Steroid-Induced Diabetes: Causes, Risks, and What You Can Do
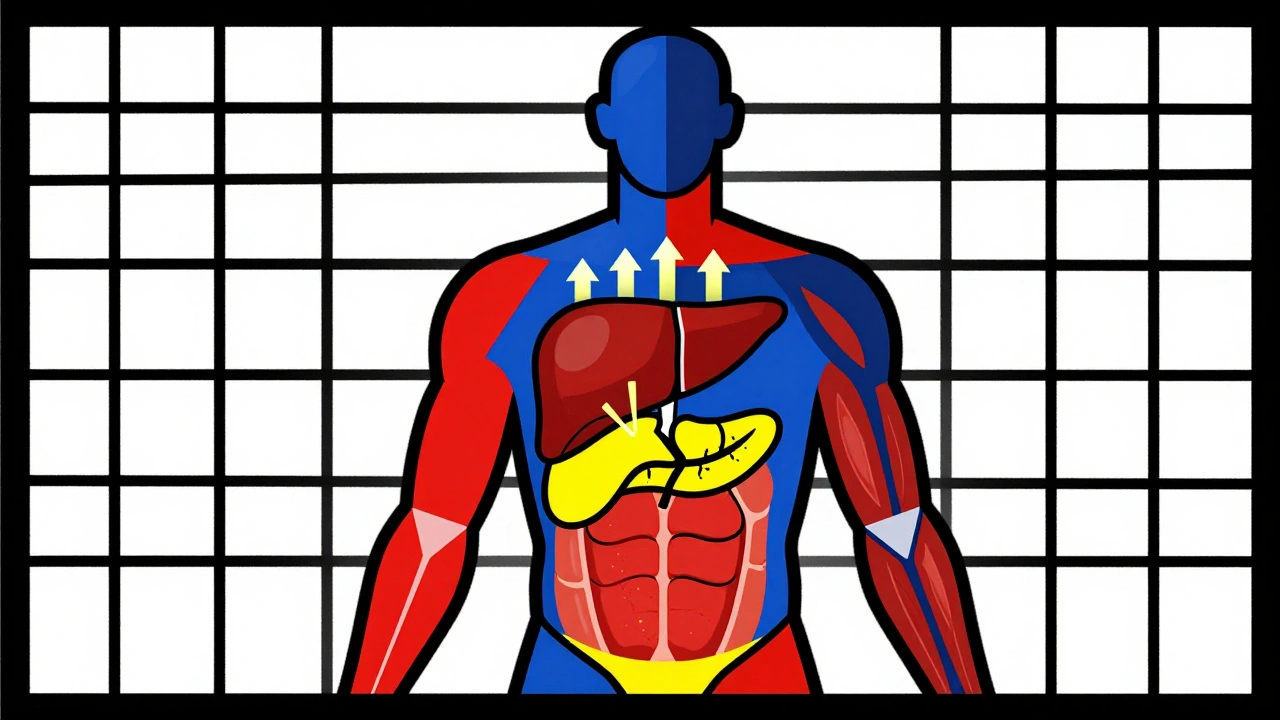
When you take steroid-induced diabetes, a form of high blood sugar triggered by corticosteroid medications. It’s not the same as type 1 or type 2 diabetes—it’s a side effect, not a lifelong condition for most people. This happens because drugs like prednisone, dexamethasone, or methylprednisolone interfere with how your body uses insulin. Your liver pumps out more glucose, and your muscles and fat cells stop responding to insulin like they should. The result? Blood sugar climbs—even if you’ve never had diabetes before.
This isn’t rare. People on long-term steroids for asthma, rheumatoid arthritis, or after an organ transplant often see their numbers rise. Even short courses, like a 5-day pack for a flare-up, can cause spikes. The risk goes up with higher doses, older age, being overweight, or having a family history of diabetes. It’s not your fault. It’s biology. And it’s manageable if you catch it early.
corticosteroids, powerful anti-inflammatory drugs used for autoimmune conditions and severe allergies are the main trigger. But not everyone gets this side effect. Some people’s bodies handle the extra glucose just fine. Others see fasting blood sugar jump from 90 to 180 mg/dL in days. That’s why doctors check blood sugar before and during steroid treatment—especially if you’re on more than 20 mg of prednisone daily for over two weeks.
And it’s not just about sugar. insulin resistance, when cells stop responding properly to insulin, making blood sugar harder to control is the core problem. Your pancreas tries to make more insulin to compensate, but eventually, it can’t keep up. That’s when you need help—diet, exercise, or sometimes even short-term insulin. Stopping steroids often reverses it, but not always. Some people end up with permanent type 2 diabetes after prolonged use.
What can you do? Track your blood sugar if you’re on steroids, even if you feel fine. Eat fewer refined carbs. Stay active—walking after meals helps lower spikes. Talk to your doctor about alternatives if possible. Don’t quit steroids cold turkey—that’s dangerous. But do ask: Is this dose necessary? How long do I really need it? Are there other options?
Below, you’ll find real-world advice from people who’ve been there. You’ll see how metformin helps some, why certain painkillers can make it worse, and how to avoid double-dosing while managing multiple meds. There’s no magic fix, but there are clear steps you can take to protect your health while still getting the treatment you need.
Corticosteroid-Induced Hyperglycemia and Diabetes: How to Monitor and Manage It
Dec 1 2025 / MedicationsCorticosteroid-induced hyperglycemia affects up to 50% of patients on high-dose steroids. Learn how to monitor blood sugar, when to start insulin, and why tapering can cause dangerous lows.
VIEW MORE