PPI Risk Calculator
This calculator helps determine your risk of gastrointestinal bleeding while on dual antiplatelet therapy (DAPT) and whether you should take a proton pump inhibitor (PPI).
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for your heart after a stent or heart attack. But it also means you’re at higher risk for a dangerous gastrointestinal (GI) bleed. About 1 in 20 people on this combo will have a serious GI bleed within the first year. The good news? Adding a proton pump inhibitor (PPI) cuts that risk by nearly a third. But not all PPIs are created equal. And not everyone needs one.
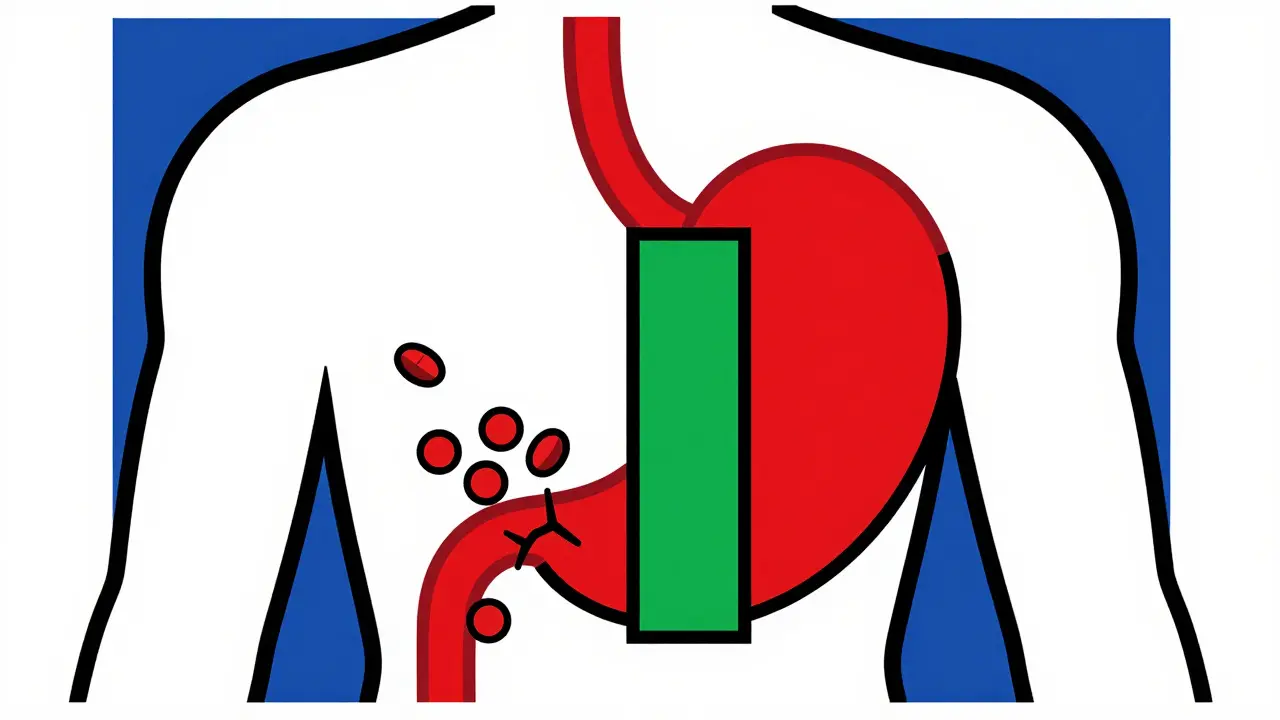
Why GI Bleeds Happen with Antiplatelets
Aspirin and other antiplatelet drugs stop platelets from sticking together. That’s how they prevent heart attacks and strokes. But platelets also help seal tiny tears in your stomach lining. When those drugs are active, even minor irritation from stomach acid can turn into a bleeding ulcer. The risk spikes in the first 30 days after starting therapy, and it doesn’t go away. People over 65, those with a history of ulcers, or anyone taking NSAIDs like ibuprofen or steroids are at even higher risk.Studies show that taking aspirin alone increases GI bleeding risk 2 to 4 times. Add clopidogrel, and that risk jumps another 30-50%. In a 2025 study of nearly 97,000 stroke patients in Korea, those on dual therapy had 325 major GI bleeds over 12 months. The ones who took a PPI had a 37% lower chance of bleeding. That’s not a small benefit - it’s life-saving for some.
Which PPI Works Best - and Why It Matters
Not all proton pump inhibitors are the same. The big difference comes down to how they interact with clopidogrel. Clopidogrel needs to be processed by an enzyme in your liver called CYP2C19 to become active. Some PPIs block this enzyme. If they do, clopidogrel can’t do its job as well.Omeprazole is the most common PPI, and it’s strong at reducing acid. But it also blocks CYP2C19 by about 45%. That means it can reduce clopidogrel’s effect by 30%, which might raise your risk of another heart attack. A 2010 meta-analysis found this interaction could increase cardiovascular events by 27%.
That’s why doctors now prefer pantoprazole or esomeprazole when clopidogrel is part of the mix. Pantoprazole reduces CYP2C19 activity by less than 15%. Esomeprazole barely touches it. Both still cut GI bleeding risk by 34-37%, just like omeprazole - but without weakening your heart protection.
If you’re on ticagrelor or prasugrel instead of clopidogrel, you don’t need to worry about this interaction. Those drugs don’t rely on CYP2C19. So omeprazole is fine here. In fact, it’s often the go-to because it’s cheaper and just as effective.
PPIs vs. H2 Blockers: Why PPIs Win
Some people wonder if famotidine (Pepcid) or ranitidine (Zantac) - the older H2 blockers - can do the same job. The answer is no. A 2017 JAMA Internal Medicine review looked at 12 studies and found PPIs reduced upper GI bleeding by 60%. H2 blockers? Only 30%. The absolute difference? PPIs prevented 1.8% of major bleeds. H2 blockers? Just 0.9%.That’s a big gap. And it’s not just about numbers. In real-world use, PPIs work faster, last longer, and protect the stomach lining more completely. If you’re at risk, an H2 blocker isn’t enough. You need a PPI.
Who Should Take a PPI - and Who Doesn’t Need One
The 2023 European Society of Cardiology guidelines say: give a PPI to anyone on antiplatelets who has two or more of these risk factors:- Age 65 or older
- History of GI bleeding or ulcers
- Taking anticoagulants (like warfarin or apixaban)
- Using NSAIDs (ibuprofen, naproxen)
- Taking corticosteroids (prednisone)
If you have none of these, you probably don’t need a PPI. And here’s the problem: too many people are getting them anyway. A 2022 study found 35-45% of low-risk patients on DAPT were prescribed a PPI unnecessarily. That’s not harmless. Long-term PPI use is linked to higher risks of:
- C. difficile infection (risk up 0.5%)
- Community-acquired pneumonia (risk up 0.8%)
- Chronic kidney disease (hazard ratio 1.20)
- Potential bone fractures with high doses over years
One 2025 JAMA study even looked at dementia risk and found no clear link - but the debate isn’t over. The bottom line: if you’re not at risk, skip the PPI. If you are, take it - but only as long as you need it.
How Long Should You Take It?
Most people on DAPT take aspirin and another antiplatelet for 6 to 12 months. That’s when bleeding risk is highest. So most guidelines recommend PPIs for that same window. After that, if you’re still on aspirin alone, your GI risk drops significantly. You can often stop the PPI unless you have other risk factors.But if you’re on extended DAPT - say, 2 or 3 years because you had a major heart event - then you likely need the PPI longer too. A 2025 Nature article confirmed that the protective effect of PPIs lasts as long as the antiplatelet therapy does. Don’t stop it just because your doctor says “12 months” if your risk profile hasn’t changed.
What About Cost and Access?
Pantoprazole and esomeprazole are available as generics. In Australia, a 30-day supply costs under $10 with a prescription. Omeprazole is even cheaper. The real cost isn’t the pill - it’s the hospital bill from a GI bleed. A single bleeding episode can cost over $20,000 in emergency care, transfusions, and hospitalization. A 2019 study found PPI prophylaxis saves $1,200 per patient per year by preventing these events.And yet, only 16.6% of low-risk stroke patients in Korea got a PPI - even though the data supports it. Meanwhile, in the U.S., 40-50% of DAPT patients get one. That’s not because doctors are better there - it’s because guidelines are clearer and systems are in place to remind them.
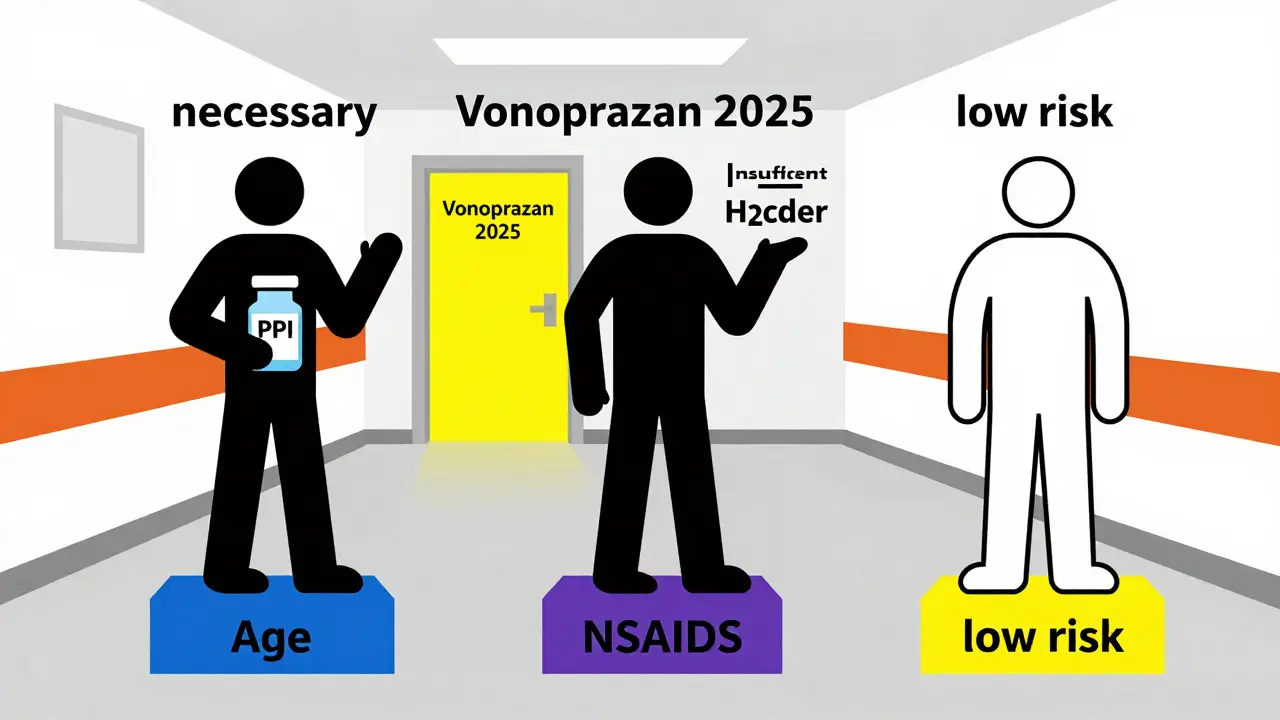
What’s Next? New Drugs on the Horizon
A new class of acid blockers called potassium-competitive acid blockers (PCABs) is coming. Vonoprazan, which is already used in Japan and Europe, works faster and longer than PPIs. Crucially, it doesn’t interfere with CYP2C19 at all. That means it can protect your stomach without weakening clopidogrel. The FDA is reviewing it for U.S. approval in late 2025. If approved, it could replace PPIs for many patients - especially those on clopidogrel.Meanwhile, genetic testing is becoming more common. Some people have a CYP2C19 gene variant that makes clopidogrel less effective. If you’re one of them, your doctor might switch you to prasugrel or ticagrelor - and then you can safely use any PPI. Testing isn’t routine yet, but it’s coming.
What You Can Do Right Now
If you’re on aspirin plus another antiplatelet:- Ask your doctor: Do I have any GI bleeding risk factors? (Age? Past ulcers? NSAIDs?)
- If yes, ask: Should I be on a PPI? Which one? (Ask specifically about pantoprazole or esomeprazole if you’re on clopidogrel.)
- If no, ask: Why am I on this? Is it necessary?
- Don’t take it longer than needed. Reassess at 6-12 months.
- Never stop your antiplatelet without talking to your cardiologist.
It’s not about taking more pills. It’s about taking the right ones - at the right time - for the right reason. PPIs aren’t a cure-all. But for the right person, they’re one of the safest, most effective ways to avoid a life-threatening bleed - without putting your heart at risk.