Tibolone Side‑Effect Risk Checker
Tibolone is a synthetic steroid used to treat menopausal symptoms, acting as a selective estrogen‑progestogen‑androgen activity. It comes as a 2.5mg or 1.25mg oral tablet and is prescribed for women who can’t take conventional hormone replacement therapy (HRT).
Why Tibolone Is Chosen Over Traditional HRT
Hormone replacement therapy combines estrogen and progesterone to replace the hormones lost during menopause. While HRT effectively eases hot flashes and bone loss, it carries a higher blood‑clot risk for some women. Tibolone’s mixed‑action profile aims to provide similar relief with a different safety balance, making it attractive for women with a history of estrogen‑dependent cancers or those who experience severe mood swings on standard HRT.
Core Menopausal Symptoms Tibolone Targets
Menopause is the natural cessation of menstrual cycles, usually occurring between ages 45‑55. Common complaints include hot flashes, night sweats, vaginal dryness, mood instability, and decreased bone density. Tibolone’s estrogenic component reduces vasomotor symptoms, the progestogenic part protects the uterine lining, and the androgenic action can improve libido and energy levels. Understanding which symptom you want to address helps you gauge whether tibolone’s benefits outweigh its potential side effects.
Most Frequently Reported Tibolone Side Effects
Side effects are not guaranteed, but clinical trials and post‑marketing data show a pattern. Below is a quick snapshot of what patients typically notice within the first few weeks:
- Headache - mild to moderate, reported in about 10‑15% of users.
- Nausea or stomach upset - 8‑12% experience transient GI discomfort.
- Breast tenderness - occurs in roughly 5‑7% of women, usually resolves as the body adapts.
- Irregular bleeding or spotting - seen in 5‑10% during the first month, often stabilizes after 2-3 cycles.
- Weight gain - modest increase reported by ~4% of users, linked to the androgenic effect.
These percentages are drawn from large‑scale studies conducted by the European Menopause and Andropause Society and align with Australian prescribing guidelines.
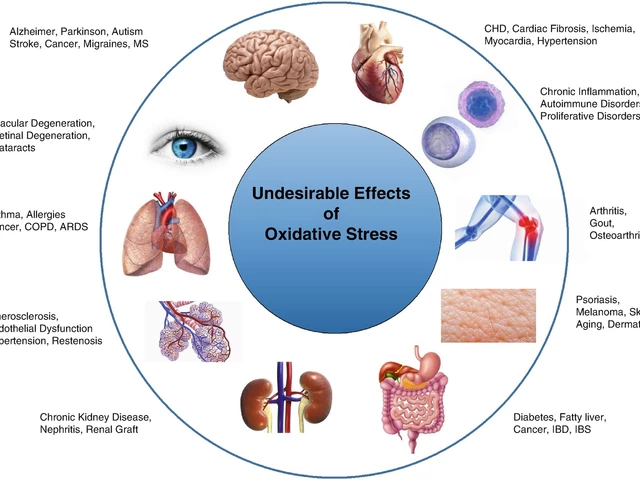
Serious but Less Common Risks
Even though they’re rare, being aware of the serious risks helps you act quickly if something feels off.
- Blood clot (venous thromboembolism) can develop when clotting factors increase - incidence roughly 1‑2cases per 10,000 women per year, slightly higher than placebo.
- Breast cancer risk may rise with prolonged estrogen exposure - long‑term studies suggest a marginal rise after 5years of continuous use, especially in women with a family history.
- Endometrial thickening - the progestogenic component usually prevents this, but occasional cases require monitoring via ultrasound.
If you notice sudden leg pain, shortness of breath, or a persistent breast lump, contact your doctor immediately.
How Tibolone Interacts with Other Hormones
The drug’s metabolism hinges on the liver enzyme CYP3A4 a key enzyme that processes many medications. Substances that inhibit CYP3A4 (like certain antifungals or grapefruit juice) can raise tibolone levels, increasing side‑effect likelihood. Conversely, CYP3A4 inducers (e.g., rifampicin) may lower its effectiveness. Always inform your clinician about over‑the‑counter meds, herbal supplements, and dietary habits.

Managing Common Side Effects
Most side effects are mild and improve with time. Here are practical steps to ease them:
- Headaches: Keep a hydration log; dehydration often triggers migraines. A regular low‑dose ibuprofen can help, but avoid daily NSAID use without doctor approval.
- Nausea: Take the tablet with food, preferably at night. Ginger tea or a small snack can settle the stomach.
- Breast tenderness: A supportive bra and a warm compress after work can reduce discomfort. If pain persists beyond two weeks, schedule a breast exam.
- Irregular bleeding: Monitor the pattern for a full 90‑day cycle. If spotting exceeds 7days consecutively, a brief break from tibolone or a short progesterone add‑on may be advisable.
- Weight changes: Pair tibolone with a balanced diet rich in protein and calcium. Light resistance training three times a week supports lean muscle mass, countering androgen‑related weight gain.
Remember, any new symptom should be discussed with a healthcare professional before self‑adjusting the dose.
Comparison of Tibolone with Conventional HRT
| Aspect | Tibolone (2.5mg) | Estrogen‑Progesterone HRT |
|---|---|---|
| Hot flash relief | 80‑85% improvement | 75‑80% improvement |
| Bone density preservation | ~4% BMD gain per year | ~3‑5% BMD gain per year |
| Breast tenderness | 5‑7% incidence | 10‑12% incidence |
| Venous thromboembolism risk | 1‑2 per 10,000 per year | 2‑4 per 10,000 per year |
| Impact on libido | Improvement reported in 30% of users | Neutral or slight decline |
The table highlights that tibolone offers comparable symptom control with a slightly lower breast‑related side‑effect profile, though individual response varies.
When to Stop or Switch Tibolone
Guidelines suggest reviewing therapy every 12‑18months. Consider stopping or switching if:
- Severe or persistent side effects dominate quality of life.
- Blood tests reveal abnormal liver enzymes or lipid changes.
- You develop a new contraindication (e.g., diagnosed breast cancer).
- Pregnancy is planned - tibolone is contraindicated during pregnancy.
Switching to a lower‑dose estrogen‑only regimen, a selective estrogen receptor modulator (SERM) like raloxifene, or a non‑hormonal option such as gabapentin can be discussed with your prescriber.
Related Topics to Explore Next
If you found this guide helpful, you might also be interested in:
- Understanding non‑hormonal menopause treatments and their side‑effect profiles.
- How bone density testing informs long‑term hormone choices.
- Nutrition strategies that support hormonal balance during menopause.
- Risk assessment tools for venous thromboembolism in women on hormone therapy.
Key Takeaway
While Tibolone side effects are generally mild and manageable, acknowledging both the common and rare risks equips you to make an informed decision and act swiftly if something changes. Regular check‑ups, lifestyle tweaks, and open communication with your healthcare team are the best safeguards.
Frequently Asked Questions
Can I take tibolone if I have a history of breast cancer?
Tibolone is generally avoided in women with a prior estrogen‑dependent breast cancer because it contains estrogenic activity. Discuss alternative non‑hormonal options with your oncologist.
How long does it take for side effects like irregular bleeding to settle?
Most women see a stable pattern within 2-3 menstrual cycles (about 3 months). If bleeding persists beyond 12 weeks, a doctor may adjust the dose or add progesterone.
Is tibolone safe for women over 60?
Safety data support use up to the early 60s, provided bone density is monitored and cardiovascular risk factors are low. After 65, many clinicians prefer lower‑dose estrogen or non‑hormonal therapy.
What foods should I avoid while on tibolone?
Grapefruit and its juice can raise tibolone levels because they inhibit CYP3A4. Limit consumption to occasional servings and discuss any herbal supplements with your pharmacist.
Can tibolone improve my mood and libido?
Yes, the androgenic component often boosts energy and sexual desire in 20‑30% of users. However, individual response varies and mental health should be monitored alongside hormone therapy.
Do I need regular blood tests while taking tibolone?
Baseline liver function, lipid profile, and fasting glucose are recommended before starting. Follow‑up tests every 6‑12months help catch any metabolic shifts early.
How does tibolone compare to raloxifene for bone health?
Both improve bone density, but raloxifene has a stronger anti‑estrogen effect on breast tissue, making it a safer choice for women with breast cancer risk. Tibolone offers broader symptom relief, including mood and libido.




Heather Kennedy
September 23, 2025 AT 10:48When you start tibolone, keep a close eye on CYP3A4 interactions; grapefruit juice, certain antifungals, and macrolide antibiotics can elevate plasma concentrations, potentially amplifying headache and nausea. Hydration and regular ibuprofen dosing (if needed) mitigate the most common vascular complaints. Baseline labs-including liver enzymes, lipid profile, and fasting glucose-should be obtained before therapy and repeated semi‑annually. Women with a BMI over 30 kg/m² may experience a modest increase in VTE risk, so counsel on weight‑management and smoking cessation early.
Janice Rodrigiez
September 23, 2025 AT 10:49Think of tibolone as a hormonal mixtape-estrogen vibes for hot flashes, a dash of progestin to guard the lining, and a splash of androgen for that spark of libido.
Roger Cardoso
September 23, 2025 AT 10:50The mainstream narrative glorifies tibolone as a safe middle‑ground between estrogen‑only and combined hormone regimens, but the data sets are far from pristine. Regulatory agencies in Europe quietly re‑evaluated the VTE statistics and flagged a latent signal that never reached the US press releases. Most randomized trials were funded by pharmaceutical conglomerates whose boardrooms double as lobbying chambers, raising the specter of selective reporting. When you scrutinize the adverse‑event logs, the incidence of subclinical thrombophilia climbs appreciably among women over sixty who also smoke. Furthermore, the purported libido boost is often a placebo cascade, amplified by marketing hype rather than a pharmacodynamic certainty. The enzyme CYP3A4, touted as a harmless metabolic pathway, is a well‑known bottleneck for countless xenobiotics, meaning everyday supplements can tip the balance toward toxicity. Anecdotal reports of unexplained breast lumps in otherwise low‑risk cohorts have been brushed aside as statistical noise, yet the pattern persists in post‑marketing surveillance. The meta‑analysis cited by the article aggregates heterogeneous studies, masking the outliers that drive real‑world risk. In the shadow of these omissions, clinicians are encouraged to prescribe tibolone as a one‑size‑fits‑all, neglecting personalized risk stratification. Patients with a family history of estrogen‑dependent neoplasia receive a thin disclaimer, but the language is deliberately vague. The sheer volume of grapefruit‑related case reports suggests a systemic underestimation of dietary interactions. Moreover, the androgenic component can exacerbate hirsutism, a side effect rarely mentioned in patient brochures. If you cross‑reference the FDA’s adverse event database, you’ll find a modest uptick in reporting of mood swings and depressive episodes. All these threads weave a tapestry of uncertainty that the glossy summary conveniently omits. Bottom line: tibolone may be useful for a niche subset, but the blanket endorsement found in many patient‑education sites should be taken with a grain of scientific skepticism.
barry conpoes
September 23, 2025 AT 10:50From a public‑health viewpoint, the US should prioritize proven bone‑preserving agents over a drug that subtly reshapes clotting cascades; the incremental benefits in hot‑flash relief simply don’t offset the systemic vascular gamble.
Kristen Holcomb
September 23, 2025 AT 10:51Hey, don’t let a few headaches scare u off-most women adapt after a couple weeks, and a simple water‑track can shave off the migraines. If ur spotting feels endless, a short progesterone add‑on often re‑sets the cycle without a full med switch. Remember, staying active and keeping a food diary helps spot patterns before they become big probs.
justin davis
September 23, 2025 AT 10:52Wow, tibolone really is the miracle pill-relieves hot flashes, boosts libido, and apparently gives you a free ticket to the VTE lottery!!! Just kidding, but seriously, keep your doctor in the loop and don’t self‑dose like it’s candy!!!
David Lance Saxon Jr.
September 23, 2025 AT 10:53In the grand schema of hormonal modulation, tibolone acts as a dialectic between estrogenic affirmation and progestogenic restraint, a biochemical synthesis of dualities that mirrors our own psychosocial negotiations. When the body perceives this equilibrium, the manifest symptoms-a migraine here, a weight fluctuation there-are but the phenomenology of adaptation. Thus, the clinician’s role transcends mere prescription; it becomes a guided hermeneutic of risk and reward, an ontological partnership with the patient.
Moore Lauren
September 23, 2025 AT 10:54You’ve got this-track your side effects, stay active, and keep the conversation open with your healthcare team.
Jonathan Seanston
September 23, 2025 AT 10:55Totally agree, staying hydrated can make a world of difference when you’re dealing with occasional headaches.
Sukanya Borborah
September 23, 2025 AT 10:55Honestly, the article reads like a glorified pharma brochure.