Steroid Diabetes Monitoring: How to Track Blood Sugar When Taking Steroids
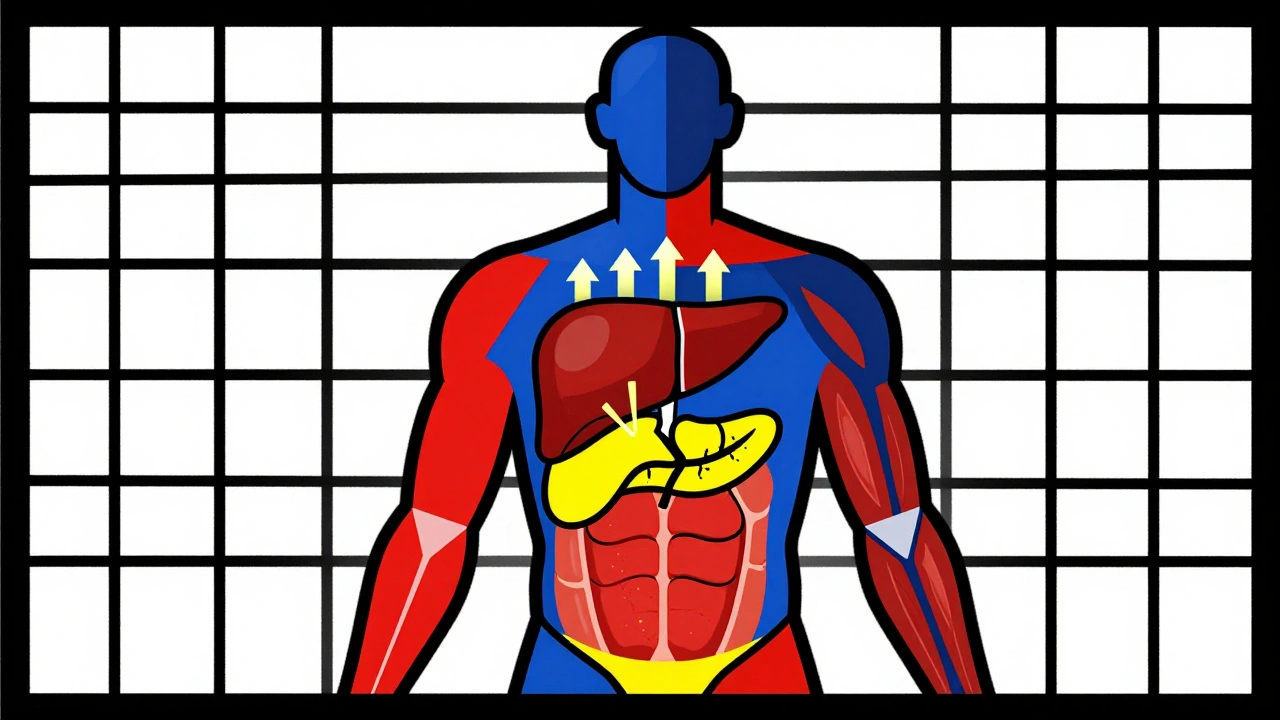
When you take steroids, synthetic hormones like prednisone or dexamethasone used to reduce inflammation and suppress immune responses. Also known as corticosteroids, they can significantly raise blood sugar levels—even in people who’ve never had diabetes before. This isn’t just a side effect; it’s a predictable metabolic shift that needs active monitoring. If you’re on steroids for more than a few days, especially at higher doses, your body may start resisting insulin, causing glucose to build up in your bloodstream. That’s steroid diabetes monitoring—not optional, but essential.
People with existing type 2 diabetes are at higher risk, but even healthy adults can develop high blood sugar after starting steroids. The effect usually shows up within days. You might notice increased thirst, frequent urination, or unexplained fatigue. These aren’t just annoyances—they’re warning signs. Blood sugar control, the process of keeping glucose levels within a safe range through diet, activity, and sometimes medication becomes a daily priority. Many patients are told to check their glucose twice a day with a home monitor, especially before meals and at bedtime. Some end up needing metformin or even insulin short-term while on steroids. The goal isn’t to eliminate the steroids—it’s to manage the spike they cause.
Corticosteroids, a class of drugs used for asthma, arthritis, autoimmune diseases, and organ transplant rejection don’t all act the same. Prednisone is the most common culprit, but even inhaled or topical steroids can affect glucose in sensitive individuals. The higher the dose and the longer the treatment, the greater the risk. That’s why diabetes management, a personalized plan to maintain healthy blood sugar levels through lifestyle and medical support must be adjusted while you’re on these drugs. Your doctor might ask you to log your readings, cut back on carbs, or avoid sugary drinks. Walking after meals can help lower post-meal spikes. Sometimes, you’ll need to see an endocrinologist—not because you have permanent diabetes, but because steroids create a temporary, treatable condition that needs attention.
What you’ll find in the posts below are real-world strategies from people who’ve been there. You’ll learn how to spot early signs of steroid-induced high blood sugar, what tests your doctor should order, how to talk to your provider about adjusting your meds, and what to do when you’re off steroids but your glucose is still off. These aren’t theoretical guides—they’re practical, tested approaches from patients and clinicians dealing with this exact issue every day. Whether you’re just starting steroids or you’ve been on them for months, this collection gives you the tools to protect your health without guessing.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Dec 1 2025 / MedicationsCorticosteroid-induced hyperglycemia affects up to 50% of patients on high-dose steroids. Learn how to monitor blood sugar, when to start insulin, and why tapering can cause dangerous lows.
VIEW MORE