PCOS Progesterone Level Estimator
Estimated Progesterone Status
Enter your information and click "Estimate Progesterone Status" to see results.
Quick Take
- Progesterone prepares the uterus for pregnancy; low levels are common in PCOS.
- Insulin resistance and chronic anovulation keep progesterone production low.
- Symptoms include irregular periods, spotting, and difficulty conceiving.
- Lifestyle changes and targeted therapies can raise progesterone naturally.
- Medical options like cyclic progestins or IVF‑friendly protocols help restore fertility.
When we talk about progesterone is a steroid hormone produced mainly by the ovaries after ovulation, essential for preparing the uterine lining for pregnancy, its role often gets eclipsed by the more talked‑about hormones like estrogen or testosterone. Yet, in the world of progesterone and PCOS, the missing piece of the puzzle is frequently progesterone itself. This article unpacks why women with Polycystic Ovary Syndrome (PCOS) often have low progesterone, how that fuels the classic PCOS symptoms, and what real‑world steps you can take to break the cycle.
What Is Polycystic Ovary Syndrome?
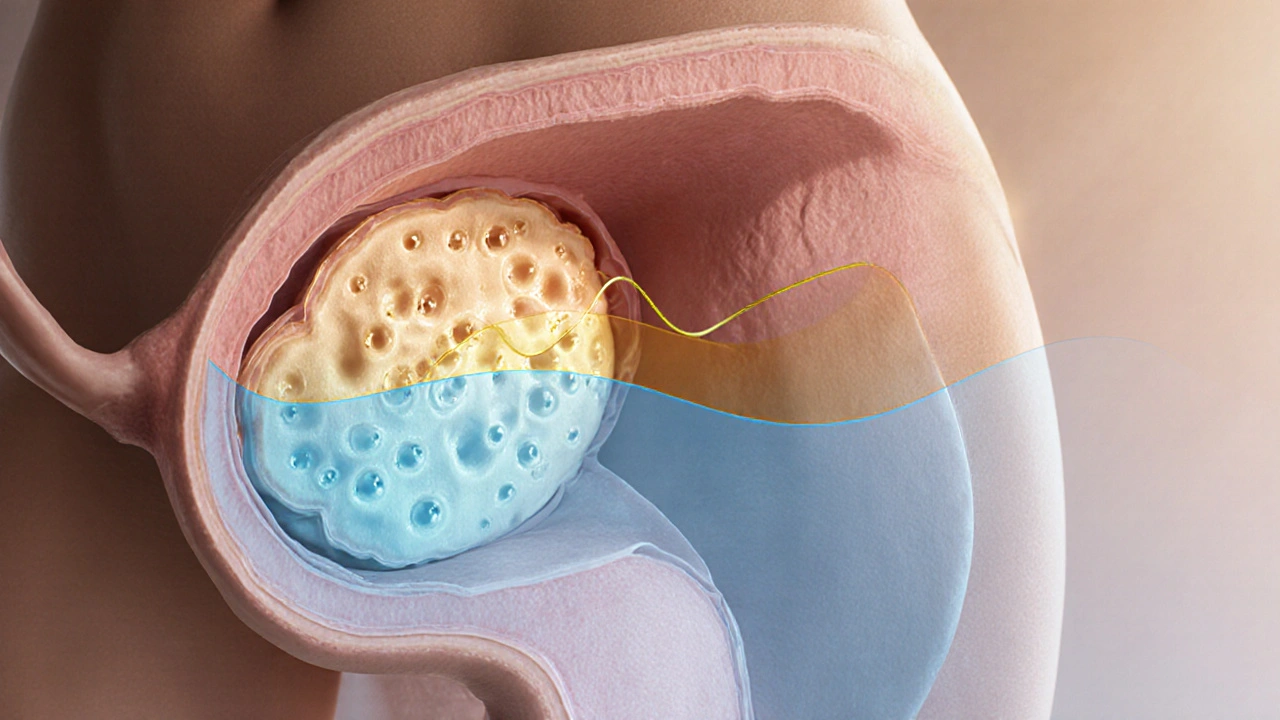
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting 8‑13% of women of reproductive age worldwide. It’s characterized by a trio of signs: irregular or absent ovulation, hyperandrogenism (high male‑type hormones), and polycystic‑looking ovaries on ultrasound. The condition isn’t just about “cysts”; it’s fundamentally a hormonal imbalance that ripples through metabolism, skin, and fertility.
Hormonal Role of Progesterone
Progesterone does three things that matter for PCOS:
- Stabilizes the uterine lining: After ovulation, the corpus luteum secretes progesterone, turning the thickened endometrium into a receptive bed for a fertilized egg.
- Counteracts estrogen: While estrogen promotes tissue growth, progesterone tells the body to stop proliferating, preventing over‑growth that leads to heavy bleeding.
- Supports the luteal phase: A healthy luteal phase (the period between ovulation and menstruation) depends on sustained progesterone, which in turn supportsembryo implantation.
When the luteal phase is shortened or absent, the body never gets the progesterone signal, and the cycle stays in an estrogen‑dominant state.
Why Progesterone Often Falls Short in PCOS
Two core mechanisms drive low progesterone in PCOS:
- Chronic anovulation: Many women with PCOS never ovulate regularly, so the corpus luteum never forms, and progesterone never spikes.
- Insulin resistance: Insulin resistance is a metabolic hallmark of PCOS. High insulin levels boost ovarian androgen production, which blocks follicle maturation and thus ovulation.
Both pathways reinforce each other. The more anovulatory cycles you have, the less progesterone you make; the less progesterone you have, the more the endometrium stays estrogen‑driven, leading to irregular shedding and spotting.
Clinical Signs of Progesterone Deficiency in PCOS
Low progesterone isn’t always obvious, but look for these clues:
- Irregular periods or prolonged amenorrhea (no period for >3 months).
- Spotting between periods - a classic sign of an unopposed estrogen environment.
- Infertility or repeated miscarriage - without a proper luteal phase, implantation struggles.
- Premenstrual mood swings that feel more “sharp” than “blunted,” often linked to low progesterone’s calming effect on the brain.
- Weight gain or difficulty losing weight - progesterone influences appetite regulation and fat storage.
These symptoms often overlap with other PCOS markers like hirsutism (excess hair growth) and acne, making it easy to miss the progesterone angle.
Diagnosing Low Progesterone in a PCOS Context
Doctors typically check progesterone on day21 of a standard 28‑day cycle. In PCOS, because cycles are irregular, timing can be tricky. Two practical approaches are:
- Mid‑luteal blood test: Collect a sample about 7days after a documented ovulation (via LH surge or ultrasound).
- Progesterone challenge: Give a short course of oral progestin; if bleeding occurs afterward, it confirms the uterus can respond, indicating the problem is lack of natural progesterone, not an out‑flow issue.
These tests, combined with a full hormonal panel (testosterone, LH/FSH ratio, fasting insulin), give a clear picture of where the endocrine imbalance lies.
Managing Low Progesterone: Lifestyle First
Diet, exercise, and sleep have a surprisingly strong impact on progesterone production:
- Low‑glycemic diet: Reducing refined carbs lowers insulin spikes, which in turn reduces ovarian androgen output, allowing follicles to mature.
- Regular strength training: Increases muscle sensitivity to insulin, improves ovulatory rates, and can raise natural progesterone by up to 30% in some studies.
- Stress management: Cortisol competes with progesterone at the hormone‑synthesis level. Mindfulness, yoga, or even a 30‑minute walk can tilt the balance back toward progesterone.
Weight loss of even 5‑10% often restores ovulation in overweight women with PCOS, indirectly boosting progesterone.
Medical Options to Boost Progesterone
If lifestyle tweaks don’t normalize cycles, clinicians have several tools:
| Therapy | Mechanism | Typical Use | Key Considerations |
|---|---|---|---|
| Oral cyclic progestins (e.g., medroxyprogesterone acetate) | Mimic luteal phase hormone | Induce regular withdrawal bleeding | May cause mood changes; not for pregnancy attempts |
| Micronized progesterone (vaginal or oral) | Bioidentical, closely matches natural hormone | Supports luteal phase in IVF cycles | Needs consistent daily use; can cause mild nausea |
| Clomiphene citrate or letrozole | Triggers ovulation, indirectly raising progesterone | First‑line for fertility | Risk of multiple eggs, monitor with ultrasound |
| Metformin | Improves insulin sensitivity, reduces androgen excess | Adjunct for metabolic PCOS | Gastro‑intestinal upset common; dose titration needed |
When pregnancy is the goal, the focus shifts to agents that promote ovulation (clomiphene, letrozole) because each ovulation brings a fresh corpus luteum and a natural progesterone surge. In women who can’t ovulate despite these drugs, supplemental micronized progesterone during the luteal phase of IVF cycles improves implantation rates.
When to Seek Professional Help
If you notice any of the following, it’s time to schedule an appointment:
- Four or more months without a period.
- Repeated miscarriage or difficulty staying pregnant past 12weeks.
- Severe acne, deepening voice, or rapid hair growth on the face/chest.
- Persistent weight gain despite diet and exercise.
A qualified endocrinologist or reproductive specialist can run the hormone panel, order an ultrasound, and tailor a treatment plan that addresses both insulin resistance and progesterone deficiency.
Bottom Line
Low progesterone is both a symptom and a driver of the PCOS cycle. By understanding how chronic anovulation, insulin resistance, and excess androgens keep progesterone levels low, you can target the root cause rather than just treating the surface issues. Combining smart lifestyle changes with the right medical support often restores a healthy luteal phase, eases menstrual irregularities, and opens the door to fertility.
Frequently Asked Questions
Can low progesterone cause weight gain in PCOS?
Yes. Progesterone influences appetite and fat storage. When progesterone stays low, the body tends to store more fat, especially in the abdominal region, and cravings for high‑carb foods increase.
Is it safe to take over‑the‑counter progesterone creams?
Topical creams deliver very little hormone systemically and are not reliable for correcting a luteal phase deficit. Prescription micronized progesterone or cyclic progestins are the evidence‑based options.
How long does it take for lifestyle changes to raise progesterone?
For many women, regular exercise and a low‑glycemic diet restore ovulation within 3‑6months, which in turn normalizes progesterone. The timeline varies based on baseline weight, insulin sensitivity, and severity of hormonal imbalance.
Does metformin directly increase progesterone?
Metformin doesn’t boost progesterone directly. It improves insulin sensitivity, lowers androgen production, and often allows follicles to mature, which then leads to a natural progesterone rise after ovulation.
Can I get pregnant if my progesterone stays low?
Pregnancy is difficult but not impossible. Low progesterone often means fewer ovulations, which reduces the chance of conception. Assisted reproductive technologies that include luteal‑phase support can overcome this hurdle.





Badal Patel
October 2, 2025 AT 22:40While the article extols lifestyle modifications as the panacea for progesterone deficiency, one must not ignore that hormonal therapy, when judiciously applied, remains the cornerstone of effective PCOS management, especially for patients whose anovulation persists despite dietary effort, thus a balanced approach, integrating both diet and medication, proves essential, lest we fall into the trap of romanticizing weight loss alone as the cure‑all.
KIRAN nadarla
October 3, 2025 AT 12:34The piece suffers from a litany of stylistic missteps; headings bob and weave without hierarchy, the estimator script is embedded amid prose, and the use of “you” creates an informal tone that clashes with the otherwise clinical narrative-additionally, the term “progesterone‑focused therapies” should be hyphenated consistently, and the occasional dangling modifier (“When lifestyle tweaks don’t normalize cycles”) leaves the sentence hanging, undermining the authority the author seeks to convey.
Kara Guilbert
October 4, 2025 AT 02:27Honestly, if you keep ignorng the root cause of insulin resistance you are basically choosing to stay sick, and that is just not okay-people need to take responsability for their bodies instead of blaming “PCOS” for everything.
Sonia Michelle
October 4, 2025 AT 16:20Think of progesterone not just as a hormone, but as a bridge between metabolic health and fertility; when we address insulin sensitivity through diet and exercise, we often see a natural resurgence of ovulation, which in turn restores the luteal phase and balances estrogen, creating a virtuous cycle that supports both mood and reproductive goals.
Neil Collette
October 5, 2025 AT 06:14Wow, because obviously everyone with PCOS just needs to pop a pill and magically start ovulating, right? As if a one‑size‑fits‑all prescription could outmuscle the complex interplay of genetics, environment, and stress-your so‑called “quick take” glosses over the fact that many women won’t respond to progestins without first tackling the underlying insulin resistance, which, surprise surprise, isn’t solved by a single tablet.
James Lee
October 5, 2025 AT 20:07Sure, but hormones are more than just “low” or “high”.
Dennis Scholing
October 6, 2025 AT 10:00For anyone feeling overwhelmed, start with small, sustainable steps: aim for a modest 5‑10% weight loss, incorporate low‑glycemic carbs, and schedule a regular moderate‑intensity workout three times a week; these changes often improve insulin sensitivity enough to allow ovulation to resume, which naturally raises progesterone levels without the need for immediate pharmacologic intervention.
Kasey Lauren
October 6, 2025 AT 23:54You’ve got this-tiny lifestyle tweaks can lead to big hormone wins!
joshua Dangerfield
October 7, 2025 AT 13:47One practical tip that’s often overlooked is timing your strength training sessions earlier in the day; research suggests that morning resistance workouts may enhance insulin sensitivity more effectively than evening sessions, which can help the ovaries recover and produce a healthier luteal phase, ultimately boosting progesterone levels.
Abhimanyu Singh Rathore
October 8, 2025 AT 03:40Allow me to point out, with the utmost respect, that the term “progesterone status” should be consistently capitalized when referring to the diagnostic category, and that the phrase “low progesterone is common in PCOS” would read more smoothly as “low progesterone is common in PCOS”; moreover, the serial comma after “diet, exercise, and sleep” adds clarity-let us not sacrifice precision for brevity, for precision is the soul of science!
Stephen Lewis
October 8, 2025 AT 17:34It is advisable to consult a qualified endocrinologist who can interpret the full hormonal panel, including fasting insulin and LH/FSH ratios, before embarking on any hormonal therapy; such a professional will tailor treatment to the individual’s metabolic profile, thereby maximizing the odds of restoring a functional luteal phase.
janvi patel
October 9, 2025 AT 07:27While many celebrate lifestyle changes, I maintain that without pharmacologic support, a substantial portion of women will never achieve a true luteal phase, rendering the emphasis on diet alone somewhat naïve.
Lynn Kline
October 9, 2025 AT 21:20Let’s celebrate the fact that even modest adjustments-like swapping sugary snacks for berries, or adding a quick 15‑minute yoga flow-can ripple through the endocrine system, fostering a more balanced estrogen‑progesterone ratio and lighting up the path toward fertility with a burst of optimism!!!
Rin Jan
October 10, 2025 AT 11:14I have spent countless hours listening to the same tired narratives about PCOS that glorify “just eat better” as a cure‑all. The reality is that hormonal imbalance is a multifactorial beast that does not yield to simplistic advice. Women suffering from progesterone deficiency often feel trapped in a cycle of hope and disappointment. They are told to lose weight, yet the underlying insulin resistance remains untouched. They are prescribed metformin, but without proper monitoring the side effects become another burden. The medical community sometimes dismisses their pain as merely “mood swings” rather than acknowledging the physiological underpinnings. Each missed ovulation represents a lost opportunity for the body to produce the crucial luteal hormone. When progesterone stays low, the endometrium remains in an estrogen‑dominant state, leading to irregular bleeding and spotting. This hormonal chaos feeds anxiety, which in turn raises cortisol-another hormone that competes with progesterone for synthesis. It becomes a self‑fulfilling prophecy where stress begets more stress. Therefore, any comprehensive treatment plan must address stress management alongside metabolic health. Mind‑body practices such as mindfulness meditation have been shown to lower cortisol levels. Coupled with a low‑glycemic diet, they can gradually restore the body's natural hormonal rhythm. Patience is essential because the endocrine system does not reset overnight. Ultimately, a balanced approach that honors both the science and the lived experience offers the best chance for recovery.
Jessica Taranto
October 11, 2025 AT 01:07Indeed, integrating stress‑reduction techniques, such as regular meditation, moderate exercise, and adequate sleep, can significantly lower cortisol levels, which in turn facilitates progesterone synthesis, thereby supporting a healthier luteal phase, and it is crucial to monitor these variables regularly, perhaps using a journal or app, to track progress over time.
akash chaudhary
October 11, 2025 AT 15:00Frankly, the article’s “quick take” reads like a superficial checklist, ignoring the deep metabolic pathways; the author should have delved into the mechanistic link between insulin signaling and steroidogenesis rather than offering platitudes, because without that insight readers are left with a half‑baked understanding that does no one any real good.