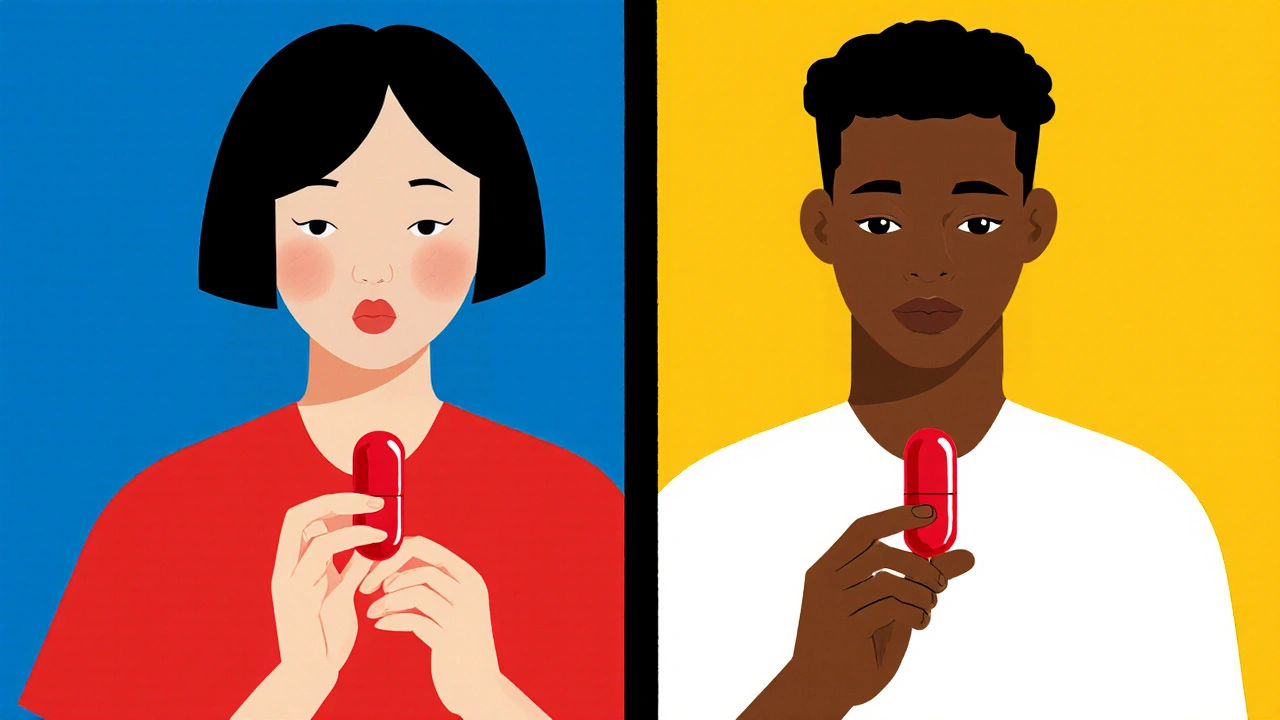
Ethnicity and Drug Response: How Genetics Influence Medication Effectiveness
When you take a pill, it doesn’t work the same way for everyone. ethnicity drug response, how different populations react to medications based on genetic variations tied to ancestry. Also known as pharmacogenetics, it explains why a dose that helps one person might do nothing—or cause harm—to another. This isn’t about stereotypes. It’s about DNA. Studies show that people of African descent often need higher doses of certain blood pressure drugs like beta-blockers because of how their bodies metabolize them. Meanwhile, East Asian populations frequently experience stronger side effects from the blood thinner warfarin, requiring much lower starting doses. These aren’t random quirks. They’re biological patterns rooted in centuries of genetic evolution.
pharmacogenetics, the science of how genes affect drug reactions is turning medicine from guesswork into precision. For example, the drug abacavir, used for HIV, can trigger a life-threatening reaction in people with the HLA-B*5701 gene variant—common in people of European descent but rare in others. Doctors now test for this before prescribing. Similarly, clopidogrel, a heart drug, doesn’t work well in about 30% of people of East Asian background because of a genetic variation that blocks its activation. That’s why some clinics now screen patients before choosing treatments. And it’s not just about race—it’s about ancestry, migration, and inherited biology. Even within broad ethnic groups, there’s wide variation. A person of Mexican heritage may have different genetic markers than someone from Nigeria, even if both are labeled "Hispanic" or "Black" in medical records.
personalized medicine, tailoring treatments to an individual’s genetic profile is the future, but we’re already living part of it. The FDA now includes pharmacogenetic information in over 200 drug labels. Some antidepressants, like SSRIs, show clear differences in effectiveness between Caucasian and Asian patients. Pain meds like codeine work poorly in people with a slow-metabolizer gene found more often in North Africans and Middle Easterners. Even common drugs like statins or metformin show different outcomes across ethnic groups. This isn’t about excluding people—it’s about giving them the right dose, the right drug, the first time.
What you’ll find in the posts below aren’t abstract theories. They’re real-world guides on how these differences show up in practice—from antibiotics that work better in one group to painkillers that backfire in another. You’ll see how doctors are adjusting prescriptions, how labs are catching risks before they happen, and why one-size-fits-all medicine is outdated. This isn’t just science. It’s safety. It’s effectiveness. It’s your health.
Ethnicity & Drug Response: Key Genetic and Metabolic Differences
Oct 26 2025 / MedicationsExplore how genetic and metabolic differences across ethnic groups shape drug response, key enzymes, clinical guidelines, and future steps toward true precision medicine.
VIEW MORE