Starting a new medication can feel overwhelming. You might be relieved it’s finally helping your symptoms, or anxious about what’s coming next. Either way, you’re not alone. Nearly half of all people stop taking their prescriptions too soon-not because they don’t want to get better, but because they didn’t understand what to expect. That’s why asking the right questions before you leave the doctor’s office isn’t just helpful-it’s essential.
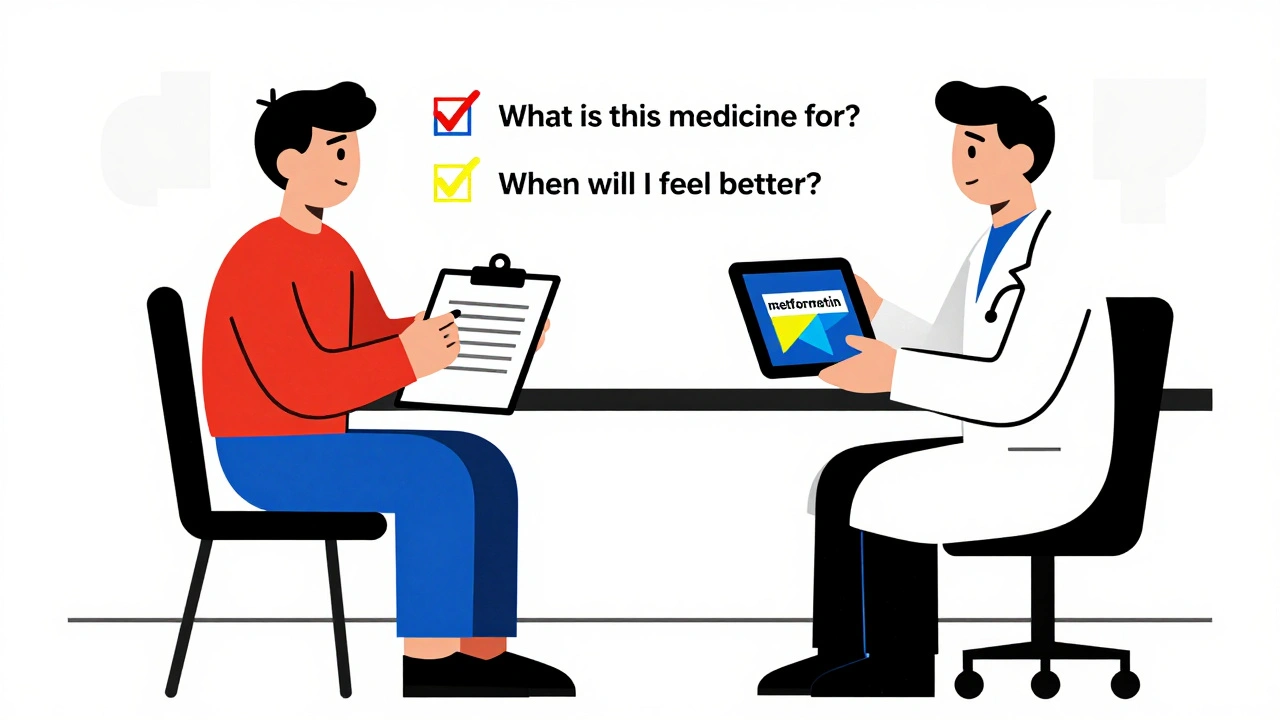
What is this medicine really for?
- What’s the exact name of this medication-both brand and generic?
- What condition is it meant to treat, and how will I know it’s working?
How and when do I take it?
- Do I take it with food, on an empty stomach, or at a specific time of day?
- What’s the exact dose? How many milligrams?
- How long should I take it? Is this short-term or lifelong?
What side effects should I watch for?
- What side effects are normal at first-and which ones mean I should call you right away?
- How long do the common side effects usually last?
- What if they don’t go away?
Will this interact with anything else I’m taking?
- Do I need to tell you about my supplements, vitamins, or over-the-counter drugs?
- Are there foods, alcohol, or activities I need to avoid?
Are there other options?
- Why this drug and not another?
- Is there a cheaper version?
- Could genetic testing help decide what works best for me?
What happens if this doesn’t work?
- When will we check if it’s working?
- What’s the next step if it doesn’t help?
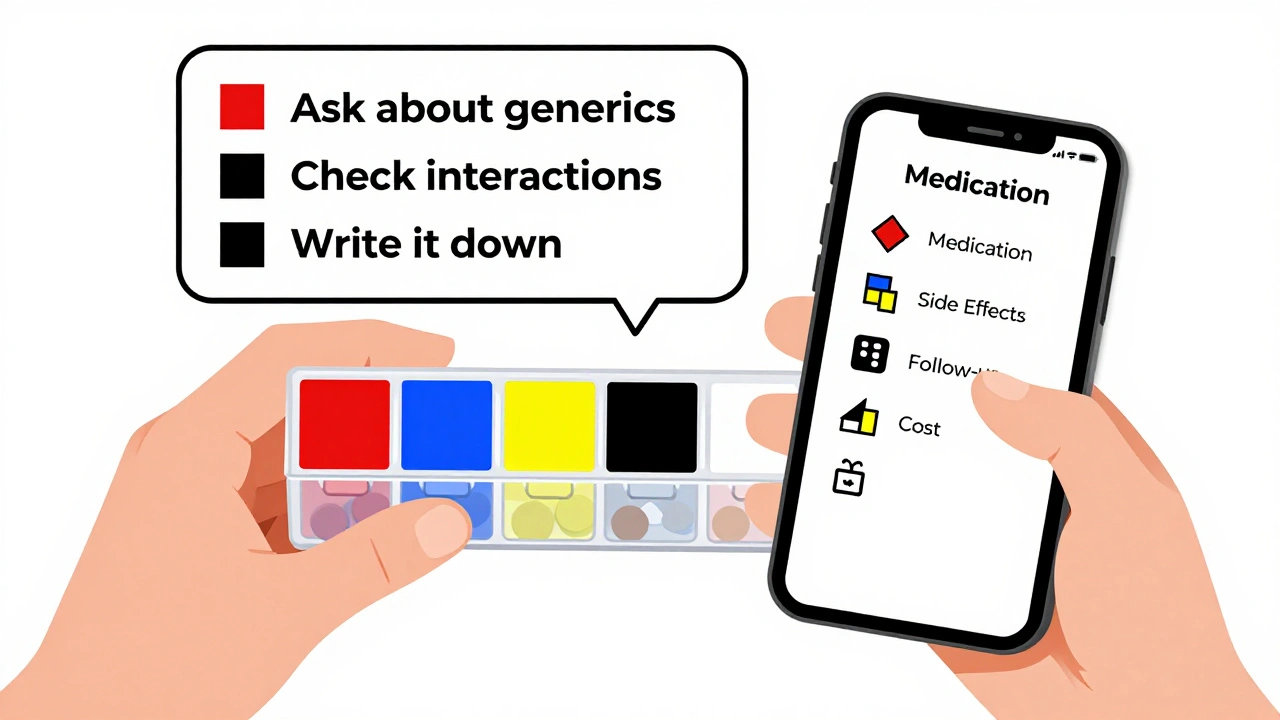
How do I remember all this?
You won’t. Not after a 15-minute appointment. That’s why you need to write it down. Or record it. Or bring someone with you. A University of Michigan study found that patients who wrote down their doctor’s answers remembered 70% more than those who just listened. Use a notebook. Use your phone. Use a free app like MyTherapy or Hero Health. Take a photo of the prescription label. Ask your pharmacist to explain it again when you pick it up. And if your doctor rushes you? Say: I want to make sure I get this right. Can we go over these points one more time? You’re not being difficult. You’re being smart.What if my doctor gets annoyed?
Some doctors are busy. Some are overwhelmed. Some still think patients should just “follow orders.” But the truth? Doctors who welcome questions are the ones who keep patients out of the hospital. A 2023 UCLA study of 10,000 patients showed those who asked at least five of these key questions had 32% fewer bad reactions. That’s not just a win for you-it’s a win for your doctor too. If you feel rushed, try this: “I’ve read that asking these questions helps avoid mistakes. I’d really appreciate your help going through them.” Most providers respond well to that. And if they dismiss you? Consider finding a new one. Your health isn’t negotiable.Final reminder: You’re the boss of your body
Medications are powerful tools. But they’re not magic. They work best when you understand them. When you know what to expect. When you know what to watch for. When you know what to do next. Don’t wait until you feel worse to ask. Don’t wait until you’re scared to speak up. Ask before you leave the office. Write it down. Follow up. Your life depends on it.What if I forget to ask a question during my appointment?
If you forget, call your doctor’s office or pharmacy within 24-48 hours. Most clinics have a nurse line for exactly this. You can also email through your patient portal. Don’t wait until you’re already having side effects. A quick follow-up can prevent a hospital visit.
Can I ask about the cost of my medication?
Absolutely. In fact, you should. One in four people skip doses because they can’t afford their meds. Ask: “Is there a generic version?” “Can I get a 90-day supply to save money?” “Does the drugmaker have a discount program?” Many pharmacies offer $4 generics for common meds like metformin or lisinopril. Don’t assume it’s expensive-ask.
Should I bring a list of all my current meds to every appointment?
Yes. Always. Include prescription drugs, over-the-counter meds, vitamins, supplements, and herbal products. Even if you think it’s “just melatonin” or “just aspirin.” Many dangerous interactions happen because doctors don’t know what you’re taking. Bring the actual bottles if you can. It saves time and prevents mistakes.
Is it okay to stop a medication if I feel worse?
Never stop a prescribed medication without talking to your doctor first. Some meds, like antidepressants or blood pressure pills, can cause dangerous withdrawal symptoms if stopped suddenly. If you feel worse, call your doctor. They might adjust the dose, switch you to another drug, or tell you the side effects will pass. Stopping on your own is riskier than continuing.
What if I’m on multiple medications? How do I keep track?
Use a pill organizer with alarms, or a free app like MyTherapy or Medisafe. Write down each drug, the dose, and the time you take it. Keep a printed copy in your wallet or phone. Many people mix up pills when they’re on five or more meds. A simple checklist prevents dangerous errors.




Ethan McIvor
December 4, 2025 AT 13:57Man, this hit different. I used to just take whatever the doc handed me like a zombie. Then my grandma had a bad reaction to some blood pressure med she didn’t understand. Now I print out the script, write notes in the margins, and even record the doc’s voice on my phone (with permission, obviously). It’s not paranoia-it’s survival.
Also, if you’re on meds long-term, keep a little journal. Not just ‘took pill’, but ‘felt less foggy after 3 days’ or ‘headache worse after wine’. Patterns matter more than you think.
And yeah, if your doc rolls their eyes? Find a new one. Your body isn’t a lab rat.
🙏
Mindy Bilotta
December 6, 2025 AT 07:37just a quick thing: if you’re on metformin, dont drink grapefruit juice. i thought it was just for blood pressure meds but nope, it messes with the gut absorption. also, if you get diarrhea for more than 3 days, call your doc-not wait it out. been there, survived it.
Michael Bene
December 7, 2025 AT 00:30Let me tell you something nobody else will: your doctor doesn’t know jack about your meds. They read the pamphlet for 30 seconds while you’re in the room. The real experts? Pharmacists. They’re the ones who catch the 17 interactions between your antidepressant, your turmeric gummies, your CBD oil, and that ‘natural’ energy drink you swear isn’t a drug.
And don’t get me started on ‘just one glass of wine’. One glass? Sure. But what about the two you had last night? Or the three last weekend? Your liver doesn’t care about your ‘special occasion’. It just sees toxins. And guess what? It’s still processing last week’s meds when you hit it with this week’s booze.
Also, if you’re over 50 and not getting pharmacogenetic testing? You’re playing Russian roulette with your brain. Genomind isn’t sci-fi-it’s science. And if your doc hasn’t heard of it? They’re outdated. Move on.
Stop trusting ‘trust me, I’m a doctor’. Trust data. Trust your body. Trust the pharmacist. Not the guy who’s rushing to lunch.
PS: If you’re taking melatonin and statins? You’re asking for trouble. I’ve seen it. Twice. In the ER. Don’t be number three.
Brian Perry
December 7, 2025 AT 05:00okay so i took my new anxiety med and the first night i felt like i was being slowly eaten alive by bees and i thought i was dying and called 911 and they were like ‘uh… it’s just side effects’ and i was like ‘BUT THE BEES??’
turns out it was just my brain rewiring. but wow. i thought i was gonna die. and now i’m fine. but i still hate that med.
also, i forgot to ask about alcohol. now i drink coffee instead. and i’m okay with that.
ps: if you’re on this med and you feel like you’re turning into a ghost? you’re not crazy. you’re just changing. it gets better. maybe.
Chris Jahmil Ignacio
December 7, 2025 AT 17:40Let’s be real. This whole system is rigged. Big Pharma writes the guidelines. The FDA is a revolving door. Your doctor gets paid bonuses to prescribe certain drugs. You think they care if you live or die? No. They care about their quota.
That 2022 study? It was funded by a drug company. The ‘68% quit early’ stat? It’s designed to scare you into compliance. They want you to stay on it forever. That’s their business model.
And don’t even get me started on pharmacogenetic testing. It’s a scam. They charge $500 to tell you what you already know-that you react badly to meds. Meanwhile, the real solution? Lifestyle. Diet. Sleep. Movement. But they don’t want you to know that because you can’t patent broccoli.
You think your doctor wants you to ask questions? No. They want you to shut up, take the pill, and come back next month for the refill. That’s how the machine works.
Stop trusting the system. Start trusting yourself. Or don’t. But don’t blame me when you end up in the hospital because you followed the script.
Paul Corcoran
December 9, 2025 AT 04:47This is such an important post. Seriously. I used to be the person who just nodded and smiled at the doctor until I ended up in the ER because I didn’t know my blood pressure med made me dizzy when I stood up.
Now I bring a notebook. I write down every question before I go. I even rehearse them in the car. And I always ask for a printed handout or a link to the patient guide.
One thing I wish more people knew: if you’re on more than 5 meds, ask for a med review. Many clinics offer it for free. A pharmacist sits with you and goes through every pill, supplement, and herb. They find duplicates, interactions, and things you don’t even remember taking.
Also, if you’re scared to ask a question? Say this: ‘I want to make sure I’m doing this right.’ That’s all it takes. Most docs are happy to help if you show up prepared.
You’re not a burden. You’re a partner in your care. And that’s powerful.
Colin Mitchell
December 10, 2025 AT 21:37Biggest tip I’ve ever gotten? Always ask ‘What’s the worst that could happen if I don’t take this?’
Not ‘what are the side effects?’-that’s too vague.
‘What’s the worst that could happen if I skip this?’
For my dad’s cholesterol med, it was ‘heart attack in 5 years’. That got his attention.
For my anxiety med, it was ‘chronic insomnia leading to burnout and job loss’. That made me stick with it.
Also, if your doc says ‘it’s fine’ but you still feel weird? Trust your gut. Call back. Write it down. Send an email. You’re not overreacting. You’re being responsible.
And if you’re on meds for depression? Don’t wait 6 weeks to say something. If you feel worse after 2 weeks, call. That’s not weakness. That’s wisdom.
Mark Gallagher
December 12, 2025 AT 03:46What a bunch of woke nonsense. You people are so obsessed with asking questions you’ve forgotten how to follow orders. The doctor knows best. If you don’t like it, go to Canada. Wait, you’re already there. Never mind.
Medications are not optional. They’re not a suggestion. They’re medicine. If you can’t handle taking a pill once a day, maybe you shouldn’t be managing your own health.
And pharmacogenetic testing? That’s for rich people who think they’re special. Your DNA doesn’t make you more deserving of care. Your obedience does.
Stop wasting doctors’ time with your ‘I want to know everything’ nonsense. Just take the pill. Be quiet. Be grateful. That’s what real Americans do.
Also, grapefruit juice? That’s a liberal myth. It’s fine. Just take your pill. Stop overthinking.