Hyperkalemia Risk Calculator
Risk Assessment Tool
This tool estimates your risk of hyperkalemia based on Cleveland Clinic scoring system. Enter your factors to see your risk level and recommended monitoring schedule.
Your Risk Assessment
Recommendations
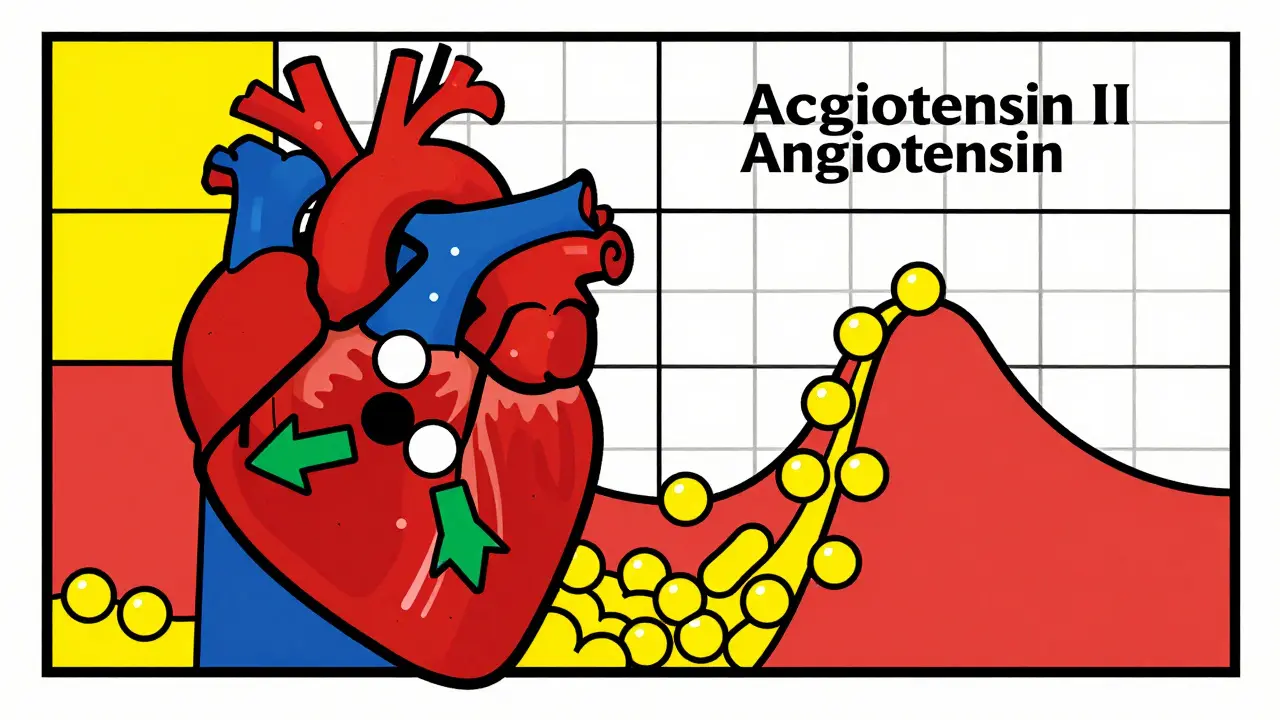
Combining ACE inhibitors and potassium-sparing diuretics is common in patients with high blood pressure, heart failure, or kidney disease. But this mix can push potassium levels dangerously high - a condition called hyperkalemia. And it’s not just a lab result. High potassium can stop your heart. Yet, many people don’t know this risk exists until it’s too late.
Why This Combination Is So Risky
ACE inhibitors, like lisinopril or enalapril, work by blocking a hormone called angiotensin II. That helps lower blood pressure and protects the kidneys. But it also reduces aldosterone - the hormone that tells your kidneys to flush out potassium. Less aldosterone means potassium builds up. Then there are potassium-sparing diuretics: spironolactone, eplerenone, amiloride, and triamterene. These don’t make you pee out potassium like other diuretics. Instead, they block the channels in your kidneys that normally get rid of it. So you keep more potassium - which sounds good if you’re low, but dangerous if you’re already holding onto too much. Put them together? It’s a double hit. Your kidneys get confused. They stop excreting potassium from both ends. The result? Potassium climbs. And fast.Who’s Most at Risk?
Not everyone on this combo develops high potassium. But certain people are sitting on a ticking clock:- People with eGFR below 60 (signs of reduced kidney function)
- Those with diabetes - even mild cases
- Patients with heart failure
- Anyone over 65
- People already starting with potassium levels above 4.5 mmol/L
The Numbers Don’t Lie
Studies show this isn’t theoretical. In one large study, 11% of patients on ACE inhibitors alone developed hyperkalemia. That number jumped to 18.7% when spironolactone was added. Another study found patients on both drugs had 3 to 5 times higher risk than those on ACE inhibitors alone. And it’s not rare. About 5.4 million Americans are on this combination. With an 11% risk rate, that’s over half a million people at serious risk. Most won’t feel symptoms until it’s too late. Fatigue? Muscle weakness? Irregular heartbeat? These are late signs. By then, your heart could be in danger.What Happens When Potassium Gets Too High?
Hyperkalemia is defined as potassium above 5.0 mmol/L. Severe cases are above 6.0 mmol/L. At that level, your heart’s electrical system starts to misfire. You might see:- Palpitations
- Chest discomfort
- Numbness or tingling
- Weakness in arms or legs
- Slow or irregular pulse

Monitoring Is Non-Negotiable
Guidelines are clear: if you’re on this combo, you need blood tests - not just once, but repeatedly.- Test potassium within 1 week after starting
- Check again at 2 and 4 weeks
- Then every 3 to 6 months if stable
- For eGFR under 30? Test weekly at first
What to Do If Potassium Rises
If your potassium hits 5.0-5.5 mmol/L:- Check your diet. Are you eating bananas, oranges, potatoes, tomatoes, or salt substitutes? These are packed with potassium.
- Reduce dietary potassium to under 75 mmol/day (about 3,000 mg). That’s cutting back on most fruits, veggies, and processed foods with potassium additives.
- Consider switching to a thiazide or loop diuretic like hydrochlorothiazide or furosemide. These help flush out potassium.
- Lower the dose of your ACE inhibitor by half and retest in 1-2 weeks.
- Stop potassium-sparing diuretics immediately.
- Consider switching from ACE inhibitor to an ARB (like losartan). ARBs carry a slightly lower risk - about 18% less in some studies.
- Use newer potassium binders like patiromer (Veltassa) or sodium zirconium cyclosilicate (Lokelma). These drugs trap potassium in your gut and let it leave through stool. They let you keep your heart-protecting meds without the danger.
Why So Many People Are Still at Risk
You’d think doctors would follow guidelines. But they don’t. Studies show:- Only 32% of patients with hyperkalemia get dietary counseling
- Just 18% of eligible patients get sodium bicarbonate, which can help lower potassium in those with acidosis
- Only 22% of severe cases get a nephrologist consult
- 33% of patients with potassium above 6.0 mmol/L have no follow-up within 7 days
New Hope: Better Tools and Strategies
The game is changing. New tools are making this combo safer:- SGLT2 inhibitors like dapagliflozin (Farxiga) - originally for diabetes - reduce hyperkalemia risk by 32% in kidney patients on ACE inhibitors. Now they’re being used as a triple therapy: ACE inhibitor + SGLT2 inhibitor + low-dose potassium-sparing diuretic.
- Digital apps that track potassium-rich foods help patients stay within limits. One study showed a 27% drop in hyperkalemia episodes with app use.
- Point-of-care potassium tests are coming soon. In 2026, a handheld device may let you check your potassium at home - no lab needed.
What You Can Do Today
If you’re on this combo:- Ask your doctor: “What’s my potassium level? When was it last checked?”
- Get a list of high-potassium foods. Avoid them. Bananas, oranges, spinach, sweet potatoes, and salt substitutes are big ones.
- Don’t take over-the-counter supplements with potassium - even “natural” ones.
- Keep all follow-up appointments. Don’t skip blood tests.
- If you feel weak, dizzy, or your heart skips beats - get checked immediately.
Bottom Line
ACE inhibitors and potassium-sparing diuretics are powerful tools. Used right, they prevent heart attacks, strokes, and kidney failure. Used without monitoring? They can kill. The key isn’t avoiding the combo. It’s managing it. Test early. Test often. Watch your diet. Use new tools. And never assume it’s safe just because you feel fine.Can I still take ACE inhibitors if I’m on a potassium-sparing diuretic?
Yes - but only with strict monitoring. Many patients safely stay on both medications by getting blood tests every 1-4 weeks, adjusting doses, and watching their diet. The goal isn’t to stop the drugs, but to use them safely. New potassium binders like Veltassa and Lokelma also allow you to keep these life-saving medications even if potassium rises.
How do I know if my potassium is too high?
You won’t feel it until it’s severe. Early high potassium often causes no symptoms. That’s why blood tests are critical. Symptoms like muscle weakness, irregular heartbeat, or nausea appear only when potassium is dangerously high - above 6.0 mmol/L. Don’t wait for symptoms. Get tested regularly if you’re on this combo.
Are there safer alternatives to potassium-sparing diuretics?
Yes. If you need a diuretic and are on an ACE inhibitor, thiazides (like hydrochlorothiazide) or loop diuretics (like furosemide) are safer because they lower potassium. They’re often used in combination with ACE inhibitors for heart failure or kidney disease without raising hyperkalemia risk. Talk to your doctor about switching if you’re at high risk.
Does switching from an ACE inhibitor to an ARB reduce the risk?
Yes, slightly. Studies show ARBs like losartan cause about 18% less hyperkalemia than ACE inhibitors. But the difference isn’t huge. If you’re already on an ACE inhibitor and doing well, switching isn’t always necessary. The bigger issue is combining it with a potassium-sparing diuretic - that’s where the real risk lies, regardless of the class.
Can I eat bananas or potatoes if I’m on these drugs?
Not if you’re at high risk. One banana has about 420 mg of potassium. A medium potato has over 900 mg. The recommended daily limit for people on this combo is under 3,000 mg. Many processed foods also contain hidden potassium additives. Avoid high-potassium foods, salt substitutes (like NoSalt), and herbal supplements. Talk to a dietitian to plan safe meals.
Why don’t doctors test potassium more often?
Many don’t follow guidelines. A 2023 study found only 28% of primary care doctors consistently check potassium levels in patients on this combo. Some think it’s unnecessary if the patient feels fine. Others assume the lab will flag it. But labs don’t call you - you need to request the test. Don’t wait. Ask for it.


Jake Moore
January 19, 2026 AT 03:38Just had my potassium checked last week after being on lisinopril + spironolactone for 6 months. It was 5.6. My PCP said, 'We’ll watch it.' No diet talk, no follow-up plan. I had to ask for the potassium binder. Don’t trust your doctor to catch this. You gotta be your own advocate.
Dayanara Villafuerte
January 20, 2026 AT 02:51banana = death in a yellow peel 🍌💀
Just kidding… sort of. I swapped my daily smoothie for low-potassium berries and my numbers dropped 0.8 in 3 weeks. Also, stop using salt substitutes. They’re basically potassium bombs. Veltassa saved my life. No, I’m not sponsored. Just alive.
Joni O
January 21, 2026 AT 21:52my grandma’s on this combo and she’s 78 with eGFR 42. she didn’t know any of this until i printed out this post and sat her down. she’s now using a food tracker app and checking her potassium every 2 weeks. she says she feels less tired. small wins, y’all.
Robert Davis
January 22, 2026 AT 19:42So let me get this straight. We’re told to take these meds because they ‘save lives,’ but we’re also told they can kill us if we don’t monitor every single thing? Sounds like a trap. Why aren’t they making a safer version? Why do we have to be medical detectives just to stay alive? This isn’t healthcare. It’s a liability game.
Andrew Qu
January 24, 2026 AT 06:10For those asking about ARBs vs ACE inhibitors - the risk difference is real but small. I’ve switched 3 patients from lisinopril to losartan when potassium crept up. One went from 5.8 to 4.9 in 4 weeks. But the real win? Pairing ARBs with SGLT2 inhibitors. That combo cuts hyperkalemia risk AND improves heart outcomes. It’s the new standard. Ask your cardiologist.
Selina Warren
January 24, 2026 AT 16:39STOP WAITING FOR SYMPTOMS. You think you’re fine because you’re not collapsing? That’s the whole damn problem. Potassium doesn’t knock you out with a sledgehammer - it whispers until your heart forgets how to beat. I’ve seen two patients code on this combo. One was 52, active, vegan. He thought ‘natural’ meant safe. It didn’t. Test. Now. Don’t wait for your obituary to be written by a nurse who’s tired of cleaning up after preventable disasters.
Stacey Marsengill
January 24, 2026 AT 21:38Oh, so now I’m supposed to count potassium like it’s calories? I’m supposed to avoid potatoes, bananas, tomatoes, spinach, and salt? What am I supposed to eat? White bread and water? And who’s gonna pay for Veltassa? $1,200 a month? My insurance said ‘no’ twice. So now I’m just supposed to stop my meds? Thanks for the life-saving advice, Dr. Google.
kenneth pillet
January 26, 2026 AT 07:39just got my labs back. 5.2. doc said ‘we’ll recheck in 3 months.’ i asked for a referral to a dietitian. he looked at me like i asked for a unicorn. i’m going to a free clinic next week. don’t wait for them to care.
Naomi Keyes
January 28, 2026 AT 06:36According to the 2023 ACC/AHA Guidelines, Section 4.7.2, all patients on dual RAAS blockade with concomitant CKD or diabetes must undergo serial potassium monitoring within 7 days of initiation, with documented clinical decision-making regarding dietary modification and/or pharmacologic intervention. Failure to comply constitutes a deviation from the standard of care and may constitute negligence. Please consult your provider immediately.
Eric Gebeke
January 29, 2026 AT 00:56My husband’s on this combo. He’s 69, diabetic, eGFR 48. We’ve been doing everything right. Blood tests every 3 weeks. No bananas. No salt substitute. But last week, his potassium was 5.9. They admitted him. He got IV insulin, kayexalate, and a new prescription for Lokelma. He’s fine now. But here’s the truth: the system didn’t protect him. We did. If you’re on this combo, you’re not a patient. You’re a soldier. And the battlefield is your kitchen, your pharmacy, and your doctor’s office.