Metformin Dosing Calculator
Metformin Dosing Calculator
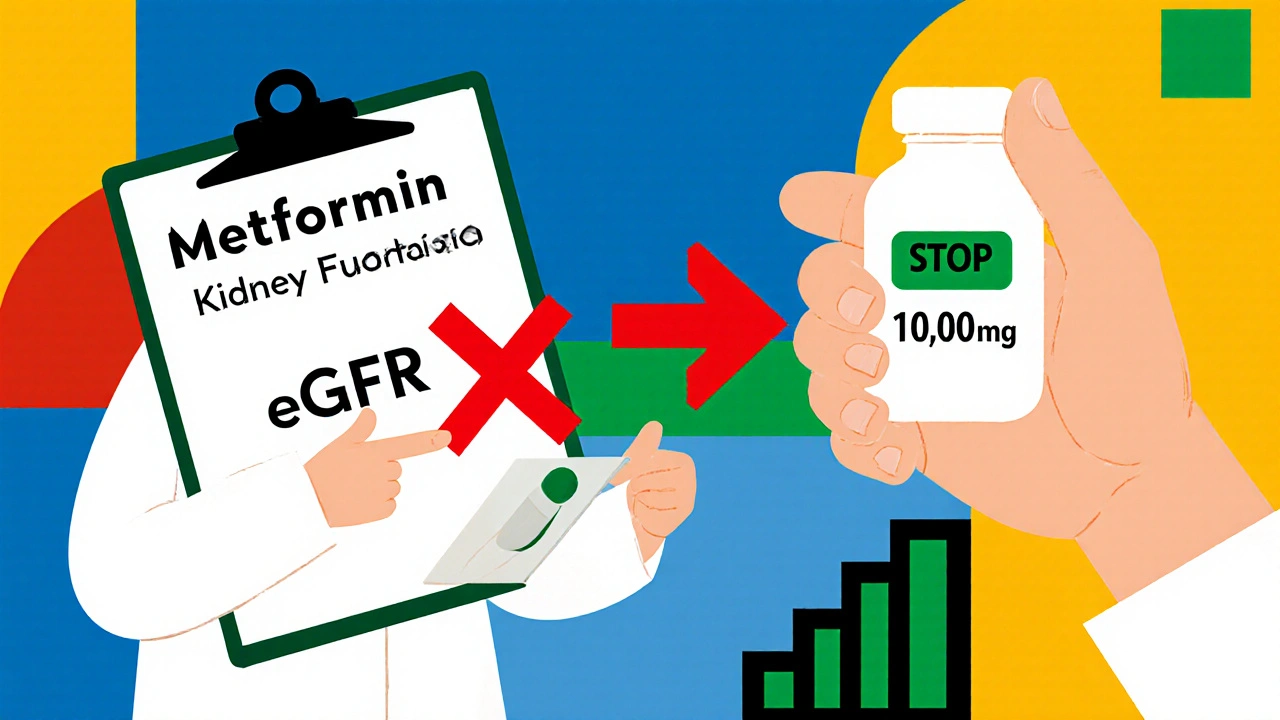
Enter your eGFR value (mL/min/1.73m²) to determine the maximum safe dose of metformin based on current clinical guidelines.
Dosing Recommendations
Enter your eGFR to see your recommended maximum daily dose.
Metformin is the most commonly prescribed diabetes medication in the world. It’s cheap, effective, and reduces the risk of heart attacks in people with type 2 diabetes. But if your kidneys aren’t working well, many doctors still tell you to stop taking it. That’s often the wrong call. The truth is, metformin doesn’t hurt your kidneys. It just leaves your body through them. And if your kidneys slow down, you need to adjust the dose-not stop the drug entirely.
Why Kidney Function Matters for Metformin
Metformin isn’t broken down by your liver. It doesn’t get metabolized at all. It passes through your kidneys, unchanged, and gets flushed out in your urine. That means if your kidneys aren’t filtering well, metformin builds up in your blood. High levels can, in rare cases, lead to lactic acidosis-a serious but extremely uncommon condition.
For years, doctors used serum creatinine levels to decide if someone could take metformin. If your creatinine was above 1.4 mg/dL for women or 1.5 mg/dL for men, you were told to stop. But creatinine is unreliable. It changes with muscle mass, age, and even diet. A muscular 70-year-old might have a normal creatinine but poor kidney function. An older, frail person might have low creatinine but kidneys that are barely working.
In 2016, the FDA changed the rules. They switched to using eGFR-estimated glomerular filtration rate. This number gives a much clearer picture of how well your kidneys are filtering waste. It’s calculated using your age, sex, race, and blood creatinine. Now, dosing is based on real kidney function, not a flawed lab value.
Current Dosing Guidelines by eGFR
Here’s what the major guidelines say today. These aren’t suggestions-they’re clinical standards backed by data from tens of thousands of patients.
- eGFR 60 or higher: You can take the full dose-up to 2,550 mg per day. Get your eGFR checked every 6 to 12 months.
- eGFR 45-59: Maximum dose is 2,000 mg per day. Check your kidney function every 3 to 6 months.
- eGFR 30-44: Maximum dose is 1,000 mg per day. Monitor every 3 months. This is the gray zone where many doctors still overreact.
- eGFR below 30: Metformin is generally not recommended. But even here, some patients with stable kidney function and no other risks may continue 500 mg daily under close supervision.
These aren’t arbitrary numbers. They come from studies tracking over 100,000 people with type 2 diabetes and chronic kidney disease. The risk of lactic acidosis in patients on metformin with eGFR above 30 is about 3.3 cases per 100,000 patient-years. That’s lower than the risk of a car accident on your daily commute.
What About Dialysis?
If you’re on dialysis, you still might need metformin. But the timing matters.
- Peritoneal dialysis: 250 mg once daily is safe.
- Hemodialysis: Take 500 mg after each dialysis session. Metformin is removed during dialysis, so you need to replace it afterward. Never take your full dose right before dialysis-it won’t help and could cause low blood sugar.
Many nephrologists now prefer metformin over other diabetes drugs in dialysis patients because it doesn’t cause weight gain or low blood pressure. It also doesn’t interact with other dialysis medications.
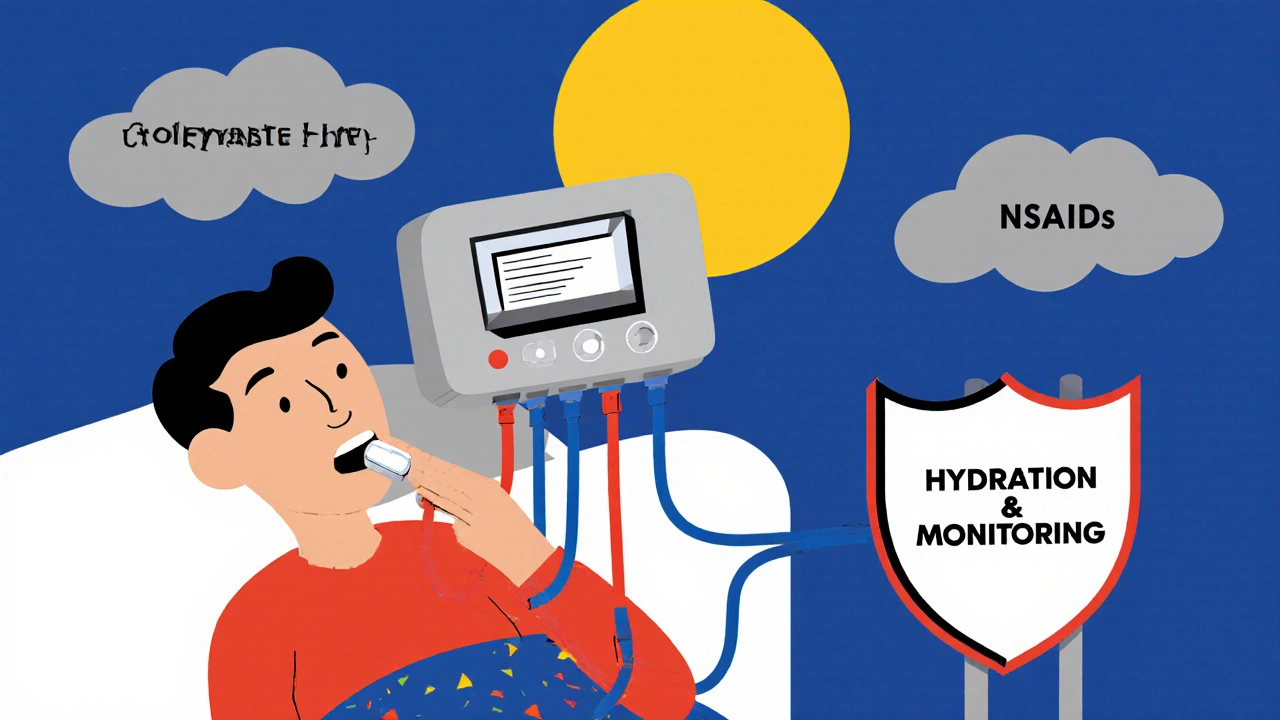
When You Must Hold Metformin
There’s one big exception: contrast dye.
If you’re getting a CT scan, angiogram, or any procedure using iodinated contrast, you need to stop metformin. Why? The dye can cause sudden kidney injury, especially if your eGFR is below 60. If your kidneys shut down temporarily, metformin builds up fast.
Here’s what to do:
- Stop metformin the day before the scan.
- Wait 48 hours after the procedure.
- Check your eGFR again.
- If it’s stable, restart at your previous dose.
Don’t restart without checking. A 2023 study found that 31% of patients who restarted metformin too soon after contrast dye had a spike in lactate levels-some even developed mild acidosis.
The Big Myth: Metformin Damages Kidneys
This is the most dangerous misconception in diabetes care.
Metformin does not cause kidney damage. It doesn’t inflame your kidneys. It doesn’t scar your nephrons. It just gets filtered out. If your kidneys are already damaged, the drug stays in your system longer. That’s why we adjust the dose-not stop it.
A 2022 chart review at the Cleveland Clinic found that 22% of patients with eGFR between 30 and 59 had metformin stopped unnecessarily. Their HbA1c jumped an average of 1.5% within three months. Many ended up on insulin sooner than needed, gained weight, and had more hypoglycemic episodes.
One patient, a 78-year-old woman with eGFR 42, had her metformin stopped after a routine blood test. Her doctor assumed the low eGFR meant she couldn’t take it. Her blood sugar soared. She developed diabetic neuropathy. She was put on insulin. Her monthly cost jumped from $6 to $280. All because of a myth.
What Other Guidelines Say
Not every guideline agrees perfectly. Here’s how they differ:
| eGFR Range | ADA/FDA | AACE/ACE | NICE (UK) | KDIGO |
|---|---|---|---|---|
| ≥60 mL/min | Full dose OK | Full dose OK | Full dose OK | Full dose OK |
| 45-59 mL/min | Max 2,000 mg | Reduce dose | Review dose | Safe if no AKI risk |
| 30-44 mL/min | Do not start; may continue | Reduce dose | Max 1,000 mg | Use with caution |
| <30 mL/min | Contraindicated | Contraindicated | Contraindicated | Consider 500 mg if stable |
The differences matter. In the U.S., you might be told to stop metformin at eGFR 45. In the UK, they’ll lower the dose. In Canada, RxFiles gives exact milligram limits. The bottom line? Don’t rely on one doctor’s opinion. Ask: Which guideline are you following?
Monitoring Beyond eGFR
eGFR isn’t the only thing to track.
- Vitamin B12: Metformin lowers B12 levels in 7-10% of long-term users. Get tested every 2-3 years. Low B12 can cause nerve damage, fatigue, and brain fog-symptoms that look like diabetes complications.
- NSAIDs: Avoid ibuprofen, naproxen, or celecoxib if your eGFR is below 60. These drugs can cause sudden kidney drops. Use acetaminophen instead for pain.
- Hydration: Dehydration from vomiting, diarrhea, or heat can crash your eGFR overnight. If you’re sick, hold metformin until you’re eating and drinking normally.
- Weight and mobility: Elderly patients with low muscle mass may have falsely high eGFR. If you’re frail, ask for a cystatin C test-it’s more accurate than creatinine for older adults.
What Happens If You Don’t Adjust the Dose?
There are two sides to this.
On one hand, stopping metformin in a stable patient with eGFR 38 can lead to uncontrolled blood sugar. One Reddit user shared that their 82-year-old patient’s HbA1c jumped from 6.8% to 8.9% after metformin was stopped. That’s a 31% increase in diabetes-related complications over five years.
On the other hand, continuing full doses when eGFR is below 30 can be dangerous. A 2022 case report described a 76-year-old man with eGFR 27 who kept taking 2,000 mg daily. He developed lactic acidosis with a blood pH of 6.98-life-threatening. He survived, but only after intensive care.
The key isn’t fear. It’s awareness. If your eGFR is below 45, you need a plan. Your doctor should be checking your labs every 3 months. You should know your number. And you should never skip a kidney test just because you feel fine.
How to Talk to Your Doctor
Many doctors still use old guidelines. If you’re told to stop metformin because your creatinine is high or your eGFR is 40, ask:
- “Is my kidney function stable, or did it drop suddenly?”
- “Can I stay on metformin at a lower dose?”
- “What’s my exact eGFR? Can I see the lab report?”
- “Will stopping this increase my risk of heart disease or stroke?”
Bring a printout of the ADA or NICE guidelines. Most doctors will respect evidence-based standards. If they refuse, ask for a referral to an endocrinologist or nephrologist.
Final Thoughts
Metformin is one of the best tools we have for type 2 diabetes. It protects your heart. It helps you lose weight. It’s affordable. And it doesn’t harm your kidneys.
If your kidneys are slow, don’t panic. Don’t stop. Adjust. Monitor. Stay informed. Your body isn’t broken-it’s just working differently. And with the right dose, metformin can still be part of your life for years to come.
Keep your eGFR numbers handy. Know your dose. Ask questions. And remember: metformin doesn’t cause kidney damage. Ignorance does.
Does metformin damage the kidneys?
No, metformin does not damage the kidneys. It is cleared from the body through kidney filtration, but it does not cause inflammation, scarring, or injury to kidney tissue. The misconception that metformin harms kidneys leads many patients to stop taking it unnecessarily, which can worsen blood sugar control and increase long-term complications.
What eGFR level is too low for metformin?
Metformin is generally contraindicated when eGFR falls below 30 mL/min/1.73 m². For eGFR between 30 and 44, the maximum daily dose is 1,000 mg with monitoring every 3 months. For eGFR 45-59, the max dose is 2,000 mg. Never start metformin if eGFR is below 30, but if you’re already on it and your kidney function slowly declines, you may continue at a reduced dose under supervision.
How often should kidney function be checked on metformin?
If your eGFR is 60 or higher, check it every 6-12 months. If it’s between 45 and 59, check every 3-6 months. If it’s between 30 and 44, check every 3 months. More frequent checks are needed if you’re sick, dehydrated, or starting a new medication like NSAIDs or contrast dye.
Can I take metformin if I’m on dialysis?
Yes, but the dose and timing matter. For peritoneal dialysis, 250 mg once daily is safe. For hemodialysis, take 500 mg after each session because the drug is removed during dialysis. Never take your full dose before dialysis-it won’t be effective and may cause low blood sugar.
Should I stop metformin before a CT scan with contrast dye?
Yes, if your eGFR is below 60. Stop metformin the day before the scan and don’t restart until 48 hours after the procedure. Check your kidney function again before restarting. If your eGFR is above 60, you can usually continue taking it as normal.
Can metformin cause vitamin B12 deficiency?
Yes, long-term metformin use is linked to lower vitamin B12 levels in 7-10% of users. This can lead to nerve damage, fatigue, or memory issues. Get your B12 checked every 2-3 years if you’ve been on metformin for more than 4 years. If levels are low, your doctor may recommend supplements.




Robert Merril
November 16, 2025 AT 14:40So let me get this straight metformin doesnt hurt kidneys but doctors still pull it like its poison lmao my grandpa was on it for 12 years with eGFR 38 and his sugar was better than mine with a Fitbit
they told him to stop because creatinine was 1.6 and now hes on insulin and his feet are numb
the system is broken
Noel Molina Mattinez
November 17, 2025 AT 03:13Stop metformin before contrast dye yes but why 48 hours why not 24 why not 72 nobody knows its just tradition like not eating before surgery
Roberta Colombin
November 17, 2025 AT 11:26Thank you for sharing this important information in such a clear way. Many people are afraid to take metformin because they believe it harms the kidneys, but the science shows otherwise. It is vital that patients understand their eGFR numbers and work with their doctors to adjust doses safely. Knowledge empowers us to make better choices for our health.
Let’s keep talking about this so no one has to stop a life-changing medication out of fear.
Dave Feland
November 18, 2025 AT 02:33Let me be perfectly clear - the FDA’s eGFR guidelines are a politically sanitized compromise born out of pharmaceutical lobbying and timid clinical inertia. The real data - from the 2022 Cleveland Clinic retrospective and the 2023 contrast dye study - proves that even eGFR 30–44 patients can safely tolerate 1500 mg daily if monitored with cystatin C and lactate levels. The fact that NICE allows 1000 mg while ADA says ‘may continue’ is a disgrace. This isn’t medicine. It’s bureaucratic cowardice dressed in white coats.
And don’t get me started on vitamin B12. The AMA has known about metformin-induced deficiency since 1997. Yet 80% of primary care docs still don’t test it. That’s malpractice by omission.
Ashley Unknown
November 18, 2025 AT 23:46Okay so I just found out my endo stopped my metformin because my creatinine was 1.4 and now I’m terrified I’m gonna die from lactic acidosis or worse - my insurance is gonna raise my premiums because I’m ‘high risk’ now
AND I just read that some doctors are STILL using creatinine instead of eGFR like we’re in 2005
WHAT IF THEY’RE LYING TO ME
WHAT IF THE LAB IS WRONG
WHAT IF THE CONTRAST DYE KILLS ME
WHAT IF MY B12 IS LOW AND NO ONE TOLD ME
WHAT IF I’M ALREADY HAVING NEUROPATHY AND I JUST THINK IT’S FROM STRESS
WHAT IF I’M GOING TO DIE BECAUSE SOMEONE DIDN’T UPDATE THEIR CLINICAL GUIDELINES IN 20 YEARS
WHO DO I SUE
WHY ISN’T THIS ON THE NEWS
WHY DO I FEEL LIKE I’M BEING EXPERIMENTED ON
Georgia Green
November 20, 2025 AT 13:07My doc switched me to 1000mg when my eGFR dropped to 41. I didn’t know about the B12 thing until my neurologist mentioned it last year. Got tested - low as hell. Took supplements, my brain fog cleared up. Still on metformin. Still alive. Still managing my sugar.
Just ask for the numbers. Don’t let them scare you off.
Christina Abellar
November 21, 2025 AT 03:08Good summary. I’ve seen too many patients stopped on metformin too early. Monitoring is key - not fear.
Eva Vega
November 22, 2025 AT 01:08The clinical utility of eGFR in the context of metformin pharmacokinetics is predicated upon the assumption of stable renal perfusion and absence of acute kidney injury (AKI). However, the concomitant use of NSAIDs, volume depletion, or iodinated contrast agents may precipitate a transient decline in GFR, thereby increasing the risk of metformin accumulation. The 48-hour hold post-contrast is thus not arbitrary but rather a risk-mitigation strategy informed by pharmacodynamic modeling and population-level pharmacovigilance data. Further, the KDIGO recommendation to consider 500 mg in eGFR <30 is an off-label application requiring individualized risk-benefit analysis, particularly in patients with preserved tubular secretion and no evidence of metabolic acidosis.
Matt Wells
November 23, 2025 AT 04:34It is regrettable that the general public continues to conflate pharmacokinetic clearance with nephrotoxicity. Metformin is not nephrotoxic - it is nephrodependent. The persistent misapplication of outdated creatinine thresholds reflects a troubling ignorance of renal physiology among non-specialists. One must question the competency of clinicians who prescribe insulin to patients with eGFR 45 simply because they are unaware of the 2016 FDA guidance. This is not patient care. This is medical negligence.
George Gaitara
November 24, 2025 AT 19:19And what about the fact that the FDA guidelines were written by people who have financial ties to big pharma? Metformin is generic. What if they want to push newer, more expensive drugs? What if they’re hiding data? I’ve seen studies where lactic acidosis rates were suppressed. They don’t want you to know you can still take it at eGFR 35. They want you on insulin so they can sell you pens and pumps and monthly subscriptions.
They’re lying. They’re all lying.
Deepali Singh
November 25, 2025 AT 04:18Let’s not ignore the socioeconomic layer here. Patients who can afford cystatin C tests, endocrinology referrals, and B12 supplements are the ones who benefit from these nuanced guidelines. The rest? They get told to stop metformin and are left with a $280 insulin prescription and a 1.5% HbA1c spike. This isn’t clinical wisdom - it’s healthcare inequality dressed as protocol.