Insulin for Steroid Diabetes: What You Need to Know
When you take steroids, powerful anti-inflammatory drugs like prednisone or dexamethasone used for conditions like asthma, arthritis, or autoimmune diseases, your body can start acting like it has diabetes, a condition where blood sugar rises because the body can't use insulin properly. This isn't just a side effect—it's called steroid-induced diabetes, a temporary or sometimes long-term form of high blood sugar triggered by steroid use. And when blood sugar stays high, insulin, a hormone your pancreas makes to move sugar from your blood into your cells often becomes the only reliable tool to bring it back under control.
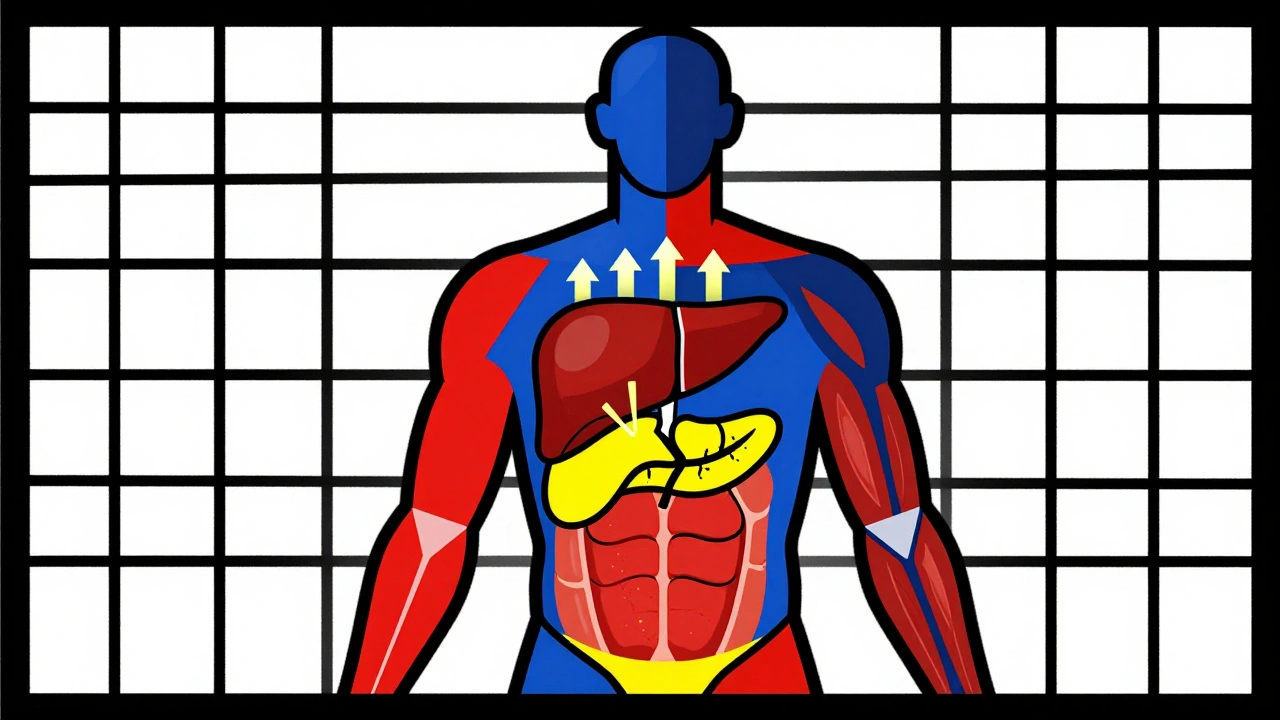
Steroids mess with how your liver releases sugar and how your muscles and fat cells respond to insulin. The result? Blood sugar spikes, especially after meals. Many people don’t realize this is happening until they feel unusually thirsty, tired, or need to pee all the time. If you’re on long-term steroids—say, more than a few weeks—your doctor should check your blood sugar regularly. If it stays above 180 mg/dL, insulin isn’t a last resort. It’s the most direct, effective fix. Unlike oral meds, insulin works fast, doesn’t rely on your pancreas to still make some insulin, and won’t overload your liver or kidneys. That’s why it’s the go-to for steroid diabetes, even in people who never had diabetes before.
People often worry that starting insulin means they’re "really sick" or that they’ll be on it forever. But with steroid-induced diabetes, that’s not usually true. Once you stop the steroids, your blood sugar often returns to normal. Insulin here is a bridge, not a life sentence. Still, you can’t just guess your dose. Too little and your sugar stays high, risking nerve, eye, or kidney damage. Too much and you risk low blood sugar, which can be dangerous. That’s why tracking your levels, timing meals, and working with your doctor to adjust your insulin type and dose matters more than you think.
The posts below show how real people and doctors handle this. You’ll find what works when steroids and blood sugar collide, how to avoid common mistakes with insulin dosing, and why some meds that work for regular diabetes can make steroid diabetes worse. You’ll also see how kidney function, weight, and other meds like diuretics or antipsychotics play into the mix. This isn’t theory—it’s what happens in clinics and homes every day when someone’s on high-dose steroids and their body says, "I can’t handle this alone."
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Dec 1 2025 / MedicationsCorticosteroid-induced hyperglycemia affects up to 50% of patients on high-dose steroids. Learn how to monitor blood sugar, when to start insulin, and why tapering can cause dangerous lows.
VIEW MORE