Every year, millions of Americans face a brutal choice: pay for their medicine or pay for rent. It’s not a hypothetical. It’s real life. In the United States, the same pill you can buy for $20 in Canada or €15 in Germany might cost you $200 - sometimes more. And it’s not because the drug is better. It’s the same factory. The same active ingredient. The same packaging. So why does the U.S. pay so much more?
The System Was Built to Let Drug Companies Set Any Price
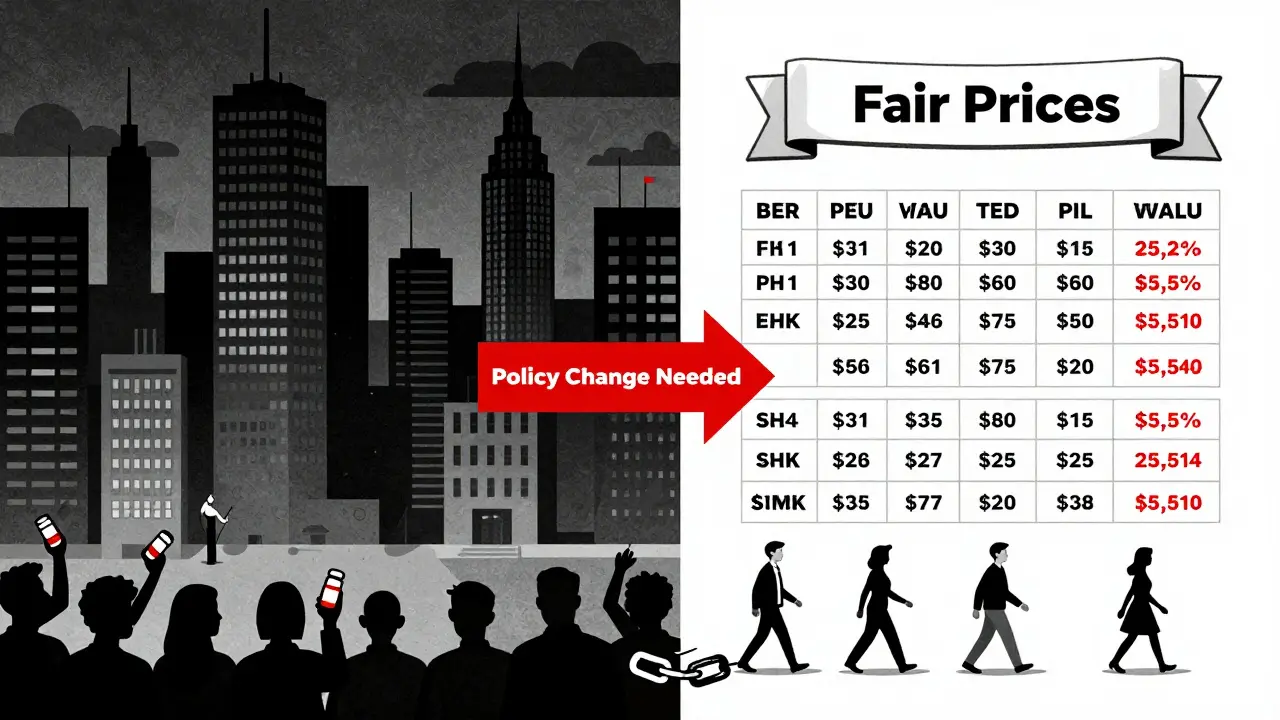
The U.S. is the only developed country where drugmakers can charge whatever they want. No government agency steps in to say, ‘That’s too high.’ In countries like the UK, Germany, or Japan, health authorities negotiate prices directly with manufacturers. If a company refuses to lower the price, the drug doesn’t get covered by public insurance. In the U.S., that power doesn’t exist - not for Medicare, not for Medicaid, not for private insurers. The Medicare Modernization Act of 2003 made it illegal for Medicare to negotiate drug prices. That law locked in a system where pharmaceutical companies have near-total control.
That’s not a coincidence. It was a deliberate decision. The pharmaceutical industry spent hundreds of millions lobbying Congress to block price negotiation. And it worked. For over 20 years, that rule stayed in place. Even today, Medicare can only negotiate prices for a tiny handful of drugs - just ten in 2026, rising to 15 in 2027. That’s less than 1% of all prescription drugs covered by Medicare. Meanwhile, other countries negotiate hundreds at once.
Who’s Really Getting Rich?
The U.S. makes up less than 5% of the world’s population. Yet, it accounts for 75% of global pharmaceutical profits. That’s not a typo. It means Americans are subsidizing drug research and development for the rest of the world - not because we’re generous, but because we’re forced to pay inflated prices.
Take Galzin, a drug used to treat Wilson’s disease. In the U.S., it costs $88,800 a year. In the UK, it’s $1,400. In Germany, $2,800. That’s a 1,555% markup. And Galzin isn’t even a new drug - it’s been around for decades. The cost to produce it hasn’t changed. But the price? It’s skyrocketed.
Companies claim they need high prices to fund innovation. But the data doesn’t back that up. The top 10 drugmakers spent $58 billion on R&D in 2024 - and $112 billion on marketing and profit distribution. That’s nearly double. And the most profitable drugs? Not the ones that cure cancer. The ones that manage chronic conditions - diabetes, obesity, high cholesterol. Drugs like Ozempic and Wegovy. In 2025, after public pressure, Novo Nordisk lowered the price of Ozempic from $1,000 to $350 a month. But that’s still five times what it costs in Europe. And they only did it after the White House threatened to use the Inflation Reduction Act to force a lower price.
The Middlemen Are Making It Worse
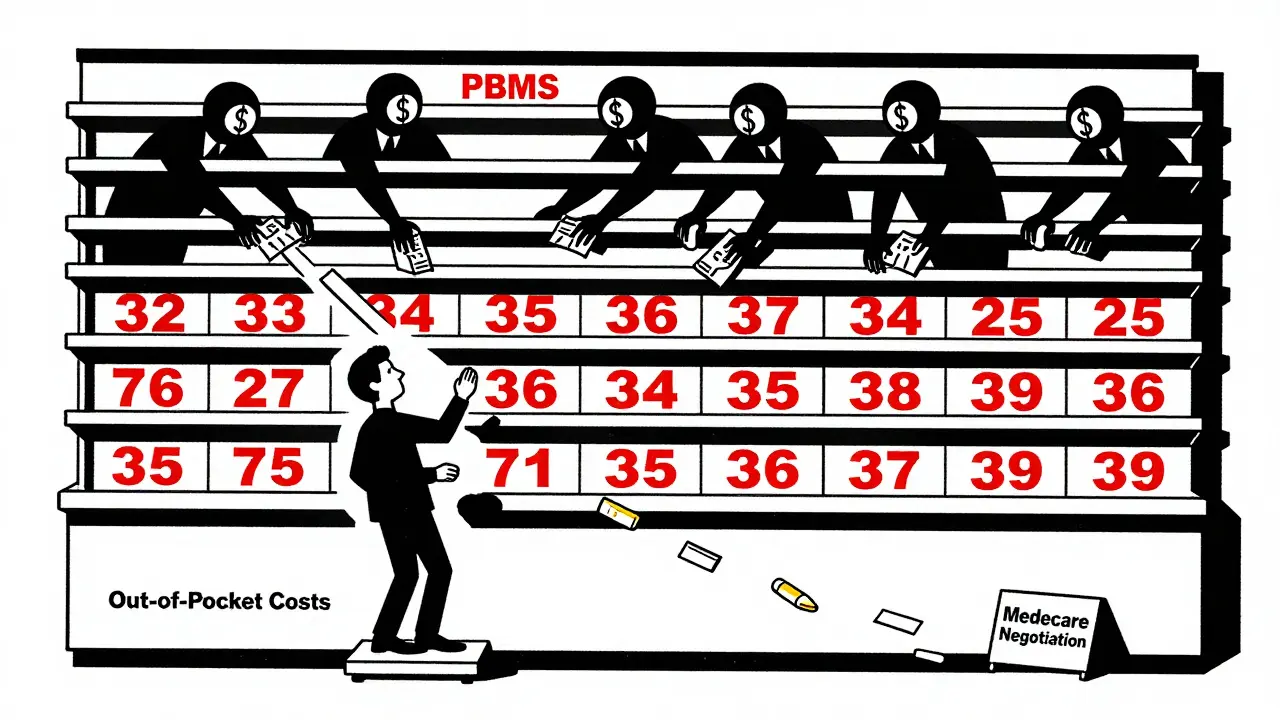
It’s not just drugmakers. There’s a whole hidden layer of middlemen making the system more expensive - Pharmacy Benefit Managers, or PBMs. Originally, PBMs were supposed to help insurers get discounts. Now, they’re owned by big insurance companies. And they’ve figured out a way to profit from high prices: rebates.
Here’s how it works: A drugmaker sets a high list price. The PBM negotiates a rebate - say, 40% off. The PBM keeps a chunk of that rebate. The rest goes to the insurer. But here’s the catch: the patient still pays based on the original high price. So if a drug’s list price is $1,000 and the rebate is $400, the patient might pay $200 out of pocket - even though the drug’s real cost is $600. The system rewards high prices, not low ones.
And because PBMs control which drugs get placed on insurance formularies, they can push manufacturers to raise prices just to pay bigger rebates. It’s a game where the only winners are the PBMs and the drugmakers. Patients and insurers lose.
The Inflation Reduction Act Tried to Fix It - But It’s Not Enough
In 2022, Congress passed the Inflation Reduction Act. For the first time, Medicare could negotiate prices on a small number of high-cost drugs. In 2025, the first 10 drugs were selected. By January 2025, HHS announced those drugs had already saved Medicare beneficiaries $1.5 billion in out-of-pocket costs. That’s real money. That’s life-changing for people on fixed incomes.
But here’s the problem: the law was weakened in 2025 by a budget reconciliation bill that cut funding for the negotiation program. Now, only 10 drugs are eligible in 2026. The program is too slow. Too narrow. And it doesn’t touch private insurance. So while Medicare patients get some relief, millions of others - the ones with private plans - still pay the full inflated price.
And it’s not just Medicare. The Inflation Reduction Act also introduced a $2,000 annual cap on out-of-pocket drug costs for Medicare Part D. That’s huge. Before, some seniors were paying $10,000 a year just for insulin and heart meds. Now, they won’t pay more than $2,000. But that cap doesn’t apply to people under 65. And it doesn’t stop drugmakers from raising prices year after year - they just pay a rebate to Medicare when they do. That rebate doesn’t go to the patient. It goes to the government.
Specialty Drugs Are the New Nightmare
The biggest driver of rising drug costs isn’t aspirin or antibiotics. It’s specialty drugs - the ones for cancer, rare diseases, diabetes, and obesity. These drugs cost $100,000 a year or more. And their prices keep climbing. IQVIA reports that in 2024, U.S. drug prices jumped 11.4% - the biggest increase in over a decade. The main reason? Novel obesity and diabetes medications.
These drugs are innovative. But they’re also monopolized. Patents block generics for years. And manufacturers extend patents in tiny ways - changing the delivery method, adding a new dosage - just to keep prices high. That’s called “evergreening.” It’s legal. And it’s everywhere.
Meanwhile, the cost of treating cancer has doubled in the last 15 years. A single course of immunotherapy can cost $250,000. Insurance may cover part of it. But the patient still pays thousands. And if they can’t afford it? They skip doses. Or stop treatment. That’s not a choice. That’s a death sentence.
What’s Next? The Fight Isn’t Over
There are two paths forward. One is reform. The other is chaos.
On the reform side, Senator Bernie Sanders’ Prescription Drug Price Relief Act proposes tying U.S. drug prices to what other wealthy countries pay. If Germany pays $500 for a drug, the U.S. pays $500. Simple. Direct. Fair. The White House has floated similar ideas, but so far, only a few deals have been made - and they’re voluntary.
On the chaos side, Project 2025 - a conservative policy blueprint - proposes gutting the Inflation Reduction Act. It would eliminate the $2,000 cap, remove Medicare negotiation entirely, and let PBMs keep their rebate system. According to the Center for American Progress, that plan would raise costs for 18.5 million Medicare beneficiaries. That’s nearly one in four seniors.
Meanwhile, drugmakers are fighting back. They’re suing to block Medicare negotiation. They’re lobbying Congress to block price transparency rules. And they’re spending millions on ads that say, ‘Don’t let the government take your medicine.’ But the truth is, the government isn’t taking anything. It’s just asking for a fair price.
What Can You Do?
If you’re paying high prices for your meds, you’re not powerless.
- Check if your drug is on Medicare’s negotiation list - if so, your price may drop in 2026.
- Use GoodRx or SingleCare to compare cash prices. Sometimes, paying cash is cheaper than insurance.
- Ask your doctor about generic alternatives. Many brand-name drugs have cheaper versions that work just as well.
- Call your insurer. Ask why your drug isn’t covered at a lower tier. Push back. You’d be surprised how often they’ll reconsider.
- Support policy changes. Write to your representative. Vote for candidates who prioritize drug pricing reform.
The system is broken. But it wasn’t built by accident. And it won’t be fixed by accident either. It takes pressure - from patients, from doctors, from voters. Because no one should have to choose between medicine and rent.
Why are drug prices so much higher in the U.S. than in other countries?
The U.S. is the only developed country that doesn’t allow the government to negotiate drug prices. In countries like Canada, Germany, and the UK, health agencies set fair prices based on what the drug is worth. In the U.S., drugmakers set their own prices with no limits. This system, created by laws like the Medicare Modernization Act of 2003, lets companies charge whatever they want - and they do.
Do Pharmacy Benefit Managers (PBMs) make drug prices higher?
Yes. PBMs were meant to lower costs by negotiating discounts, but now they’re owned by big insurers and profit from high list prices. They get rebates from drugmakers based on how high the price is - so they’re incentivized to push expensive drugs. Patients pay based on the high list price, not the discounted price, so PBMs benefit when prices go up, not down.
How does the Inflation Reduction Act help lower drug costs?
The Inflation Reduction Act lets Medicare negotiate prices for 10 high-cost drugs in 2026, with more added each year. It also caps out-of-pocket drug costs for Medicare Part D at $2,000 a year and requires drugmakers to pay rebates if they raise prices faster than inflation. These changes have already saved millions of seniors billions in out-of-pocket costs.
Why do drug companies keep raising prices even when they’re already profitable?
Because they can. With no price controls, companies treat drugs like luxury goods - the more people need them, the more they charge. Many drugs, especially for chronic conditions like diabetes or obesity, have no real competition. Patents block generics for years. Even after patents expire, manufacturers tweak the formula slightly to get new patents - a tactic called evergreening. Profit margins are huge, and there’s no legal penalty for raising prices.
Are generic drugs always cheaper?
Usually, yes - but not always. Sometimes, when only one generic manufacturer exists, they can raise prices too. And some brand-name drugs have no generic version because the patent is extended artificially. Always check prices on GoodRx or ask your pharmacist - sometimes the cash price for a generic is lower than your insurance copay.
What’s Project 2025, and how would it affect drug prices?
Project 2025 is a conservative policy plan that would eliminate Medicare’s ability to negotiate drug prices, scrap the $2,000 out-of-pocket cap, and weaken the Inflation Reduction Act. According to the Center for American Progress, this would raise costs for 18.5 million seniors and others on Medicare, forcing many to choose between medicine and basic needs.






Josh josh
January 24, 2026 AT 12:12eric fert
January 25, 2026 AT 10:15Karen Droege
January 25, 2026 AT 11:40Neil Thorogood
January 26, 2026 AT 06:56Jessica Knuteson
January 27, 2026 AT 11:02Angie Thompson
January 28, 2026 AT 06:25bella nash
January 29, 2026 AT 12:03Sally Dalton
January 30, 2026 AT 16:26Ashley Karanja
February 1, 2026 AT 01:01Geoff Miskinis
February 1, 2026 AT 22:09Mohammed Rizvi
February 3, 2026 AT 09:40Betty Bomber
February 5, 2026 AT 03:13Robin Van Emous
February 5, 2026 AT 09:00