Drug Black Box Warning Checker
Check if your prescription medication has a black box warning and learn what the FDA requires doctors and patients to know about serious risks. Black box warnings aren't stop signs—they're safety alerts that help you make informed decisions with your doctor.
BLACK BOX WARNING
Medication Name:
Risk:
Who's at Risk:
What this means for you: This warning doesn't mean you should stop taking the medication. Your doctor will monitor you closely if they believe this drug is right for your condition.
Key Actions:
- Discuss with your doctor if you're at risk for this side effect
- Watch for symptoms like
- Follow up as recommended by your healthcare provider
Disclaimer: This tool is for educational purposes only. Always consult your healthcare provider about your specific medication and treatment options.
When you pick up a new prescription, the last thing you expect to see is a bold, black-bordered warning on the label that says your drug could kill you. But for more than 400 medications in the U.S., that’s exactly what’s there. These are called black box warnings-the strongest safety alert the FDA can require. And while they sound scary, they don’t mean you should stop taking the medicine. They mean you need to know exactly what you’re dealing with.
What Exactly Is a Black Box Warning?
A black box warning, officially called a boxed warning by the FDA, is a legal requirement added to a drug’s packaging and patient information leaflet when serious, sometimes deadly, side effects have been confirmed through real-world use. It’s not something the FDA throws in lightly. Before adding one, they need solid evidence-usually from thousands of patients taking the drug over months or years-not just lab tests or small clinical trials. The warning gets its name from the thick black border that surrounds the text, making it impossible to miss. It’s designed to grab the attention of doctors and patients alike. Inside, you’ll find details about the specific risks: things like liver failure, heart attacks, suicidal thoughts, or birth defects. Sometimes it tells you who’s most at risk-like pregnant women, older adults, or people with certain genetic conditions. These warnings aren’t added during drug approval. They come later, after the drug is already on the market. That’s because some dangers only show up when millions of people start using it. For example, a rare side effect might happen in one out of every 10,000 users. In a trial of 500 people, you’d never see it. But once it’s prescribed to millions, the pattern becomes clear.Why Do These Warnings Exist?
The FDA doesn’t use black box warnings to scare people. They use them to save lives. There are four main reasons one gets added:- The drug has been linked to serious or fatal side effects that outweigh the benefits for some people.
- The side effect can be avoided if the drug is used in a specific way-like not mixing it with alcohol or avoiding it in people with certain health conditions.
- The drug is only approved for very limited use-for example, only as a last resort after other treatments failed.
- The drug poses a special danger to certain groups, like children, pregnant women, or the elderly.
Black Box Warnings Aren’t a Stop Sign
This is the biggest misunderstanding: a black box warning doesn’t mean the drug is unsafe. It means it’s powerful-and needs careful handling. Pharmacists and doctors hear this all the time: “I saw the black box warning. Should I stop taking this?” The answer is almost always: not without talking to your doctor first. Many life-saving drugs have black box warnings. Chemotherapy drugs. Immunosuppressants after organ transplants. Some antipsychotics. Even certain birth control pills. These aren’t dangerous because they’re flawed. They’re dangerous because they work so strongly that they can disrupt your body’s natural systems. Dr. Meghan Lehmann, a pharmacist at Cleveland Clinic, puts it plainly: “If a medication you’re taking carries a risk that warrants a black box warning, that doesn’t necessarily mean you shouldn’t take it.” The key is context. Is this drug the best option for your condition? Are there safer alternatives? Have you been screened for risk factors? Your doctor should walk you through this. If they didn’t, ask. Don’t assume they’ve covered it.Who Gets Warned-and Who Doesn’t?
Here’s the problem: the warning is on the label. But patients rarely read it. A 2023 survey found that 78% of patients said they’d want to know about a black box warning before starting a drug. But only 42% remembered their doctor ever discussing it. That’s a huge gap. Many people find out about the warning after Googling their medication-often after a scary symptom pops up. Reddit threads and pharmacy forums are full of people saying, “I just found out my drug has a black box warning. Why didn’t anyone tell me?” Doctors aren’t always the ones to blame. Time is tight. Prescriptions are handed out fast. But that doesn’t make it okay. If your drug has a black box warning, you deserve a conversation. Not just a handout. Ask your doctor:- What’s the specific risk here?
- How likely is it to happen to me?
- What signs should I watch for?
- Are there other options without this warning?
How Are These Warnings Decided?
The FDA doesn’t act on rumors. They rely on real data. Every year, about 1.2 million reports of side effects come into their MedWatch system. These come from doctors, pharmacists, patients, and drug companies. When a pattern emerges-say, five people on the same drug develop sudden liver failure-the FDA investigates. They might ask the drugmaker to run more studies. Or they might review existing data from hospitals and insurance claims. If the evidence is strong enough, they contact the company and demand a boxed warning. The company then writes the exact wording. The FDA approves it. Then it goes on every bottle, every insert, every website. And once it’s there? It’s almost impossible to remove. Since 2000, only 12 black box warnings have been taken off entirely. Why? Because the bar for removing one is even higher than for adding it. You need proof the risk is much lower than originally thought-and that’s rare.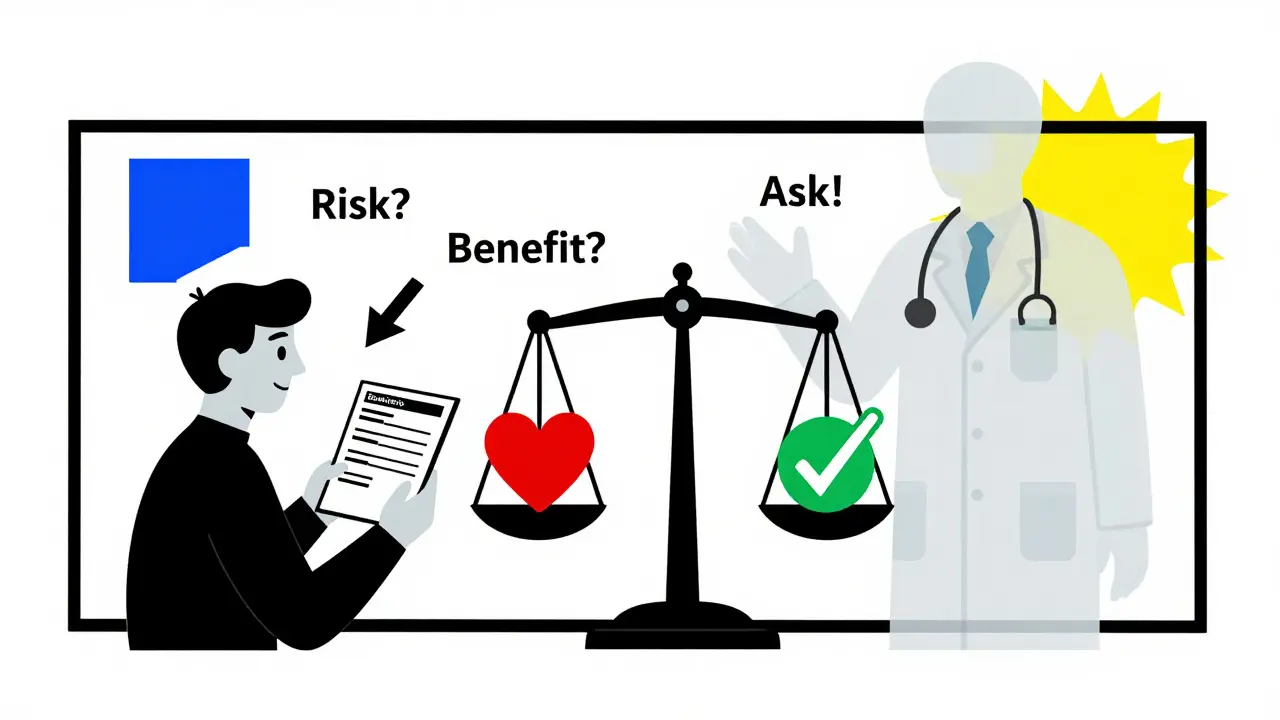
What’s Changing in 2025?
The system isn’t perfect. It’s slow. It’s reactive. But it’s getting better. In 2025, the FDA is rolling out a new AI-powered system to scan health records and pharmacy data in real time. This could cut the time between spotting a danger and issuing a warning from 18 months to just 6-9 months. That’s huge. They’re also testing “dynamic labeling”-digital versions of drug inserts that update automatically when new safety info comes in. Imagine your phone app showing a pop-up: “New warning: this drug may increase stroke risk in people over 70.” No waiting for a new bottle. No missing a recall. And more warnings are coming. Between 2015 and 2023, 45% of all new black box warnings were for cancer drugs or heart medications. That’s not a coincidence. These are high-risk, high-reward treatments. The more we push the limits of medicine, the more we need these alerts.What Should You Do If Your Drug Has One?
Don’t panic. Don’t quit. Do this:- Find the warning. Look at the package insert. Ask your pharmacist for a copy if you don’t have one.
- Identify the risk. What exactly could happen? How often? Who’s most at risk?
- Check your own risk. Do you have the condition that makes this dangerous? Are you on other meds that could interact?
- Ask your doctor: “What are the signs I should call you about?” Write them down.
- Set up a check-in. Schedule a follow-up in 2-4 weeks. Don’t wait for something to go wrong.
Final Thought: Knowledge Is Your Shield
Black box warnings exist because people have died from drugs that were thought to be safe. They’re not punishment. They’re protection. You have the right to know what you’re putting in your body. You have the right to ask questions. And you have the right to be heard when you’re scared. The system isn’t flawless. But when you understand the warning, you’re no longer a passive patient. You’re an active partner in your care. And that’s the best defense you’ve got.Does a black box warning mean I can’t take the medication?
No. A black box warning means the drug carries serious risks, but those risks may still be worth taking if the benefits outweigh them for your specific condition. Many life-saving medications-like chemotherapy drugs, immunosuppressants, and certain antidepressants-have black box warnings. Your doctor should review your individual risks and benefits before prescribing it.
Why didn’t my doctor tell me about the black box warning?
Many doctors assume patients will read the label or that the warning is obvious. But studies show nearly 60% of patients don’t recall being told about it. Time constraints, communication gaps, or assumptions about patient understanding can lead to this oversight. If you didn’t hear about it, ask. It’s your right to know.
Can I switch to a drug without a black box warning?
Sometimes, yes. But not always. Many drugs with black box warnings are the most effective or only option for certain conditions. For example, if you have rheumatoid arthritis and other drugs failed, a drug with a black box warning might be your best shot. Switching isn’t always safer-it might mean worse symptoms or no relief at all. Talk to your doctor about alternatives, but don’t assume a warning-free drug is automatically better.
Are black box warnings the same in Australia and other countries?
No. Black box warnings are a U.S. FDA-specific system. Other countries, including Australia, use different formats-like “contraindications,” “precautions,” or “serious adverse reactions” in their product information. The risks might be similar, but the labeling style and regulatory process differ. Always check your local drug information, especially if you’re traveling or getting medication from overseas.
How long after a drug is approved does a black box warning usually appear?
There’s no fixed timeline. Some warnings appear within a year; others take a decade. It depends on how often the side effect occurs and how quickly it’s detected. For rare reactions-like one in 10,000 patients-it can take years for enough cases to pile up. Newer drugs are especially likely to get warnings later, because they haven’t been used widely enough to reveal hidden risks.
Can I report a side effect if I think it’s related to a black box warning?
Yes. In the U.S., you can report side effects directly to the FDA’s MedWatch program, either online or by phone. In Australia, you can report to the Therapeutic Goods Administration (TGA). These reports help the FDA and other agencies identify new safety patterns. If enough people report the same issue, it can lead to a new warning or even a label update.





Samar Khan
December 28, 2025 AT 13:21OMG I just found out my antidepressant has a black box warning 😱 I thought it was just a weird label and ignored it. Now I’m crying in the pharmacy aisle. Why didn’t my doctor say anything?! I feel so violated. 🥺
Russell Thomas
December 29, 2025 AT 04:49Oh wow, another ‘trust your doctor’ pep talk. Yeah right. My doctor handed me a script for something with a black box warning like it was a coupon for free coffee. Then he checked his phone. 🤡
And don’t get me started on how the FDA waits until people start dropping like flies before they act. It’s not safety-it’s damage control with a fancy label.
Joe Kwon
December 30, 2025 AT 20:39As a clinical pharmacist, I see this daily. The black box warning isn’t a red flag-it’s a traffic signal. It tells you to slow down, check your surroundings, and proceed with awareness.
Most patients panic because they don’t understand risk stratification. A 0.01% chance of hepatotoxicity isn’t the same as a 10% chance of a headache. Context is everything. The system’s flawed, but the intent? Life-saving. We just need better patient education infrastructure-especially around digital labeling and real-time alerts.
Nicole K.
December 31, 2025 AT 03:16You people are so careless. If a drug can kill you, you shouldn’t take it. Period. My cousin died from something like this. You think you’re smart because you ‘ask questions’? No. You’re just gambling with your life. Stop being so casual about death.
Fabian Riewe
January 1, 2026 AT 01:15Big respect to the folks who wrote this. I had no idea black box warnings were this nuanced. I thought they meant ‘don’t touch this.’ Turns out it’s more like ‘handle with care, know the signs, and talk to your doc.’
My mom’s on a med with one-she’s 72, diabetic, and it’s her only option. We sat down, read the insert together, made a checklist of symptoms to watch for. Now she feels empowered, not scared. That’s what this is really about.
Amy Cannon
January 2, 2026 AT 10:47As someone who immigrated from India and now lives in the U.S., I’ve noticed a stark contrast in how medications are communicated here versus back home. In India, we get a tiny leaflet in Hindi with barely legible print. Here, the warnings are bold, clear, and legally mandated-but still, no one talks about them.
It’s not just the doctor’s fault. It’s the entire system. We treat medicine like a product you buy at Walmart. But when your liver is on the line? That’s not a product. That’s your body. We need to stop rushing. We need to sit down. We need to listen. And yes, I misspelled ‘need’-I’m typing on my phone in the car. But you get the point.
Himanshu Singh
January 4, 2026 AT 06:40Hey, I just got my first black box med last week. Was scared at first. But I looked up the side effects on the FDA site, wrote down the warning signs, and called my doc. He said I’m low risk and gave me a number to call if anything weird happens. Feels better now. Just gotta be pro-active, not paranoid. 😊
Jasmine Yule
January 5, 2026 AT 23:43So Nicole K. thinks we should just avoid all black box meds? That’s not safety-that’s ignorance. You want to live in a bubble? Fine. But don’t shame people who are doing the hard work of understanding their own health.
My husband is on a transplant med with a black box warning. He’s alive because he didn’t listen to fear-mongers. He listened to data. He asked questions. He showed up to appointments. That’s responsibility. Not recklessness. 🙏
Greg Quinn
January 7, 2026 AT 19:50Black box warnings are a mirror. They reflect our society’s relationship with medicine: we want miracles, but we don’t want to pay the price. We want cures, but we don’t want to be told they’re dangerous.
These warnings aren’t about fear. They’re about humility. Medicine isn’t magic. It’s chemistry with consequences. And if we can’t accept that, then we’re not ready for the power we’ve unlocked.
Maybe the real warning isn’t on the label.
It’s in our refusal to see the cost.