Understanding Prednisolone and Its Uses
Prednisolone is a type of steroid medication that is commonly used to treat a wide range of inflammatory and autoimmune conditions, such as asthma, allergies, rheumatoid arthritis, and lupus. It works primarily by suppressing the immune system, which in turn reduces inflammation and other symptoms associated with these conditions. While prednisolone can be a crucial component in managing these disorders, it is essential to be aware of the potential dangers that may arise from its misuse.
Recognizing the Signs of Prednisolone Abuse
Abusing prednisolone can lead to various physical and mental symptoms that may be a cause for concern. Some of the common signs of prednisolone abuse include mood swings, irritability, aggression, insomnia, weight gain, and facial swelling. If you or someone you know is experiencing these symptoms while taking prednisolone, it is essential to address the issue with a healthcare professional promptly. Early intervention can help prevent further complications and ensure proper treatment for the underlying condition.
The Impact of Long-Term Prednisolone Abuse on the Body
Long-term prednisolone abuse can have severe consequences on the body, some of which may be irreversible. One of the most significant side effects of prolonged prednisolone use is the suppression of the body's natural cortisol production. Cortisol is a hormone produced by the adrenal glands that play a crucial role in regulating stress, metabolism, and immune function. Over time, the body may become dependent on prednisolone, leading to a condition known as adrenal insufficiency. This can result in fatigue, weakness, weight loss, and even life-threatening shock if not addressed promptly.
Another potential consequence of long-term prednisolone abuse is the increased risk of infections due to the suppression of the immune system. This can make it more difficult for the body to fight off bacteria, viruses, and other pathogens, leading to frequent or severe infections. Furthermore, prolonged prednisolone use can also cause a variety of metabolic issues, such as high blood sugar levels, elevated cholesterol, and increased blood pressure, which can contribute to the development of cardiovascular diseases and diabetes.
Psychological Effects of Prednisolone Abuse
In addition to the physical consequences, prednisolone abuse can also have a profound impact on one's mental health. The use of prednisolone has been associated with an increased risk of mood disorders, such as depression and anxiety. Moreover, some individuals may experience severe mood swings, aggression, and even psychotic symptoms, such as hallucinations and delusions, while abusing prednisolone. These psychological effects can significantly impact an individual's quality of life and relationships with others, making it essential to address any concerns related to prednisolone abuse as soon as possible.
Preventing and Addressing Prednisolone Abuse
The best way to prevent prednisolone abuse is to use the medication only as prescribed by a healthcare professional and closely monitor any side effects that may arise. If you suspect that you or someone you know may be abusing prednisolone, it is crucial to seek help from a healthcare provider or a mental health professional. They can assess the situation and recommend appropriate treatment options, which may include adjusting the prednisolone dosage, switching to an alternative medication, or addressing any underlying psychological issues that may be contributing to the abuse.
It is also essential to educate yourself and others about the potential dangers of prednisolone abuse and promote open communication with healthcare providers to ensure the safe and effective use of this medication. By being proactive and vigilant, we can minimize the risks associated with prednisolone abuse and ensure that those who need this medication can continue to benefit from its therapeutic effects.


India Digerida Para Occidente
May 6, 2023 AT 01:18Prednisolone is a powerful ally when used correctly, yet its shadow looms large when abused. The dramatic swings in mood and the swelling of the face feel like a storm raging inside. We must champion responsible prescribing while acknowledging the human stories behind each bottle. Let us unite in education, lest the very drug that heals become a hidden weapon.
Andrew Stevenson
May 6, 2023 AT 17:58Indeed, the pharmacodynamics of prednisolone can precipitate iatrogenic complications if the therapeutic window is exceeded. Optimizing dosage regimens and employing steroid-sparing agents can mitigate adverse drug reactions. It's encouraging to see clinicians embrace evidence‑based tapering protocols, thereby preserving adrenal integrity. Collaboration across specialties ensures we harness its benefits without courting iatrogenesis.
Kate Taylor
May 7, 2023 AT 10:38Your points are spot‑on, especially regarding tapering schedules. From a clinical perspective, integrating glucocorticoid‑receptor antagonists can further buffer the systemic impact. Patients often appreciate the jargon‑laden explanations when we break them down into lay terms. This collaborative approach bridges the knowledge gap and promotes adherence.
Hannah Mae
May 8, 2023 AT 03:18i dont think all docs are that scared of steroids. some ppl just take it for the quick fix and dont care. these warnings are overblown imo.
Iván Cañas
May 8, 2023 AT 19:58While I respect that viewpoint, cultural attitudes toward medication can vary widely. In many communities, the trust placed in a physician's guidance is paramount, and abrupt changes can cause anxiety. It's worth noting that education about risks often improves outcomes across diverse groups. Let's keep the dialogue open and inclusive.
Jen Basay
May 9, 2023 AT 12:38Interesting read! I'm reminded of how the endocrine system balances so many processes. 🤔 It's fascinating to see the cascade of effects when one hormone is tweaked.
Hannah M
May 10, 2023 AT 05:18Absolutely, the endocrine interplay is like a symphony 🎶. When prednisolone throws a note off‑key, the whole piece can wobble. Your curiosity helps shine a light on hidden risks.
Poorni Joth
May 10, 2023 AT 21:58People need to quit making excuses! Any dosage beyond the prescibed amount is a *sin* against your own health. The side‑effects are not just "some" issues-they're real, life‑threatening atractions! Stop ignoring the science and take responsibility.
Yareli Gonzalez
May 11, 2023 AT 14:38It's vital to keep this conversation grounded in compassion. Supporting those who might be struggling with dosage concerns can make a huge difference.
Alisa Hayes
May 12, 2023 AT 07:18Compassion is the backbone of effective healthcare. When patients feel heard, they're more likely to report side effects early, allowing clinicians to intervene before complications arise. In practice, regular check‑ins and transparent dialogue foster trust. Moreover, tailoring the tapering plan to individual lifestyle factors respects both medical necessity and personal autonomy. This balanced approach can prevent the cascade of adrenal insufficiency and metabolic disturbances.
Mariana L Figueroa
May 12, 2023 AT 23:58Staying active and monitoring labs are key; keep your doctor in the loop.
mausumi priyadarshini
May 13, 2023 AT 16:38Indeed, proactive engagement-regular bloodwork, vigilant symptom tracking, and consistent communication-serves as a multi‑layered safeguard; however, one must remember that individual variability, dosage adjustments, and comorbid conditions, all intertwine, demanding a nuanced, personalized approach.
Carl Mitchel
May 14, 2023 AT 09:18Let's be crystal clear: misuse of prednisolone is a textbook case of moral hazard. The cascade of biochemical disruptions is not a trivial footnote; it's a systemic failure that burdenizes both patient and healthcare system. Knowledgeable clinicians should preemptively address these pitfalls rather than react after damage is done. By championing strict adherence, we uphold both scientific integrity and ethical responsibility.
Suzette Muller
May 15, 2023 AT 01:58I appreciate the thorough analysis. From a practical standpoint, integrating patient education sessions can demystify the tapering process and reduce the temptation for overuse.
Josh SEBRING
May 15, 2023 AT 18:38Honestly, I think all this hype is for the pharma lobby. People can handle a bit of swelling or mood swing if it means their arthritis gets better. The risks are exaggerated, just read the label.
Lily Tung
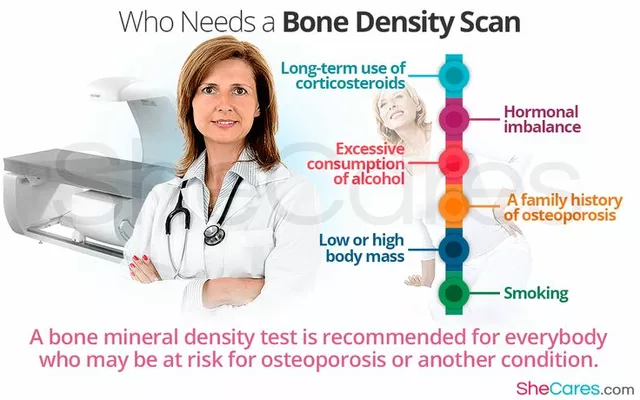
May 16, 2023 AT 11:18While I respect the sentiment that patients desire immediate relief, it is imperative to recognize the intricate cascade of physiological events precipitated by indiscriminate glucocorticoid exposure. Prolonged suppression of the hypothalamic‑pituitary‑adrenal axis compromises endogenous cortisol synthesis, thereby ushering in a state of adrenal insufficiency that may manifest as profound fatigue, orthostatic hypotension, and even circulatory collapse under stress. Concurrently, the immunosuppressive properties increase susceptibility to opportunistic infections, a risk that is often underappreciated until severe sepsis ensues. Metabolically, chronic corticosteroid use perturbs glucose homeostasis, precipitating steroid‑induced diabetes mellitus, while also promoting dyslipidemia and hypertension, all of which collectively elevate cardiovascular morbidity. Osteoblastic activity is inhibited, leading to accelerated bone demineralization, heightened fracture risk, and ultimately osteoporotic sequelae. Dermatologically, subcutaneous fat redistribution yields characteristic Cushingoid facies and truncal obesity, further impacting psychosocial wellbeing. Neuropsychiatrically, patients may experience mood lability, depressive episodes, or even steroid‑induced psychosis, complicating adherence and quality of life. From a pharmacokinetic perspective, the variable bioavailability of oral prednisolone necessitates careful dose titration, especially in patients with hepatic impairment, to avoid accumulation and toxicity. The concept of steroid‑sparing agents, such as methotrexate or biologics, offers a viable strategy to mitigate these adverse outcomes while preserving disease control. Education regarding gradual tapering protocols is paramount; abrupt cessation can precipitate adrenal crisis, an emergent condition marked by hypotension, electrolyte imbalance, and shock. Clinicians should employ regular monitoring of serum cortisol levels, fasting glucose, lipid panels, and bone density scans to preemptively identify complications. Patient empowerment through shared decision‑making fosters adherence to tapering schedules and reduces the allure of self‑medication. Moreover, interdisciplinary collaboration among rheumatologists, endocrinologists, and primary care physicians ensures a holistic approach to management. In summary, while prednisolone remains a cornerstone therapy for inflammatory conditions, its misuse carries a constellation of preventable, yet potentially irreversible, adverse effects that demand vigilant stewardship.
Taryn Bader
May 17, 2023 AT 03:58Whoa, that’s a massive hormonal rollercoaster!
Myra Aguirre
May 17, 2023 AT 20:38Sounds intense, but keeping an eye on the dosage is key.
Shawn Towner
May 18, 2023 AT 13:18Honestly, the alarmist tone overstates the danger; most patients tolerate short courses well. Still, a balanced view matters. Excess caution can deter necessary treatment.