Progesterone and PCOS: Understanding the Connection
When talking about Progesterone and PCOS, the combination of a key female hormone and a common endocrine disorder that affects up to 10% of women of reproductive age. Also known as Polycystic Ovary Syndrome, it shapes menstrual cycles, weight, and fertility. The body’s hormone orchestra can go off‑beat, and the resulting discord often shows up as irregular periods, unwanted hair growth, or difficulty getting pregnant.
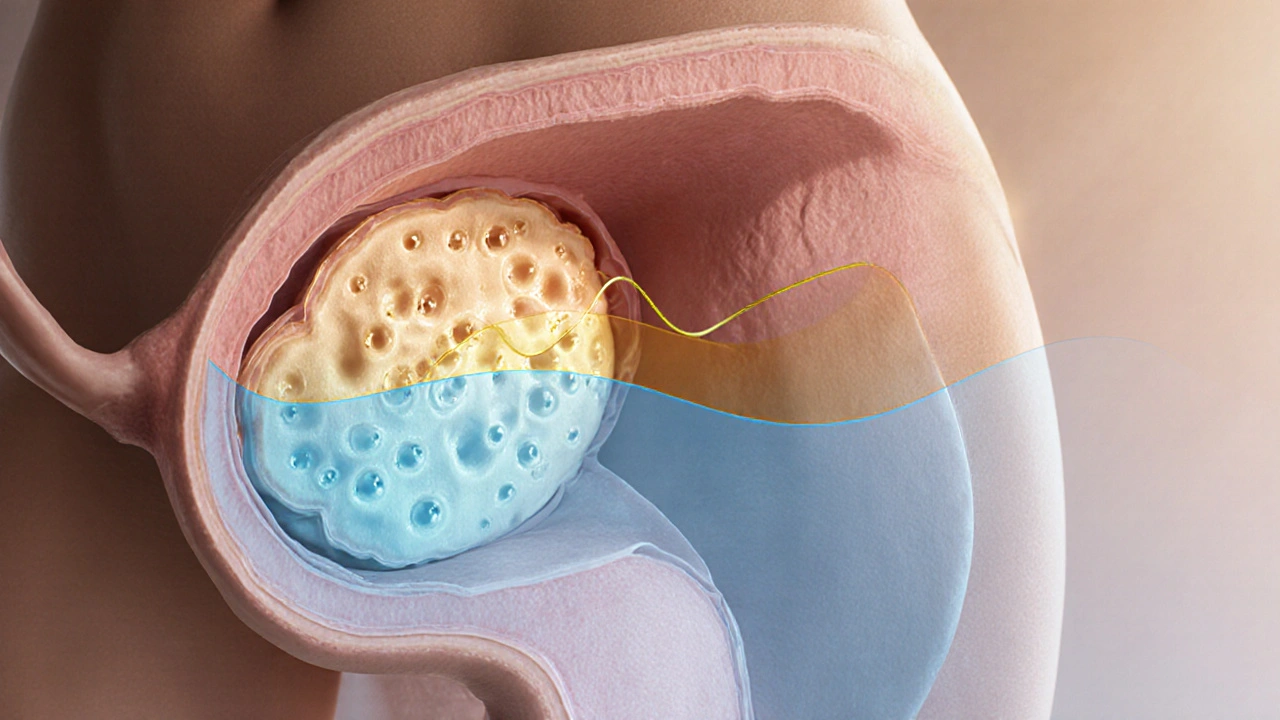
The first player in this story is Progesterone, a steroid hormone produced after ovulation that prepares the uterus for a possible pregnancy and regulates the menstrual cycle. When progesterone levels stay low, the lining of the uterus may not stabilize, leading to spotting or missed periods. The second key piece is PCOS, a hormonal disorder marked by multiple ovarian cysts, excess androgen production, and often insulin resistance. Together they create a feedback loop: low progesterone can worsen PCOS symptoms, and PCOS can keep progesterone from rising after ovulation.
Why Insulin Resistance Matters
Enter Insulin Resistance, the reduced ability of cells to respond to insulin, forcing the pancreas to produce more of the hormone. This metabolic hiccup is a common sidekick of PCOS. When cells resist insulin, the body ramps up insulin production, which can trigger the ovaries to make more androgens. Those excess androgens then suppress ovulation, keeping progesterone low. So the semantic triple looks like this: PCOS influences insulin resistance, insulin resistance drives androgen excess, androgen excess reduces progesterone. Breaking any link in this chain can improve the whole picture.
Lifestyle changes—like low‑glycemic diets, regular strength training, and stress‑reduction techniques—can lower insulin spikes. When insulin levels stabilize, the ovaries receive a calmer signal, ovulation becomes more regular, and progesterone gets a chance to rise. In practice, many women report clearer skin, fewer cravings, and steadier periods after tweaking their carbs and moving more.
Another crucial entity is Fertility, the capacity to conceive and sustain a pregnancy, heavily dependent on balanced hormones and a receptive uterine lining. Low progesterone creates a hostile environment for implantation; the thin lining can’t support an embryo. Conversely, restoring progesterone improves the uterine lining’s thickness, making it more welcoming. The triple here: Progesterone supports fertility, fertility benefits from stable insulin, stable insulin helps maintain progesterone. This interconnectedness shows why a single‑focus approach rarely works—addressing diet, exercise, and possibly medical supplementation together yields the best outcomes.
Medical options also play a role. Doctors may prescribe progesterone supplements, combined oral contraceptives, or insulin‑sensitizing drugs like metformin. Each tackles a different node in the network: supplements boost the hormone directly, contraceptives regulate cycles, and metformin improves insulin response. Choosing the right combo depends on personal goals—whether the priority is symptom relief, menstrual regularity, or preparing for pregnancy.
Below you’ll find a curated set of articles that dive deeper into each of these angles—hormone testing, diet plans, exercise routines, and medication guides. Whether you’re just learning what progesterone and PCOS are or you’re ready to fine‑tune your treatment plan, the collection offers practical steps you can start using right away.
Progesterone Deficiency and Its Impact on PCOS
Oct 2 2025 / Health and WellnessExplore why progesterone often stays low in PCOS, its impact on menstrual health and fertility, and practical lifestyle and medical strategies to restore balance.
VIEW MORE