Glucocorticoid Blood Sugar: How Steroids Raise Glucose and What to Do
When you take glucocorticoid, a class of steroid medications used to reduce inflammation and suppress immune responses. Also known as corticosteroids, it works by mimicking cortisol, your body’s natural stress hormone. But this same mechanism can disrupt how your body handles sugar, leading to high blood glucose—even if you’ve never had diabetes before.
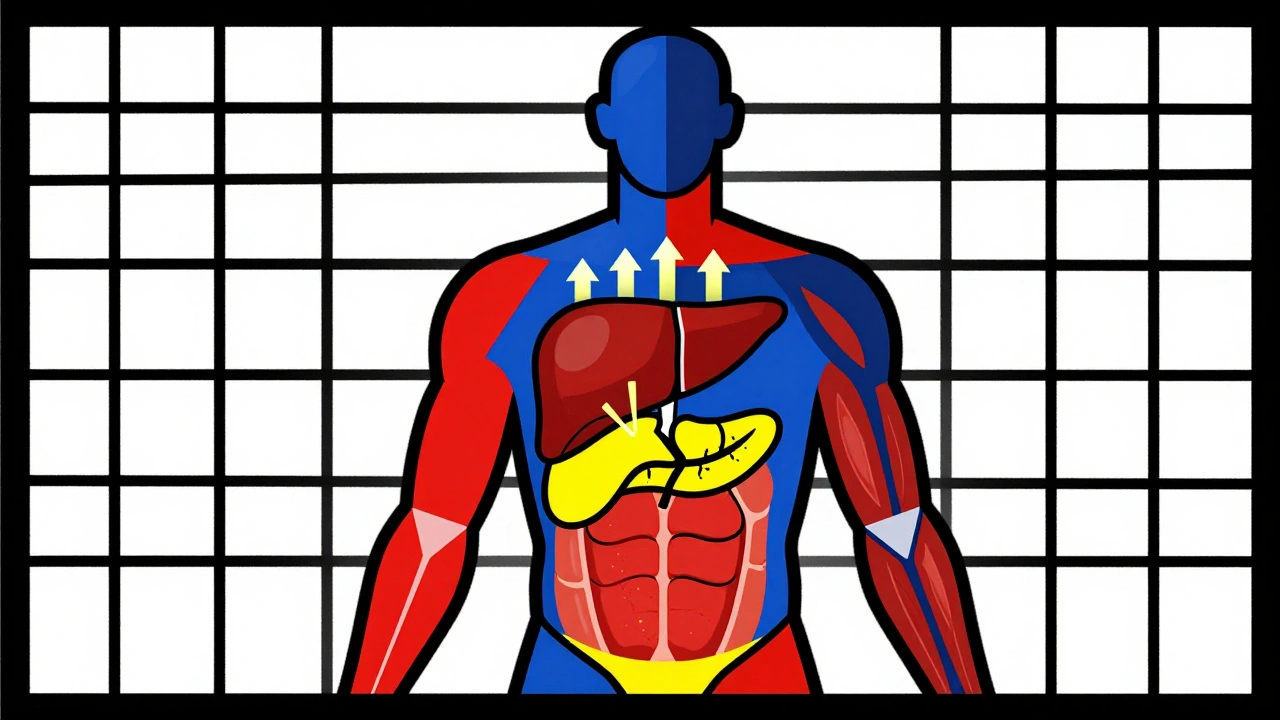
This isn’t just a side effect—it’s a well-documented metabolic shift. corticosteroids, including prednisone, dexamethasone, and hydrocortisone tell your liver to dump more glucose into your bloodstream. At the same time, they make your muscles and fat cells less responsive to insulin, a condition called insulin resistance, when cells stop reacting properly to insulin’s signal to absorb sugar. The result? Blood sugar climbs. People on long-term steroid therapy often see fasting glucose rise above 126 mg/dL, the threshold for diabetes. Even short courses, like a 5-day prednisone taper, can trigger noticeable spikes in sensitive individuals.
It’s not just about diabetes. People with prediabetes, older adults, those with obesity, or a family history of type 2 diabetes are at higher risk. But even healthy people can develop steroid-induced hyperglycemia. The key is awareness. If you’re prescribed glucocorticoids for asthma, rheumatoid arthritis, or an autoimmune flare, ask your doctor about monitoring your blood sugar. Some will check fasting glucose before and after starting treatment. Others may recommend home testing, especially if you’re on more than 20 mg of prednisone daily for over a week.
Managing this isn’t about avoiding steroids when they’re medically needed—it’s about working with your care team to balance benefits and risks. You might need a temporary adjustment to your diet, more frequent movement, or even a short course of metformin. In some cases, insulin is the safest option. The goal isn’t to stop the steroid—it’s to keep your blood sugar from going too high, which can lead to dehydration, confusion, or even hospitalization.
What you’ll find below are real-world insights from doctors and patients who’ve dealt with this issue. From how to spot early signs of high blood sugar on steroids, to what medications interact with glucocorticoids and make things worse, to how to talk to your doctor about alternatives without sounding alarmist. These aren’t theoretical guides—they’re practical, tested strategies from people who’ve been there. Whether you’re on a short course or long-term therapy, the information here will help you stay in control—without sacrificing the treatment you need.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Dec 1 2025 / MedicationsCorticosteroid-induced hyperglycemia affects up to 50% of patients on high-dose steroids. Learn how to monitor blood sugar, when to start insulin, and why tapering can cause dangerous lows.
VIEW MORE