When someone with type 2 diabetes and obesity tries everything-diet, exercise, pills, insulin-and still can’t get their blood sugar under control, what’s left? For many, the answer isn’t another pill. It’s surgery. Not the kind you think of for an appendectomy, but something more precise, more powerful: metabolic surgery. And the results? They’re not just about losing weight. They’re about reversing a disease that’s been eating away at your health for years.
How Metabolic Surgery Changes Your Body (And Your Blood Sugar)
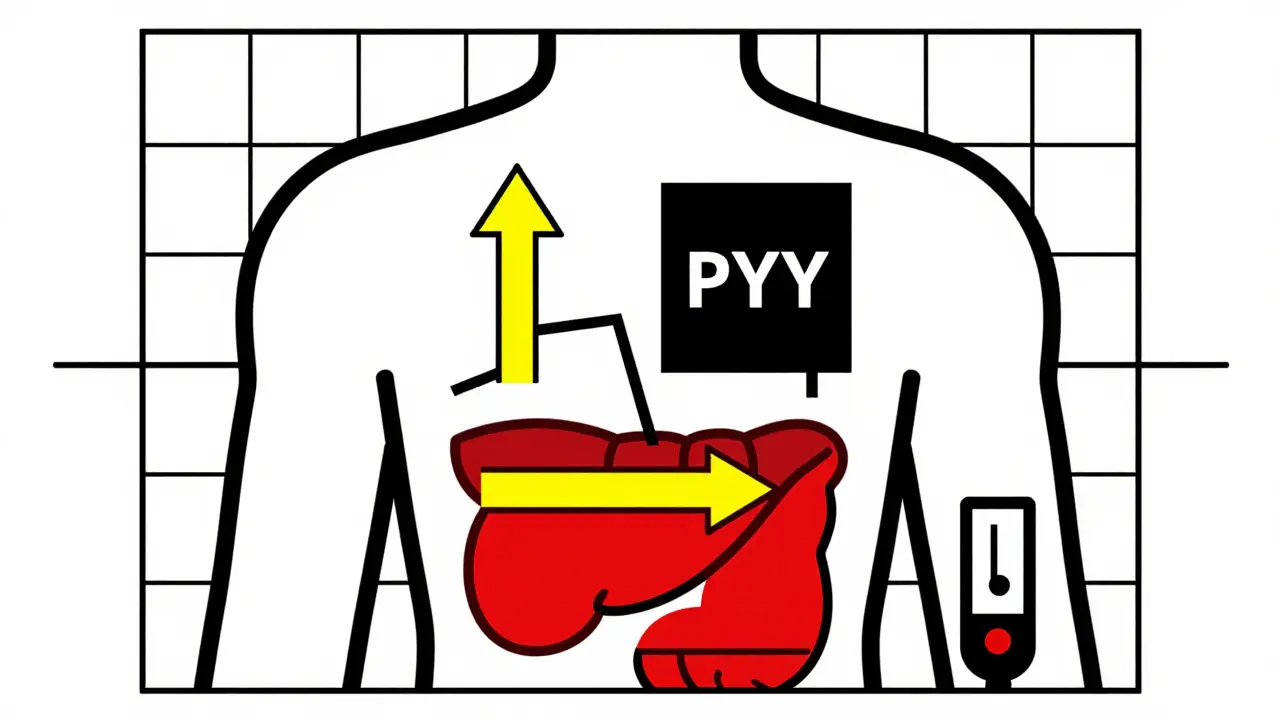
Metabolic surgery isn’t just about shrinking your stomach. It’s about rewiring how your body handles food, hormones, and energy. The most common procedures-gastric bypass, sleeve gastrectomy, and duodenal switch-don’t just limit how much you can eat. They change the signals your gut sends to your pancreas, liver, and brain. That’s why, for many patients, blood sugar levels drop within days of surgery-even before they’ve lost much weight.
This isn’t magic. It’s biology. After gastric bypass, your gut starts producing more GLP-1 and PYY, hormones that help your pancreas release insulin more efficiently and tell your brain you’re full. At the same time, ghrelin-the hunger hormone-plummets. The result? Less appetite, better insulin control, and a body that stops treating sugar like a poison.
Weight Loss That Actually Sticks
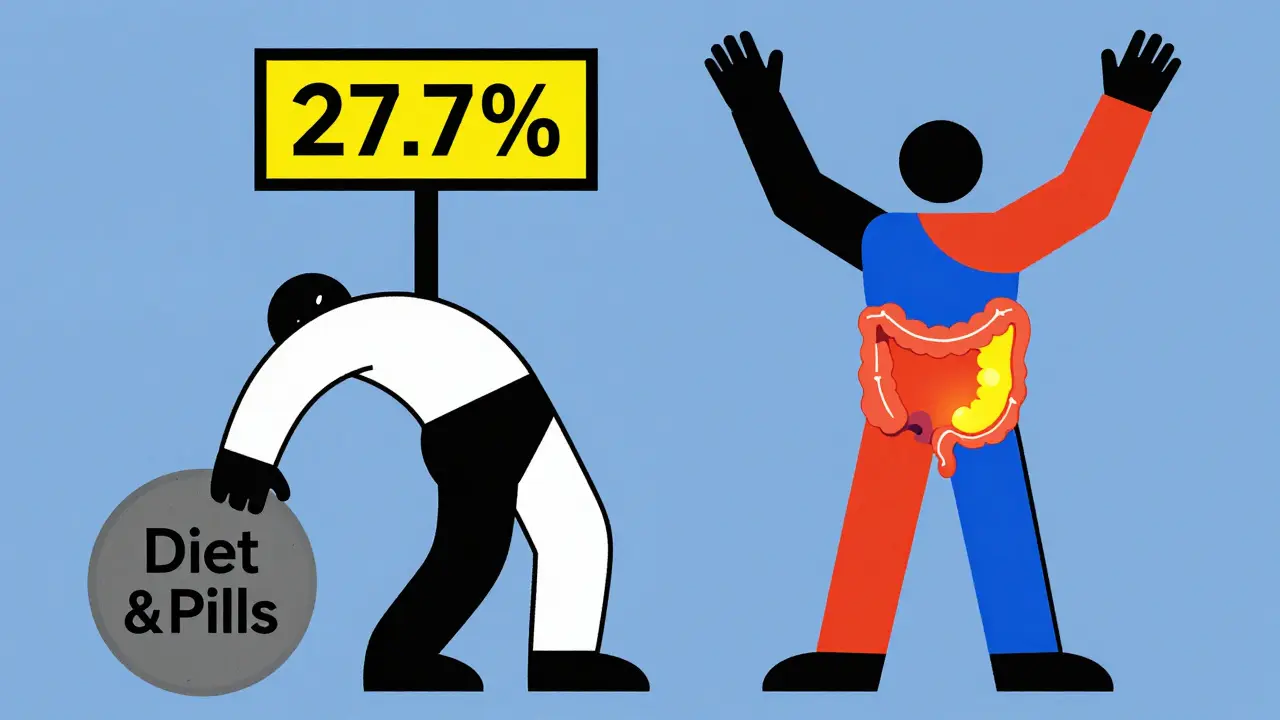
Let’s get real: most diets fail. People lose weight, then gain it back-often with extra. Metabolic surgery changes that pattern. On average, patients lose 27.7% of their starting body weight. Compare that to medical therapy alone, where people lose just 0.2%. That’s not a small difference. That’s life-changing.
Long-term data from the Swedish Obese Subjects study shows that 15 years after surgery, patients kept off nearly 20% of their excess weight. Gastric bypass patients with a starting BMI of 45.9 lost nearly 20% of their total body weight over six years. Sleeve gastrectomy patients lost slightly less-but still far more than anyone managing diabetes with pills and willpower alone.
And it’s not just about the number on the scale. It’s about how you feel. People report more energy, less joint pain, better sleep, and the ability to move without exhaustion. Many stop needing mobility aids. Others return to jobs they couldn’t do before. These aren’t side effects. They’re outcomes.
Diabetes Remission: It’s Real, and It’s Measurable
Here’s the most powerful part: metabolic surgery doesn’t just help manage type 2 diabetes-it can make it disappear.
One-year remission rates? Gastric bypass leads the pack at 42%. Sleeve gastrectomy? 37%. Biliopancreatic diversion (duodenal switch)? A staggering 95.1%. These aren’t theoretical numbers. They’re from real patients in real studies published in top medical journals.
And the remission lasts. Five years after surgery, 29% of gastric bypass patients and 23% of sleeve patients still had no signs of diabetes. Compare that to medical therapy: only 6.5% of non-surgical patients had remission after 15 years. That’s a five-fold difference.
Even more striking: in patients with BMI under 35-people who don’t even qualify as severely obese-metabolic surgery still achieved 36% complete remission. That’s a game-changer. It means surgery isn’t just for people who are extremely overweight. It’s for anyone with diabetes who’s struggling to control it.
Who Benefits the Most?
Not everyone responds the same way. The best candidates aren’t just the heaviest. They’re the ones who haven’t been on insulin for long.
Studies show that patients who haven’t needed insulin before surgery have a 53.8% chance of remission 14 months after surgery. Those already using insulin? Their odds drop significantly. Why? Because insulin use often means the pancreas is already worn out. Surgery can’t bring back dead cells.
Also, the sooner you act, the better. If you’ve had diabetes for less than five years, your chances of remission are much higher. After ten years, the pancreas may have lost too much function. That’s why waiting too long is one of the biggest mistakes people make.
And BMI matters-but not as much as you think. While guidelines often say you need a BMI over 35, studies now show people with BMIs as low as 24 can still achieve remission. The key isn’t just weight. It’s how your body is responding to the disease.
What About the Risks?
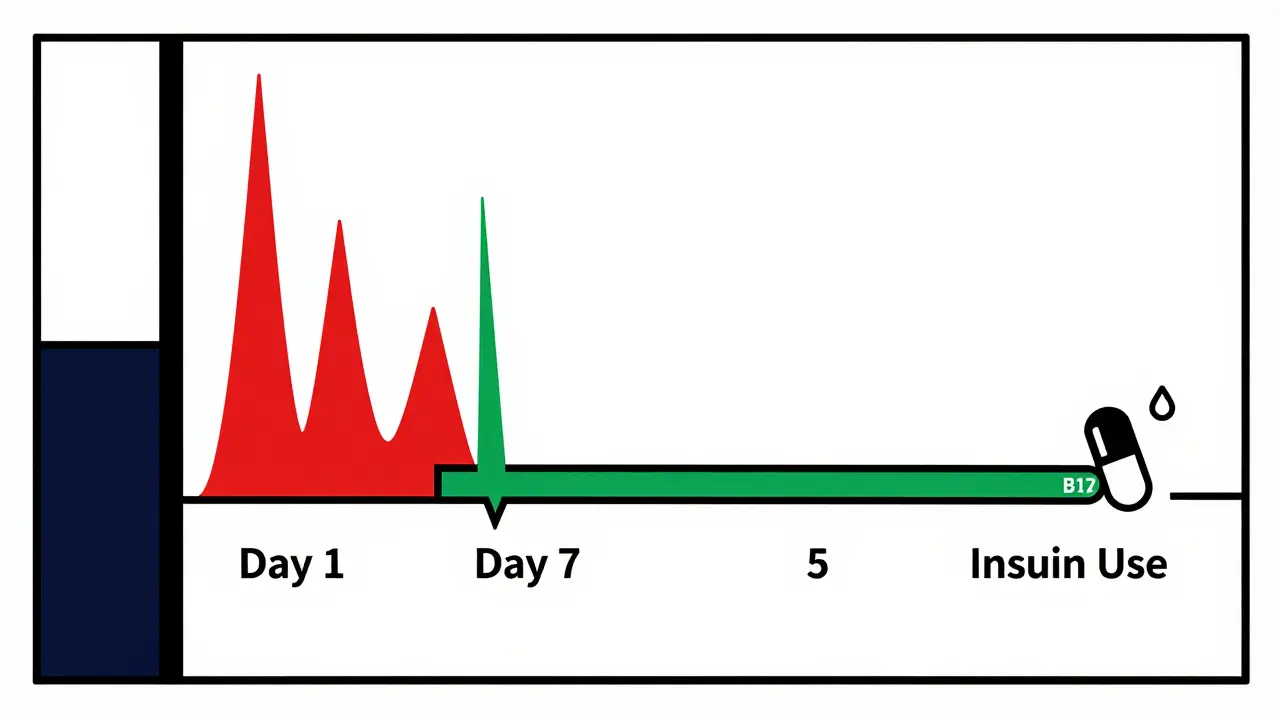
Surgery isn’t risk-free. You can’t ignore that. The most common issues are nutritional: low iron, vitamin B12, calcium, and vitamin D. That’s why lifelong follow-up is non-negotiable. You’ll need blood tests every year, sometimes every six months. You’ll need supplements. You’ll need to eat differently.
Some patients develop anemia. Others have gastrointestinal problems-nausea, dumping syndrome, or diarrhea. A small number experience bone fractures later in life due to calcium and vitamin D loss. These aren’t rare. They’re expected. And they’re manageable-with the right care.
But here’s the thing: the risks of not doing anything are often higher. Uncontrolled diabetes leads to kidney failure, blindness, nerve damage, heart attacks, and amputations. Metabolic surgery cuts the risk of these complications by nearly 20% for every year you stay in remission. That’s not a gamble. That’s a trade-off.
Why Isn’t Everyone Getting It?
If the evidence is this strong, why do only 1-2% of eligible patients get surgery? The answer is complicated.
Insurance won’t cover it for people with BMI under 35-even though the science says they benefit. Doctors don’t always know the data. Some still think surgery is only for extreme obesity. Patients are scared. They’ve heard horror stories about complications, or they believe surgery is a "cop-out"-that they should just eat less and exercise more.
But the data doesn’t lie. The STAMPEDE trial showed 42% of gastric bypass patients were in remission after one year. Only 12% of those on intensive medical therapy were. That’s not a tie. That’s a win. And it’s not just about pills. It’s about survival.
What Comes After Surgery?
Surgery isn’t the end. It’s the beginning of a new routine. You’ll need to eat smaller meals. You’ll need to chew slowly. You’ll need to avoid sugar and processed carbs. You’ll need to take vitamins for life. You’ll need to see your doctor regularly.
But here’s what changes: you won’t need insulin. You might not need any pills. Your A1C might drop from 9.5% to 5.4%. You might stop checking your blood sugar every day. You might start walking again-not because you have to, but because you want to.
And if your diabetes comes back? That doesn’t mean surgery failed. It means your body’s changing. Many patients still have better control than before surgery, even if they’re not fully in remission. They’re on fewer meds. Their numbers are lower. Their risk of complications is down. That’s still a win.
The Bigger Picture
Metabolic surgery isn’t a cure. It’s a tool. A powerful one. It doesn’t replace healthy eating or movement. It gives you the chance to make those things possible again.
For years, we treated type 2 diabetes like it was just a sugar problem. We gave pills. We blamed patients. We told them to try harder. But the truth? It’s a metabolic disease. And sometimes, the body needs a reset. Surgery doesn’t fix everything. But for many, it’s the reset they never knew they needed.
It’s not about being "thin." It’s about being well. And that’s worth more than any diet ever could be.
Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it can lead to complete diabetes remission in a large number of patients-especially those who haven’t been on insulin for long. Studies show up to 95% of patients experience remission within the first year after certain procedures like duodenal switch. Long-term remission (five+ years) is seen in 20-30% of patients, depending on the surgery type and individual factors like pre-surgery insulin use and duration of diabetes.
Is metabolic surgery only for people who are severely obese?
No. While guidelines often focus on BMI over 35, newer research shows patients with BMIs as low as 24-30 can still achieve high rates of diabetes remission. A 2019 study found gastric bypass led to 93% remission in patients with BMI 24-30. This means surgery isn’t just for "morbidly obese" patients-it’s an option for anyone with type 2 diabetes who hasn’t responded to other treatments, regardless of weight.
How soon after surgery does diabetes improve?
Many patients see their blood sugar drop within days of surgery-even before significant weight loss occurs. This is because metabolic surgery changes gut hormone signaling, improving insulin sensitivity and reducing liver glucose production. Patients often stop needing insulin or oral medications within the first week. This rapid improvement is one of the clearest signs that the effect is more than just weight loss.
What are the long-term risks of metabolic surgery?
Long-term risks include nutritional deficiencies-especially in iron, vitamin B12, calcium, and vitamin D-which can lead to anemia, osteoporosis, or bone fractures. Some patients experience gastrointestinal issues like dumping syndrome or chronic diarrhea. These risks are manageable with lifelong monitoring, supplements, and regular blood tests. The risk of complications is lower than the long-term risk of uncontrolled diabetes, which includes kidney failure, heart disease, blindness, and amputations.
Does metabolic surgery work for people already on insulin?
Yes, but outcomes are less dramatic. Patients who are insulin-dependent before surgery have lower remission rates-around 20-30%-compared to 50-90% for those who aren’t. This is because long-term insulin use often means the pancreas has lost much of its ability to produce insulin. Surgery can still improve blood sugar control and reduce insulin needs, even if full remission doesn’t happen.
How does metabolic surgery compare to weight-loss drugs like Ozempic?
Weight-loss drugs like semaglutide (Ozempic) are effective and help many people lose weight and improve blood sugar. But they don’t match the durability or remission rates of surgery. In head-to-head studies, gastric bypass led to 42% diabetes remission at one year, while intensive medical therapy (including drugs) reached only 12%. Surgery also leads to greater weight loss (27% vs. 10-15% with drugs) and more lasting improvements in cholesterol and triglycerides. Drugs require lifelong use; surgery offers a structural change that can last decades.
Is metabolic surgery covered by insurance?
Coverage varies widely. In the U.S., most insurers cover surgery for patients with BMI over 35 and type 2 diabetes. Coverage for BMI 30-34.9 is inconsistent, even though studies show benefit. In Australia, Medicare covers some procedures under specific criteria, but out-of-pocket costs can still be high. Many patients appeal denials, and success rates are rising as evidence grows. Always check with your insurer and ask for a pre-authorization based on clinical guidelines from the American Society for Metabolic and Bariatric Surgery.
What’s the recovery time after metabolic surgery?
Most patients stay in the hospital for 1-3 days. Recovery at home takes 2-6 weeks, depending on the procedure and individual health. Laparoscopic (keyhole) surgery is standard, so healing is faster than older open methods. Most people return to light work within 2-3 weeks and full activity within 6 weeks. Pain is usually mild to moderate and controlled with over-the-counter meds after the first few days.




Jack Havard
February 11, 2026 AT 13:05Gloria Ricky
February 12, 2026 AT 09:03christian jon
February 14, 2026 AT 08:24Pat Mun
February 16, 2026 AT 04:42Sophia Nelson
February 16, 2026 AT 05:03Skilken Awe
February 17, 2026 AT 03:03andres az
February 17, 2026 AT 18:02Steve DESTIVELLE
February 17, 2026 AT 20:13Neha Motiwala
February 18, 2026 AT 04:23Craig Staszak
February 19, 2026 AT 19:21