why it matters? A simple 10-minute chat with a pharmacist can double your knowledge.
- Activation: Do you feel in control? Or like you’re just following orders? People who feel like they’re part of the decision stick better.
Pharmacists are your secret weapon. Most don’t realize how much they can help. Book a 20-minute appointment. Bring your inhaler, patch, or pen. Ask: “Am I using this right? What’s the easiest way to remember? Is there a cheaper option?”

What to Do Right Now
You don’t need a fancy gadget or a big change. Start small:
- Check your technique. Ask your pharmacist to watch you use your inhaler or injectable today. No judgment. Just help.
- Set one reminder. Use your phone’s alarm for your next patch change or injection. Label it: “Insulin - 7 PM.”
- Write down one barrier. Is it cost? Fear? Forgetfulness? Write it down. Then ask your doctor: “What can we do about this?”
- Try a spacer. If you use an inhaler, get a plastic spacer. It’s $10 at any pharmacy. It makes a huge difference.
- Ask about long-acting options. If you’re on daily meds, ask if a weekly or monthly version exists. Fewer doses = fewer chances to fail.
Improving adherence isn’t about being perfect. It’s about being consistent. One missed dose won’t break you. But a pattern of missing doses? That’s what leads to hospital beds and worse outcomes.
You’re not failing. Your system is. And you deserve better - not just more pills, but better support, better tools, and better care.
Frequently Asked Questions
Why do I keep forgetting to use my inhaler even though I know it’s important?
Forgetting isn’t about laziness - it’s about how your brain works. If taking your inhaler isn’t tied to a daily habit (like brushing your teeth or eating breakfast), your brain doesn’t treat it as automatic. Try linking it to something you already do every day. Also, use a simple phone alarm with a clear label like “Inhaler - Morning.” Don’t rely on memory. Set it, and trust it.
Are smart inhalers worth the cost?
They can be - if you’re someone who struggles with consistency and likes data. Studies show they improve adherence by 30-35% in people with asthma or COPD. But they’re not magic. If you don’t check the app or get support from your care team, you’ll likely stop using it after a few months. The cost is $100-$300 a year, and insurance rarely covers it. Ask your pharmacist: “Is there a cheaper way to track my use?” Sometimes a simple pillbox with dates works just as well.
My patch keeps falling off. What can I do?
First, rotate where you apply it - upper arm, back, thigh - every time. Clean the skin with water and let it dry completely before sticking it on. If it still peels, try a medical adhesive spray or clear film dressing (like Tegaderm) from the pharmacy. These are cheap and help patches stay on through showers and sweat. If irritation keeps happening, ask your doctor about a different patch type or a cream to soothe your skin.
I’m scared of injecting myself. How do I get over it?
It’s normal. Many people feel this way. Start by practicing with a trainer pen - most manufacturers give them for free. Practice on an orange or a piece of fruit. Then, try it in front of a mirror. Use a numbing cream (like EMLA) 30 minutes before if the skin is sensitive. Most importantly, tie the injection to something calm - like listening to music or watching a show. You’re not just giving yourself a shot. You’re taking control of your health.
Can my doctor tell if I’m not taking my meds?
Yes - but not always the way you think. If you’re on an inhaler and your asthma symptoms keep flaring, or your blood sugar stays high despite taking insulin, your doctor will notice. They won’t know if you skipped a dose unless you tell them - or unless you’re using a smart device that tracks usage. But your body tells the story. Don’t wait for them to notice. Be honest. They’ve heard it all before. Their job is to help you, not judge you.
What’s the easiest way to remember all my meds?
Use a pill organizer with time slots - morning, afternoon, evening. But for inhalers, patches, and injectables, a phone calendar works better. Set one reminder per day for each medication, labeled clearly: “Inhaler - 7 AM,” “Patch Change - Monday.” Don’t use vague labels like “Take Meds.” Be specific. And if you’re overwhelmed, ask your pharmacist to simplify your regimen. Sometimes switching to a once-daily version makes everything easier.
What’s Next?
If you’ve been struggling with your inhaler, patch, or injectable, start today. Don’t wait for the next appointment. Walk into your pharmacy and ask for a technique check. Set one reminder. Write down one thing that’s stopping you. Then talk to your doctor.
You’re not alone. Millions of people are right where you are. And there are real, simple ways out. It’s not about being perfect. It’s about being consistent. One dose at a time.


Rod Wheatley
January 22, 2026 AT 01:07I used to miss my inhaler all the time-until I started using it right after brushing my teeth. Now it’s automatic. No alarms, no stress. Just brush, breathe, done. Eight months clean.
Also, get a spacer. $10 at CVS. Game changer.
Ashok Sakra
January 22, 2026 AT 23:05OMG I HATE INJECTABLES SO MUCH I CRIED LAST WEEK WHEN I HAD TO DO ONE AND MY KID SAW ME AND NOW HE THINKS I’M A VAMPIRE 😭😭😭
Andrew Rinaldi
January 24, 2026 AT 19:31It’s interesting how the body becomes a system we’re trying to optimize, but we forget it’s also a lived experience. The tech helps, sure-but the real adherence comes from feeling safe, seen, and supported. Not tracked.
Maybe the question isn’t ‘how do we make people comply?’ but ‘how do we make compliance feel like care?’
Gerard Jordan
January 25, 2026 AT 15:22Spacers are LIFE. 🙌 I didn’t believe it until my grandma used one after her ER trip. Now she calls it her ‘magic tube.’
Also, if you’re scared of needles, try holding ice on the spot first. Numbs it out. And yes, watching your favorite show while injecting? Genius. 📺💉
michelle Brownsea
January 27, 2026 AT 07:49Let’s be clear: non-adherence isn’t a ‘system failure’-it’s a personal failure of discipline. If you can’t manage to press a button or change a patch on time, you’re not ‘chronically ill,’ you’re chronically irresponsible.
People who blame ‘cost’ or ‘confusion’ are just avoiding accountability. I’ve seen people with no insurance, no smartphone, and no education-still take their meds. How? Because they cared enough to try.
Stop romanticizing noncompliance. It’s not ‘human-centered’-it’s lazy.
MAHENDRA MEGHWAL
January 27, 2026 AT 11:11Respectfully, I would like to offer a perspective from a rural community in India. Many patients do not have access to spacers, smart pens, or even refrigeration. Yet, they manage through community support-neighbors reminding each other, pharmacists visiting homes, and families holding each other accountable.
The solutions proposed here are excellent, but they assume a level of infrastructure that does not exist for millions. Perhaps the real innovation is not in technology, but in human connection.
Thank you for writing this. It is a step forward.
Philip Williams
January 28, 2026 AT 17:00There’s a critical flaw in the claim that smart devices overestimate adherence by 15–20%. The studies cited do not consistently control for inhalation depth across device types. Many sensors only detect actuation, not lung deposition.
Until we have reliable biomarkers of actual drug delivery, all adherence metrics are proxies at best. We need to stop treating sensor data as gospel.
Also, why are we not discussing the role of caregiver burden? Many elderly patients rely on family to administer-what happens when the family member is overworked?
Jerry Rodrigues
January 30, 2026 AT 11:04My patch fell off in the shower. Again. So I stuck it on with duct tape. It’s gross. But it works.
Also, I use my inhaler while waiting for my coffee to brew. Doesn’t even think about it anymore.
Uju Megafu
February 1, 2026 AT 01:31Oh wow, so now it’s the SYSTEM’S fault? Let me guess-you also blame the weather for your bad decisions?
My aunt died from uncontrolled asthma because she ‘forgot’ to use her inhaler for 6 months. She didn’t have money? Fine. But she had a phone. She had family. She had a doctor.
Stop gaslighting people into thinking this is all about access. It’s about will. And yours is weak.
Jarrod Flesch
February 1, 2026 AT 20:39Just wanted to say-spacers are the unsung heroes of asthma care. I used to get thrush every month. Now? Zero. And I use a $7 plastic one.
Also, if you’re scared of needles, try the ‘pinch and inject’ method. Less pain. I swear.
And yeah, watching Netflix while injecting? 10/10. 👍
Stephen Rock
February 1, 2026 AT 21:10Smart inhalers? Please. That’s just corporate surveillance wrapped in wellness. You think your data’s private? Nah. It’s sold to insurers who then raise your premiums.
Also, ‘habit stacking’? Sounds like a TikTok trend. Real people don’t have time for that. Just give me a once-a-month shot and shut up.
Amber Lane
February 2, 2026 AT 15:24Spacers work. Just use one.
lokesh prasanth
February 3, 2026 AT 14:16why do people use spacers? i thought the inhaler was enough? also patch falling off is just laziness. if you cant stick it on then you dont deserve to be healthy
Malvina Tomja
February 4, 2026 AT 08:33You say ‘don’t wait for the next appointment’-but what if your doctor doesn’t care? What if they dismiss you? What if they’ve seen 20 patients before you and just want to move on?
I’ve asked 3 times for a different patch. They said ‘it’s fine.’ My skin is raw.
So yes-system failure. And I’m tired of being told to ‘try harder’ when the system won’t even listen.
Samuel Mendoza
February 6, 2026 AT 04:15Actually, the 70% incorrect inhaler use stat is from a 2011 study. The 2021 one you cite? It was a small sample of urban clinic patients. Most rural users use them correctly because they’ve been doing it for 20 years.
You’re overcomplicating this. If it’s that hard, switch to oral meds. Done.