Reperfusion Injury: What It Is and Why It Matters
Have you ever wondered why restoring blood flow after a heart attack or stroke sometimes causes extra damage? That extra damage is called reperfusion injury. It happens when tissues that were starved of oxygen suddenly get blood back — and the sudden change triggers a harmful chain reaction. Understanding this helps patients and caregivers know what doctors try to prevent when they restore circulation.
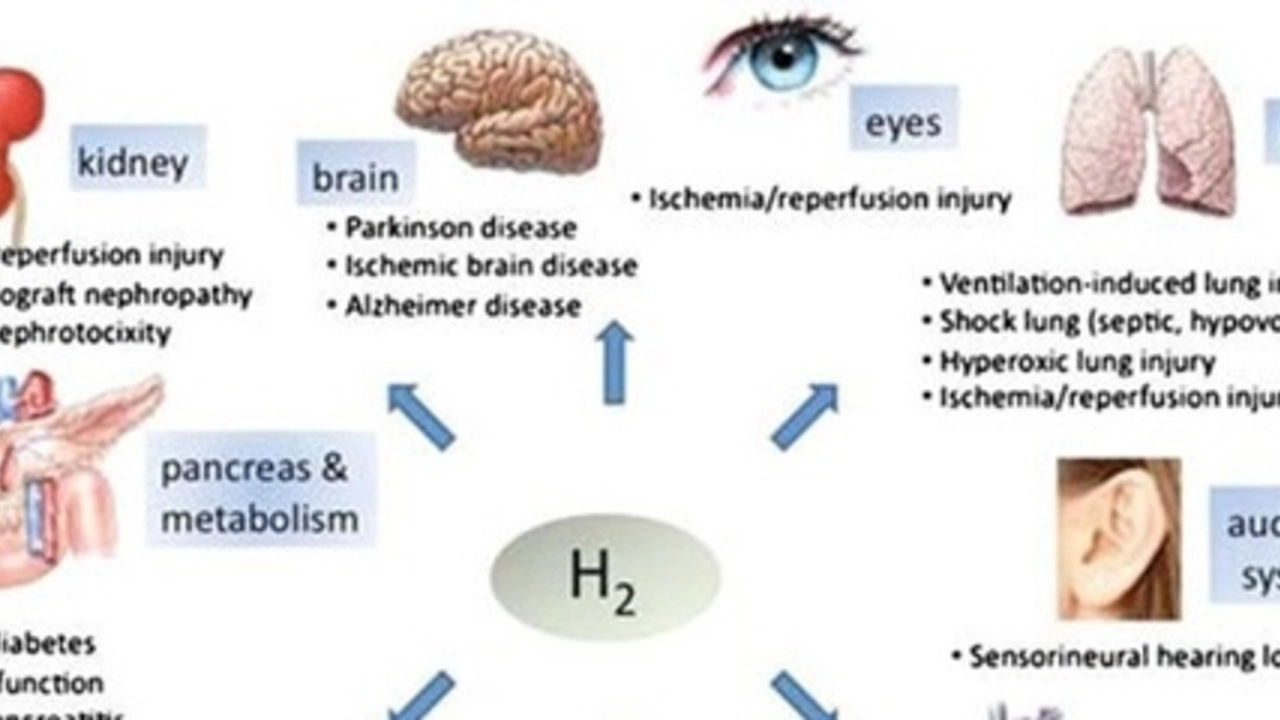
Reperfusion injury is most common after heart attacks, strokes, and some organ transplants. In those situations, blood flow is blocked for a time (ischemia). When blood returns, the tissue faces oxidative stress, sudden calcium shifts, and a burst of inflammation. These processes can kill cells or make recovery worse, even though the initial goal — restoring blood flow — is essential.
How reperfusion injury happens — simple explanation
Think of a dry sponge suddenly soaked with water. Cells that adapted to low oxygen can’t handle the rapid return of oxygen and nutrients. Key steps include: a sudden rise in reactive oxygen species (free radicals) that damage cell parts; overloaded calcium inside cells that breaks cell function; and immune cells rushing in and causing inflammation. All together, these lead to more cell death and swelling than you'd expect from the original lack of oxygen alone.
Where this shows up and what doctors do about it
In the heart, reperfusion injury can expand the area of damage after a blocked artery is opened with angioplasty. In the brain, it can worsen swelling after a clot is removed. During transplants, reperfusion can harm the new organ right after blood flow is re-established. Doctors use several practical strategies to lower the risk: getting blood flow back quickly but carefully, using targeted cooling (hypothermia) after some strokes or cardiac arrests, and applying controlled reperfusion techniques in surgeries.
There are also medical treatments that try to blunt the damaging steps. Antioxidants and drugs that limit calcium overload or block parts of the inflammatory response have been tested. Some techniques used in hospitals are called ischemic preconditioning and postconditioning — short, controlled cycles of reduced and restored blood flow that make tissues more resilient. Not every option works for every patient, and research is ongoing to find reliable drugs that reduce reperfusion harm without blocking the benefit of restored blood flow.
What should patients know? If you or someone you love is treated for a heart attack or stroke, faster treatment usually means better outcomes, even though reperfusion injury is a risk. Ask your care team what steps they take to protect the tissue when they restore blood flow. If you’re preparing for surgery or a transplant, talk about measures to reduce reperfusion damage. The good news: modern medical teams are aware of reperfusion injury and use practical ways to lower its impact while restoring circulation — because saving tissue by bringing blood back is still the first priority.
The Connection Between Reperfusion Injury and Autoimmune Disorders
Jul 6 2023 / Health and MedicineIn my recent research, I've found a fascinating connection between reperfusion injury and autoimmune disorders. Reperfusion injury, which occurs when blood supply returns to tissue after a period of ischemia or lack of oxygen, can trigger an inflammatory response. This can, in turn, lead to autoimmune disorders where the body's immune system attacks its own cells. Simply put, the damage caused by reperfusion can confuse our immune system, causing it to misfire. It's a complex topic, but understanding it could lead to breakthroughs in treating various autoimmune conditions.
VIEW MORE