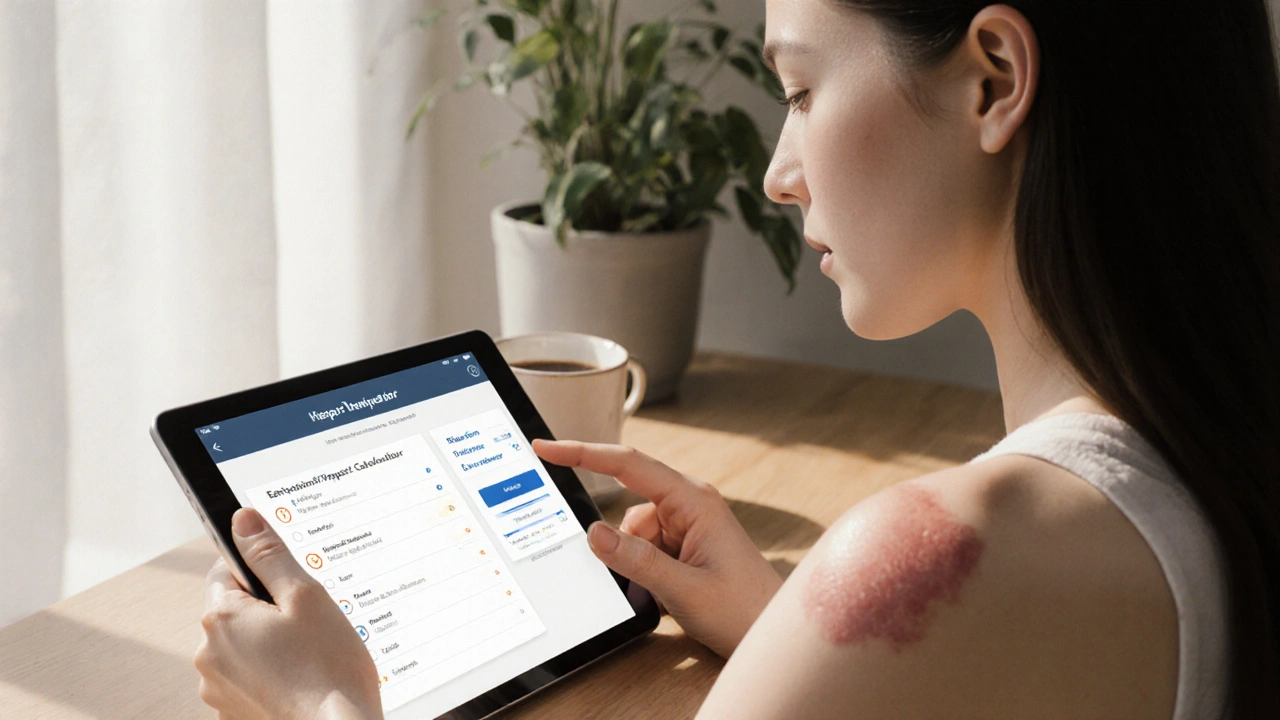
Tinea Versicolor Emotional Impact Calculator
Quick Summary
- tinea versicolor is a common fungal skin condition that can cause noticeable colour changes.
- The visible patches often trigger low self‑esteem, social anxiety and mood swings.
- Early diagnosis with a Wood's lamp and simple antifungal treatments can restore both skin tone and confidence.
- Support strategies-like talking to a dermatologist, joining online forums, and practising stress‑reduction-help manage the psychological load.
- Knowing the triggers (heat, humidity, oily skin) lets you prevent flare‑ups before they affect your life.
What Is Tinea Versicolor?
When most people hear the word "fungus," they picture a scary infection that spreads quickly. Tinea versicolor is a benign, yeast‑derived skin condition caused by an overgrowth of the fungus Malassezia. The organism lives on everyone's skin, but under warm, humid conditions it multiplies and interferes with melanin production, leading to light or dark patches.
Typical spots appear on the chest, back, shoulders and upper arms. They may be faint pink, white or brown, and often become more visible after sun exposure because the surrounding skin tans while the patches stay the same colour.
Why the Skin Changes Matter Psychologically
Seeing an uneven complexion can feel like a spotlight on an imperfection you never asked for. The visual difference isn't just cosmetic; it taps into deep‑seated concerns about appearance, especially in societies where clear skin is linked to health and confidence.
Two emotional cues dominate:
- Self‑esteem the personal evaluation of one's own worth often drops when a person feels their skin looks “abnormal.”
- Social anxiety the fear of being judged or rejected in social settings can spike, leading people to avoid pools, gyms, or even casual outings.
Studies from dermatology clinics in Australia (2023) show that 42% of patients with visible skin disorders report moderate to severe anxiety, and 28% experience depressive symptoms. Tinea versicolor, despite being medically mild, fits right into that pattern because the patches are hard to hide and often flare in summer.
Physical Symptoms That Feed the Emotional Loop
Beyond the colour change, many sufferers notice itching a mild to moderate irritation that worsens with sweating. The itch can become a constant reminder that something’s wrong, reinforcing negative thoughts.
Other triggers include:
- Heat and humidity - the fungus loves oily skin, so hot weather makes it thrive.
- Oily skin products - heavy moisturisers or oily sunscreens can feed the yeast.
- Hormonal shifts - stress hormones can alter skin oil production, creating a feedback loop.
When a flare‑up coincides with a big social event, the emotional impact magnifies, often creating a cycle of avoidance and increased stress, which in turn worsens the skin.

Breaking the Cycle: Coping Strategies
Understanding that the skin issue and the feelings are intertwined is the first step. Here are practical ways to start untangling them:
- Seek professional confirmation. A quick visit to a Dermatologist a medical specialist in skin health can give you a clear diagnosis, often using a Wood's lamp (see box below). Knowing it’s treatable reduces fear.
- Talk it out. Whether it’s a trusted friend, partner, or a mental‑health counselor, naming the worry lowers its power.
- Join a community. Online forums for skin‑condition sufferers (e.g., Reddit’s r/SkincareAddiction) let you see real‑life before‑after stories and hear coping tips.
- Practice stress‑reduction. Simple breathing exercises, short walks, or yoga can curb the hormone surge that fuels the fungus.
- Control the environment. Wear breathable fabrics, keep cool, and use non‑comedogenic sunscreen.
Diagnosis Made Simple
The gold‑standard test is a Wood's lamp examination. Under UV light, the affected patches glow a distinctive yellow‑green, confirming the presence of Malassezia. A skin scraping examined under a microscope can also reveal the characteristic “spaghetti‑and‑meatballs” pattern of yeast cells and hyphae.
Because the condition is not contagious and rarely leads to serious complications, the main goal of diagnosis is to reassure the patient and start treatment quickly.
Treatment Options: What Works Best?
Most cases clear up with a short course of antifungal therapy. Below is a quick comparison of the two main categories.
| Attribute | Topical Antifungal | Oral Antifungal |
|---|---|---|
| Common Drugs | Ketoconazole 2% cream, Selenium sulfide shampoo | Fluconazole 150mg weekly, Itraconazole pulse therapy |
| Typical Duration | 2‑4weeks | 2‑6weeks (depending on severity) |
| Effectiveness | 70‑80% clear after one course | 90‑95% clear, useful for extensive or recurrent cases |
| Side Effects | Localized irritation, rarely allergic reaction | Headache, GI upset, rare liver enzyme elevation |
| Convenience | Apply to affected areas once or twice daily | Take a pill; easier for hard‑to‑reach spots |
For most people, a Topical antifungal cream, lotion or shampoo applied directly to the skin works fine. Oral medication is reserved for widespread patches, recurrence, or when topicals aren’t tolerated.
In addition to medication, lifestyle tweaks-like using a gentle cleanser, avoiding oily sunscreens, and showering after sweating-help keep the fungus in check.
When to See a Dermatologist
Even though the condition is harmless, there are moments when professional help becomes crucial:
- The patches cover more than 20% of your body.
- You notice persistent itching that interferes with sleep.
- Over‑the‑counter treatments haven’t improved the appearance after four weeks.
- You feel overwhelmed by the emotional burden and it starts affecting work or relationships.
A dermatologist can prescribe stronger agents, arrange follow‑up monitoring, and refer you to counseling services if needed.
Putting It All Together: A Real‑World Example
Emily, a 28‑year‑old graphic designer from Sydney, noticed pale patches on her back just before her summer vacation. She felt embarrassed at the beach, avoided posting photos, and began skipping client meetings because she worried about looking “different.” After a quick skin check‑up, her doctor confirmed tinea versicolor and prescribed a selenium sulfide shampoo plus a short course of fluconazole. Within three weeks, the patches faded, and Emily started a daily mindfulness routine to manage lingering anxiety. She also joined a local support group where members shared tips on choosing non‑oil‑based sunscreens. By the next holiday, her confidence was back and the condition stayed in remission.
Emily’s story shows how a clear medical plan, combined with emotional support, can flip the script from shame to empowerment.

Frequently Asked Questions
Can tinea versicolor spread to other people?
No. The fungus lives on everyone's skin naturally; an overgrowth is a personal internal imbalance, not a contagious infection.
How long does it take for the skin colour to return to normal after treatment?
The antifungal clears the fungus within a few weeks, but the pigment may take an additional 2‑4months to fully rebalance, especially after sun exposure.
Is there a permanent cure?
Because Malassezia is a normal part of skin flora, it can recur under the right conditions. Ongoing skin‑care habits and occasional maintenance shampoos help keep it at bay.
Should I avoid the sun while I have patches?
Limited sun can actually help the patches blend better, but prolonged exposure may darken surrounding skin, making the contrast sharper. Use a non‑oil‑based sunscreen and limit intense midday sun.
Can stress make tinea versicolor worse?
Yes. Stress hormones increase oil production, creating a richer environment for the fungus. Managing stress can therefore reduce flare‑ups.



Justin Durden
October 4, 2025 AT 02:21Hang in there you’ll get through this.
Sally Murray
October 9, 2025 AT 07:21The article provides a comprehensive overview of tinea versicolor, yet it stops short of integrating psychosocial metrics with dermatological outcomes.
By framing emotional impact as a calculable score, it invites interdisciplinary discourse between clinicians and mental‑health professionals.
Nevertheless, further empirical validation is required to substantiate the proposed thresholds.
Bridgett Hart
October 14, 2025 AT 12:21It is astonishing how many people treat a benign fungal overgrowth as a catastrophic life crisis. The article exaggerates the emotional burden without providing robust data. Most sufferers experience only mild discomfort that resolves with standard therapy. The cited study from Australia lacks a proper control group and inflates prevalence of anxiety. One should not conflate transient self‑consciousness with clinical depression. The suggested coping strategies are generic and fail to address the underlying dermatological pathology. Moreover, the emphasis on social avoidance perpetuates stigma rather than empowerment. The recommendation to join online forums is a superficial remedy for a superficial problem. Dermatologists routinely prescribe topical antifungals that clear the infection within weeks, rendering prolonged psychological distress unnecessary. Patients are capable of rational self‑assessment without resorting to melodramatic narratives. The article’s tone mirrors a self‑help bestseller rather than an evidence‑based medical review. It would benefit from a balanced discussion of risk‑benefit ratios of oral versus topical agents. The emotional impact calculator is a gimmick that oversimplifies complex affective states. Readers should prioritize clinical consultation over anecdotal calculators. In conclusion, the condition is manageable and does not justify the alarmist language employed herein.
Sean Lee
October 19, 2025 AT 17:21From a mycological standpoint, the overgrowth of Malassezia spp. constitutes a dysbiotic shift that is modulated by lipid biosynthesis pathways.
Targeted inhibition of ergosterol synthesis via azole compounds can restore homeostasis, thereby attenuating both pigmentary disruption and associated neuro‑behavioral sequelae.
Future research should explore the correlation between cytokine profiles and self‑reported anxiety scores in affected cohorts.
Lawrence D. Law
October 24, 2025 AT 22:21While the premise of quantifying emotional distress is intriguing, it is imperative to acknowledge that dermatological conditions, such as tinea versicolor, present a heterogeneous clinical spectrum, and therefore, a one‑size‑fits‑all scoring algorithm, laden with arbitrary weightings, may inadvertently obscure nuanced patient experiences, leading to potential misinterpretation of severity, and consequently, suboptimal therapeutic decisions.
Mary K
October 30, 2025 AT 02:21Hey folks, I totally get how those stubborn patches can mess with your confidence, but remember you’ve got a toolbox of solutions – from gentle shampoos to confidence‑boosting pep talks!
Throw on a breathable tee, slather on a zinc‑pyrithione wash, and strut your stuff – you’re more than skin deep!
Odin Zifer
November 4, 2025 AT 07:21They don’t want you to know the real reason behind the sudden flare ups the media is hiding the link to hidden chemicals in the air
Marisa Leighton
November 9, 2025 AT 12:21Don’t let those patches dictate your narrative – you’ve already taken the first step by learning about the condition, and that knowledge is power!
Stick to a routine, keep stress low, and celebrate every tiny improvement; the journey may be bumpy but you’ve got a whole community cheering you on.
Brennan Keeler
November 14, 2025 AT 17:21It’s absurd to waste time worrying about a fungus that can be wiped out with a simple shampoo – get over it and focus on real issues.
Chelsea Hackbarth
November 19, 2025 AT 22:21Sure thing! The best fix is a selenium sulfide shampoo – it clears up fast 😊👍
Adam Shooter
November 25, 2025 AT 03:21One must consider the ontological implications of pathologizing cutaneous dysbiosis; the reductionist narrative presented herein neglects the epistemic complexities inherent in somatic‑psychic interplay.
Shanmughasundhar Sengeni
November 30, 2025 AT 08:21Honestly this article is a bit too long for what it is just a skin thing you can treat it and move on.
ankush kumar
December 5, 2025 AT 13:21Dear friends, let us embrace an inclusive perspective that recognizes both the biological mechanisms of Malassezia proliferation and the lived experiences of those navigating social spaces with visible skin changes; by fostering open dialogue, sharing practical skin‑care regimens, and cultivating compassionate support networks, we can collectively mitigate the psychological toll while reinforcing the importance of evidence‑based treatment pathways; remember, every small step toward self‑care is a victory worth celebrating.
Cameron White
December 10, 2025 AT 18:21Don't trust the pharma companies, they push treatments just to make money.
Amélie Robillard
December 15, 2025 AT 23:21Oh great, another calculator that tells you how sad you are 😒📉
Fae Wings
December 21, 2025 AT 04:21I hear you, it can feel overwhelming 😔 but you’re not alone :)