Anticoagulation: What It Is, Why It Matters, and How Medications Keep You Safe
When your blood clots too easily, it can block arteries or veins and trigger a stroke, heart attack, or pulmonary embolism. That’s where anticoagulation, the medical process of preventing harmful blood clots using drugs. Also known as blood thinning, it’s not about making blood watery—it’s about carefully tipping the balance so clots form only when they’re needed, like after a cut, and not inside your heart or lungs. People with atrial fibrillation, deep vein thrombosis, artificial heart valves, or a history of clots rely on this daily. It’s not optional. Skip a dose, and your risk jumps. Take too much, and you could bleed internally. There’s no middle ground.
Anticoagulation isn’t one-size-fits-all. warfarin, a vitamin K antagonist that’s been used for decades and requires regular blood tests is still common, but newer drugs like rivaroxaban, a direct oral anticoagulant that works without frequent monitoring are now preferred for many. These don’t need weekly INR checks, but they still carry risks—especially if mixed with other meds. For example, taking cimetidine, a common heartburn drug with certain anticoagulants can spike drug levels and lead to dangerous bleeding. That’s why knowing your full medication list matters as much as the anticoagulant itself.
Anticoagulation also ties into how your body handles other conditions. If you’re on steroids, your clotting risk can shift. If you have kidney disease, some anticoagulants need dose changes. Even something as simple as switching from brand to generic can cause confusion if you’re not tracking the exact drug and dose. That’s why questions like "What happens if I miss a pill?" or "Can I take ibuprofen?" aren’t just minor concerns—they’re life-or-death conversations with your doctor. The posts below cover real cases: how drug interactions like dofetilide and cimetidine can trigger deadly rhythms, how kidney function affects metformin and anticoagulants alike, and why double-dosing on blood thinners is one of the most common preventable errors at home. You’ll also find guidance on managing anticoagulation while traveling, during surgery, or when dealing with other chronic illnesses. This isn’t theory. It’s what people actually deal with every day.
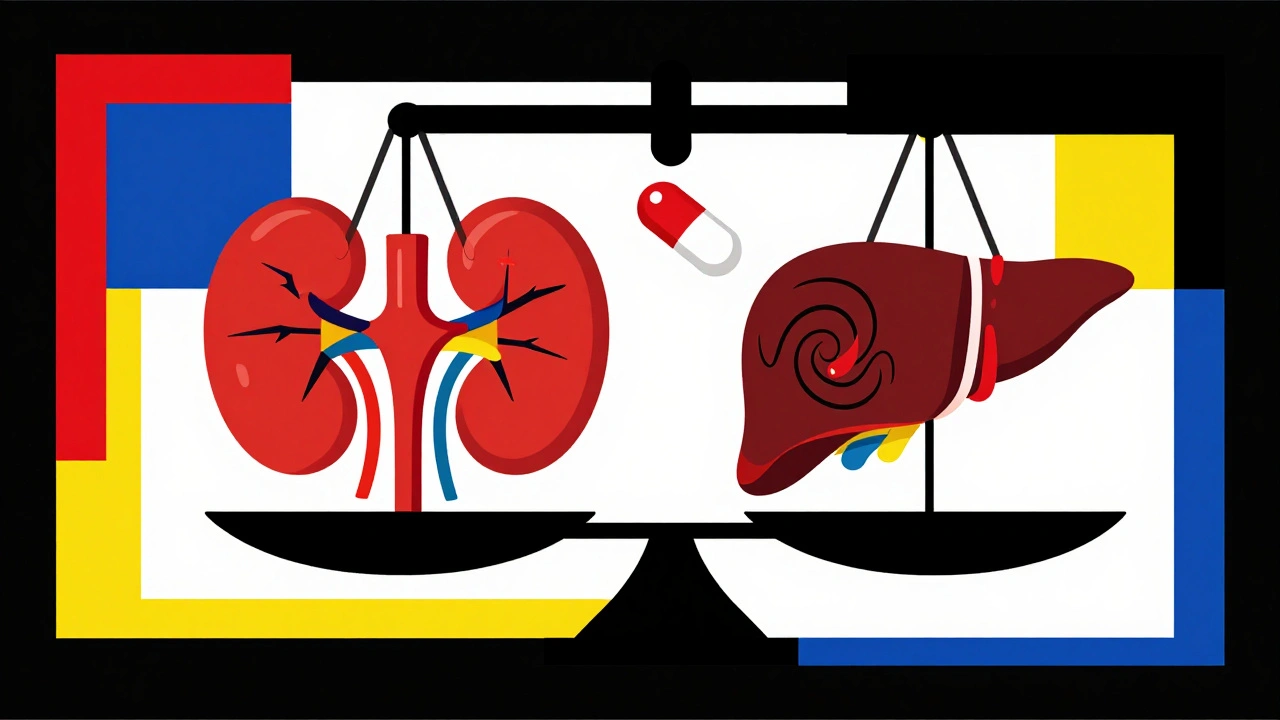
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Dec 4 2025 / MedicationsManaging blood thinners in kidney and liver disease is complex. Apixaban is often the safest option, but decisions depend on kidney function, liver stage, platelet counts, and bleeding history. No guidelines cover all cases-so what doctors do matters most.
VIEW MORE