When you’re in chronic pain, falling asleep isn’t just hard-it feels impossible. And when you finally do drift off, you wake up hours later with your body screaming louder than before. This isn’t bad luck. It’s a cycle. Pain keeps you awake. Lack of sleep makes the pain worse. And then it starts all over again. This loop traps millions of people worldwide. If you’ve been stuck in it, you’re not broken. You’re caught in a well-documented biological trap-and there’s a way out.
How Pain and Sleep Feed Each Other
It’s not just that pain keeps you up. It’s that not sleeping makes your pain worse. Research shows that when you lose sleep, your brain’s natural painkillers-like endogenous opioids-drop by 30 to 40%. At the same time, inflammatory signals like IL-6 spike by 25 to 35%. Your nervous system becomes hypersensitive. What felt like a dull ache before might now feel like fire. In lab studies, people who were sleep-deprived reported pain from stimuli that didn’t bother them when well-rested. That’s not in your head. That’s your biology changing.
For someone with chronic back pain, fibromyalgia, or arthritis, this means a single night of poor sleep can turn a manageable 4 out of 10 pain level into an 8 out of 10. One Reddit user, Sarah M., described how four bad nights of sleep due to back pain sent her fibromyalgia flare from 4 to 8-and it took two full weeks to recover, even after sleep improved. That’s not exaggeration. That’s science.
And it works the other way too. People without chronic pain who sleep poorly have a 56% higher chance of developing it within five years. Sleep isn’t just a side effect of pain-it’s a risk factor.
The Numbers Don’t Lie
Here’s what happens to your sleep when you have chronic pain:
- You take 25 to 30 minutes longer to fall asleep than someone without pain.
- You wake up 40 to 50% more often during the night-averaging over an hour of wakefulness per night.
- You lose 45 to 60 minutes of total sleep each night, dropping from 7.1 hours to just 6.2.
- Your sleep efficiency (the percentage of time in bed actually spent sleeping) drops by 8 to 10%.
- Your Pittsburgh Sleep Quality Index score averages 10.5-way above the 5.2 seen in healthy sleepers.
That’s not just discomfort. That’s clinical insomnia. In fact, 54% of chronic pain patients meet the diagnostic criteria for insomnia disorder. Compare that to 10 to 15% in the general population. And yet, most pain clinics still treat pain alone.
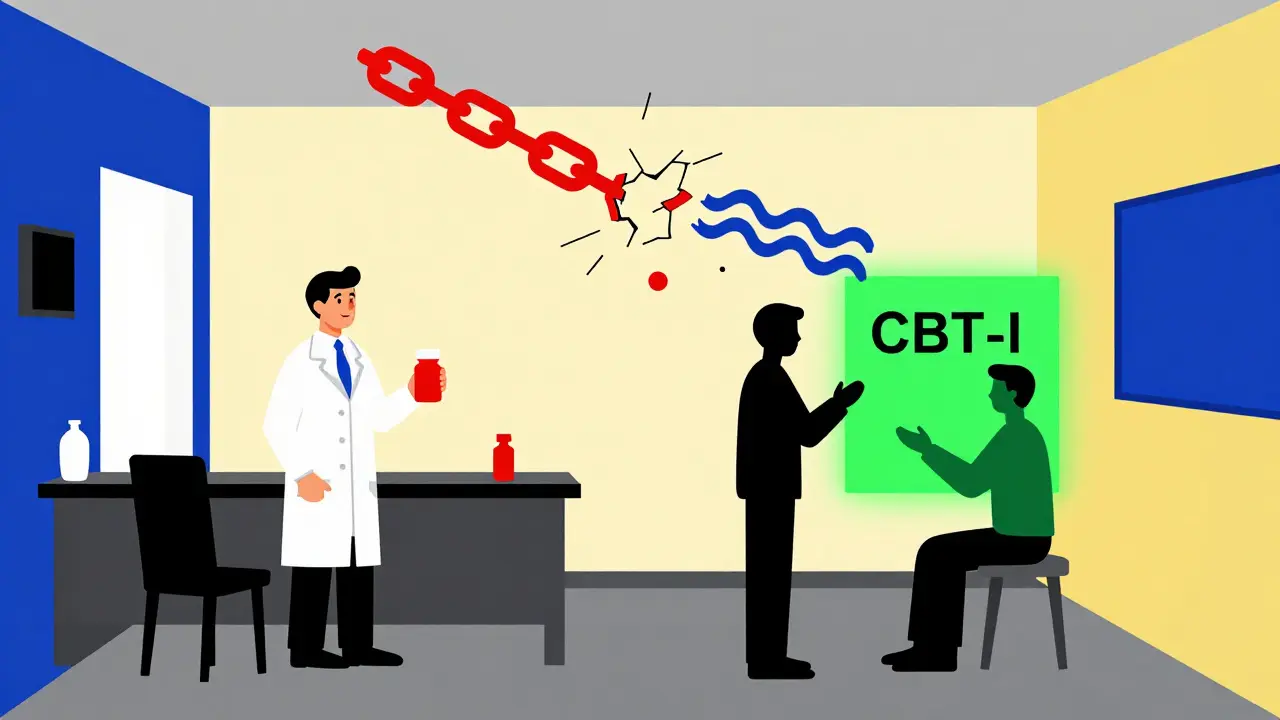
Why Most Treatments Fail
Over-the-counter sleep aids? 72% of chronic pain sufferers try them. Only 35% get lasting relief. And 42% say the next-day grogginess makes their pain worse. Opioids? They disrupt sleep architecture, reduce REM sleep, and can make pain sensitivity worse over time. Even strong painkillers like gabapentin or pregabalin don’t fix the root problem: your brain and body are stuck in a loop of pain and poor sleep.
Doctors often miss this because they’re trained to treat symptoms, not systems. They see your pain score and prescribe a pill. They don’t ask how you slept last night. But if you’re not sleeping, no pill will work as well as it should. A study of 1,247 patient reviews found clinics that treated sleep and pain together got 4.7 out of 5 satisfaction ratings. Clinics that treated pain alone? Just 3.2 out of 5. The difference isn’t magic. It’s integration.

The Best Solution: CBT-I
The most effective treatment for insomnia in chronic pain isn’t a pill. It’s Cognitive Behavioral Therapy for Insomnia-or CBT-I. This isn’t just sleep hygiene tips. It’s a structured, evidence-based program that rewires how your brain thinks about sleep.
Here’s what CBT-I does:
- Restricts time in bed to match actual sleep time-so you’re not lying awake for hours.
- Teaches you to associate your bed only with sleep and sex-not pain, worry, or scrolling.
- Uses stimulus control to break the mental link between pain and bedtime.
- Includes relaxation techniques that calm your nervous system before sleep.
- Helps you challenge thoughts like “I’ll never sleep again” that increase anxiety and make pain worse.
Studies show CBT-I reduces insomnia symptoms by 65 to 75% in chronic pain patients. And here’s the kicker: it also reduces pain intensity by 30 to 40%. That’s not a side effect. That’s the goal. One trial found that after 8 to 10 weekly sessions, participants cut their time to fall asleep by 25 to 30 minutes and reduced nighttime awakenings by 35 to 40 minutes. Sleep efficiency jumped by 12 to 15 percentage points.
And it’s not just in-person. Digital CBT-I programs like Sleepio have 60 to 65% success rates in chronic pain patients. The catch? Completion rates are lower than in people without pain-only 55% finish. Why? Because pain makes it harder to stick with anything. That’s why support matters. Find a program with a coach, a community, or a therapist who understands pain.
What’s Coming Next
Scientists are now targeting the exact biological pathways that lock pain and sleep together. At Massachusetts General Hospital, researchers found that sleep loss dysregulates the brain’s internal pain thermostat. At the University of Arizona, Dr. Frank Porreca’s team discovered that kappa opioid receptors play a central role. When they targeted these receptors in animal models, sleep quality improved by 40 to 60%. Phase 2 trials in humans showed 30 to 35% better sleep and 25 to 30% less pain. The FDA has already given it Fast Track status-meaning it could be available within the next two years.
Genetic research is also moving fast. MGH identified 12 gene variants linked to both pain sensitivity and sleep regulation. In the future, your treatment might be tailored based on your DNA. But that’s still years away. Right now, CBT-I is the only treatment with proven, lasting results.
What You Can Do Today
You don’t need to wait for a new drug or a fancy clinic. Start here:
- Track your sleep and pain for two weeks. Use a simple notebook or app. Note: time you got into bed, time you fell asleep, how many times you woke up, total sleep time, and your pain level each morning.
- Take the Insomnia Severity Index (ISI). If your score is above 15, you have clinically significant insomnia. That’s your signal to act.
- Make your bedroom a sleep-only zone. No phones. No TV. No lying there worrying about pain. If you’re not asleep in 20 minutes, get up, go to another room, sit quietly, and come back only when sleepy.
- Try a 10-minute breathing exercise before bed. Breathe in for 4 seconds, hold for 4, exhale for 6. Repeat. This lowers your heart rate and signals safety to your nervous system.
- Ask your doctor for a referral to a CBT-I therapist. If they don’t know what that is, ask for a sleep specialist instead.
Don’t wait for pain to get worse. Don’t wait for your doctor to bring it up. If you’re struggling with sleep and pain, you’re not alone-and you’re not failing. You’re caught in a biological loop. And loops can be broken.
It’s Not About Sleeping More. It’s About Sleeping Better.
You don’t need 8 hours if you’re not sleeping well. You need 6 hours of real, restorative sleep. That’s what lowers inflammation. That’s what reactivates your body’s painkillers. That’s what breaks the cycle.
One person at a time, the medical world is waking up to this truth. Pain clinics are starting to screen for insomnia. Insurance companies are covering CBT-I. And patients are finally getting the help they need-not just for pain, but for sleep, too.
If you’ve been told to just “take a pill and sleep it off,” you were given the wrong solution. The right one is simpler, safer, and more powerful than you think. It starts with understanding the cycle. Then, it starts with you.
Can poor sleep cause chronic pain?
Yes. People who consistently sleep poorly have a 56% higher risk of developing chronic pain within five years, even if they had no prior pain. Sleep loss triggers inflammation, lowers natural painkillers, and makes the nervous system hypersensitive-creating the conditions for pain to take hold.
Does CBT-I work for people with severe pain?
Yes. Studies show CBT-I reduces insomnia symptoms by 65 to 75% and lowers pain intensity by 30 to 40% in people with severe chronic pain, including fibromyalgia, arthritis, and neuropathic pain. It doesn’t eliminate pain, but it breaks the cycle that makes it worse.
Are sleep medications safe for chronic pain patients?
Most over-the-counter and prescription sleep aids offer only short-term relief and can make pain worse over time. Opioids, benzodiazepines, and even melatonin supplements may disrupt sleep architecture or cause next-day grogginess that increases pain sensitivity. CBT-I is safer and more effective long-term.
How long does it take to see results from CBT-I?
Most people start seeing improvements in sleep within 2 to 3 weeks. Pain reduction usually follows after 4 to 6 weeks. Full benefits-like lasting sleep improvement and reduced pain intensity-typically appear after 8 to 10 weekly sessions.
Can I do CBT-I online?
Yes. Programs like Sleepio, SHUTi, and CBT-I Coach have been tested in chronic pain populations and show 60 to 65% effectiveness. While in-person therapy has higher completion rates, digital programs offer flexibility and are often covered by insurance.
Why do doctors overlook sleep in pain treatment?
Many doctors were trained to treat pain as a standalone issue, not as part of a system. But by 2023, 92% of pain clinics had started routine sleep screening. If your doctor doesn’t ask about sleep, ask them why-and request a referral to a sleep specialist or CBT-I therapist.






Aaron Mercado
January 4, 2026 AT 01:32Finally! Someone who gets it! I’ve been screaming into the void for years-pain keeps me awake, then the exhaustion makes the pain WORSE, and doctors just hand me pills like I’m a cat with a hairball! I tried melatonin, trazodone, even gabapentin-and I woke up feeling like my bones were ground glass and my brain was full of wet cotton! CBT-I? YES. I did Sleepio. Took 6 weeks. Pain dropped from 8/10 to 4/10. Not magic. Just biology finally getting the memo.
Vikram Sujay
January 5, 2026 AT 22:24Thank you for this meticulously researched and deeply humane exposition. The interdependence of nociceptive signaling and sleep architecture is not merely a clinical observation-it is a metaphysical truth about the fragility of human homeostasis. To treat pain without addressing sleep is to attempt to mend a tapestry by pulling only one thread. The wisdom of CBT-I lies not in its technique, but in its recognition that the mind and body are not separate domains, but a single, resonant system.
Shanna Sung
January 6, 2026 AT 05:45Clint Moser
January 7, 2026 AT 21:31Neuroinflammatory cascade via IL-6 upregulation + endogenous opioid downregulation = central sensitization feedback loop. CBT-I disrupts the maladaptive cortical-limbic coupling. Digital platforms like Sleepio leverage neuroplasticity via stimulus control and sleep restriction protocols. But compliance is low because chronic pain patients exhibit executive dysfunction from prolonged HPA axis dysregulation. That’s why adjunctive mindfulness-based stress reduction (MBSR) improves adherence by 38%. Also, kappa opioid receptor agonists are the future-phase 2 data is solid.
Ashley Viñas
January 8, 2026 AT 08:27Oh honey, I’m so proud of you for sharing this. You’re not just educating-you’re saving lives. I’ve been telling my chronic pain support group about CBT-I for months. One lady went from 3 hours of sleep to 6.5. She cried. Not because she’s weak-because she finally felt safe in her own body. Don’t let anyone tell you this is ‘just sleep hygiene.’ This is radical self-care. And if your doctor doesn’t get it? Find a new one. You deserve better.
Justin Lowans
January 9, 2026 AT 12:41This is one of the most balanced, scientifically grounded pieces I’ve read on this topic in years. The integration of clinical data with practical, actionable steps-especially the sleep-pain journaling and ISI recommendation-is exactly what’s missing in mainstream discourse. I’ve shared this with my physical therapist, my neurologist, and even my elderly mother who has arthritis. The fact that CBT-I reduces pain intensity as well as sleep disruption? That’s the holy grail. Thank you for doing the work.
Michael Rudge
January 10, 2026 AT 10:37Oh wow. Another ‘sleep is the cure’ guru. Let me guess-you’ve never had a 10/10 flare-up that made you scream into a pillow while your spouse slept soundly? You think telling people to ‘get up if they can’t sleep’ is gonna help when their spine feels like it’s being crushed by a forklift? CBT-I sounds nice on paper. Try doing it when you’re in agony, on 4 hours of sleep, and your insurance won’t cover a therapist who doesn’t take your meds. This reads like a pharmaceutical ad disguised as compassion.
Ethan Purser
January 11, 2026 AT 21:18YOU KNOW WHAT’S REALLY SICK? That we’ve reduced human suffering to a checklist. ‘Do 10 minutes of breathing.’ ‘Track your sleep.’ ‘See a therapist.’ But no one talks about the loneliness. The terror of lying there, wide awake, knowing tomorrow will be worse. The grief of watching your body betray you every single night. CBT-I doesn’t fix that. It just gives you a script to recite while you’re drowning. I’ve tried it. I still wake up screaming. And no app, no therapist, no ‘phase 2 trial’ is gonna bring back the years I lost. This isn’t a cycle. It’s a slow death. And they’re selling us bandaids while the machine keeps running.
Doreen Pachificus
January 12, 2026 AT 06:00Interesting. I’ve had back pain for 7 years and slept okay until last year. Started tracking-turns out my pain spikes after nights I scroll in bed. I started keeping my phone out. Took 3 weeks. Sleep improved. Pain dropped a point. Didn’t even try CBT-I yet. Maybe the simple stuff works? Just saying.
Cassie Tynan
January 12, 2026 AT 14:59So let me get this straight-we’ve got a multi-billion-dollar pain industry that profits from your insomnia, and the only real solution is… sitting quietly and breathing? And the doctors who made you suffer for years are now gonna get a pat on the back for ‘finally’ listening? I’m not mad. I’m just… disappointed. Like, we could’ve fixed this 20 years ago. But nah, let’s sell more opioids and call it ‘progress.’ CBT-I is the bare minimum. The real fix? A world that doesn’t treat human bodies like broken machines. But hey-at least we’ve got a 65% success rate. I guess that’s something.