Anticholinergic Burden Calculator
Medication Selection
Select your medications to calculate your total anticholinergic burden score (ACB)
Your Results
0
Low Risk
(ACB scores range from 1-3; 3 = highest burden)
Low Risk
0-1
Medium Risk
2
High Risk
3+
Important Note: This tool calculates your anticholinergic burden score based on the Anticholinergic Cognitive Burden Scale. A score of 3 or higher is associated with increased dementia risk according to recent research. Always discuss medication changes with your healthcare provider.
Every year, millions of older adults reach for over-the-counter antihistamines like Benadryl to help them sleep or manage allergies. It’s cheap, easy to find, and seems harmless-until you hear the quiet warnings from doctors and researchers. Could these common pills be quietly increasing the risk of dementia? The answer isn’t simple, but the evidence is growing harder to ignore.
Why Some Antihistamines Are More Dangerous Than Others
Not all antihistamines are the same. There are two main types: first-generation and second-generation. First-generation ones-like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine-cross the blood-brain barrier easily. Once inside, they block acetylcholine, a key brain chemical for memory and thinking. This is called anticholinergic activity. The stronger the block, the higher the potential risk. Second-generation antihistamines-like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-were designed differently. They’re built to stay out of the brain. Thanks to special transporters that push them back out, they barely touch acetylcholine receptors in the central nervous system. Their anticholinergic effect is about 100 to 1,000 times weaker than the first-gen versions. This difference isn’t theoretical. In a 2022 study of nearly 9,000 adults over 65, those taking first-generation antihistamines had dementia rates nearly four times higher than those using second-generation ones. But here’s the twist: when researchers adjusted for other health factors, the difference wasn’t statistically significant. That doesn’t mean it’s safe-it means the picture is messy.What the Big Studies Actually Show
The most cited research comes from Dr. Shelley Gray’s 2015 JAMA Internal Medicine study. It tracked over 3,400 older adults for a decade and found a clear link between long-term use of anticholinergic drugs and dementia. But here’s what most people miss: antihistamines didn’t show a significant risk increase on their own. The real culprits? Antidepressants, bladder medications, and drugs for Parkinson’s. Antihistamines were in the noise. A follow-up study in 2019 confirmed this. When researchers looked at over 1,000 daily doses of anticholinergic drugs, antihistamines showed a risk of exactly 1.00-meaning no increased risk. Meanwhile, bladder meds had a 65% higher risk. That’s a big gap. But then came a 2021 meta-analysis that grouped all anticholinergics together and found a 46% higher dementia risk. That number sounds scary, but it’s misleading. It lumps together powerful drugs like oxybutynin (for overactive bladder) with weak ones like Claritin. It’s like saying all cars are equally dangerous because a sports car and a bicycle are both called vehicles. The most recent data from the UK Biobank in late 2023 adds another layer. When researchers controlled for sleep disorders-the very reason many older adults take Benadryl-the link between antihistamines and dementia disappeared. That suggests the problem might not be the drug itself, but the underlying condition it’s treating: poor sleep, which is a known risk factor for cognitive decline.Why Doctors Still Say ‘Avoid’
Even with mixed study results, the American Geriatrics Society’s 2023 Beers Criteria still says: avoid first-generation antihistamines in people over 65. Why? Because the risk isn’t just about dementia. These drugs cause dizziness, confusion, dry mouth, urinary retention, and falls. One fall in an older adult can mean a broken hip, months in rehab, and a steep decline in independence. The Anticholinergic Cognitive Burden Scale (ACB) rates diphenhydramine as a level 3-the highest possible. That means even short-term use can add up. If someone takes it nightly for sleep, that’s 365 doses a year. Over five years, that’s nearly 2,000 doses. That’s not a few pills-it’s a heavy burden on the brain. Doctors aren’t just worried about dementia. They’re worried about the cumulative effect. Older adults often take multiple medications. Add a blood pressure pill, a painkiller, and a sleep aid-all with anticholinergic effects-and the total burden can tip the scale. One drug might be fine. Three together? That’s a different story.
What’s Really Going On in Real Life
In clinics and online forums, the disconnect is glaring. On Reddit’s r/geriatrics, a care manager reported that 83% of her clients over 70 were taking diphenhydramine every night-none of them knew it was an anticholinergic. On Drugs.com, 68% of the 2,347 comments about Benadryl mention long-term safety concerns. Yet the packaging still only says “may cause drowsiness.” A 2022 survey by the National Council on Aging found that 42% of adults over 65 use OTC antihistamines for sleep. And 78% of them had no idea these drugs carry any brain-related risk. That’s not ignorance-it’s a system failure. These pills are sold next to gum and candy. No prescription. No warning labels. No conversation with a doctor. One woman on AgingCare.com wrote: “My mother’s doctor prescribed Benadryl for years to help her sleep, and now she has dementia. I can’t help but wonder.” Her story isn’t rare. It’s common. And while science hasn’t proven causation, it hasn’t ruled it out either. The evidence is murky, but the human cost is real.What to Use Instead
The good news? There are safer alternatives. For allergies, switch to loratadine, cetirizine, or fexofenadine. They work just as well without the brain fog. For sleep, the gold standard isn’t a pill-it’s cognitive behavioral therapy for insomnia, or CBT-I. Studies show it’s 70-80% effective in older adults. It teaches you how to retrain your brain to sleep naturally. The problem? CBT-I is hard to access. Therapists are scarce. Wait times average over eight weeks. Medicare pays only $85 to $120 per session, so few providers take it. That’s why so many people stick with Benadryl-it’s the only option they can get right away. There are also prescription alternatives with low anticholinergic burden. Low-dose doxepin (Silenor), approved for insomnia in 2010, has an ACB score of just 1. It’s not perfect, but it’s far safer than diphenhydramine. And it’s gaining traction-now capturing 12% of the prescription sleep aid market.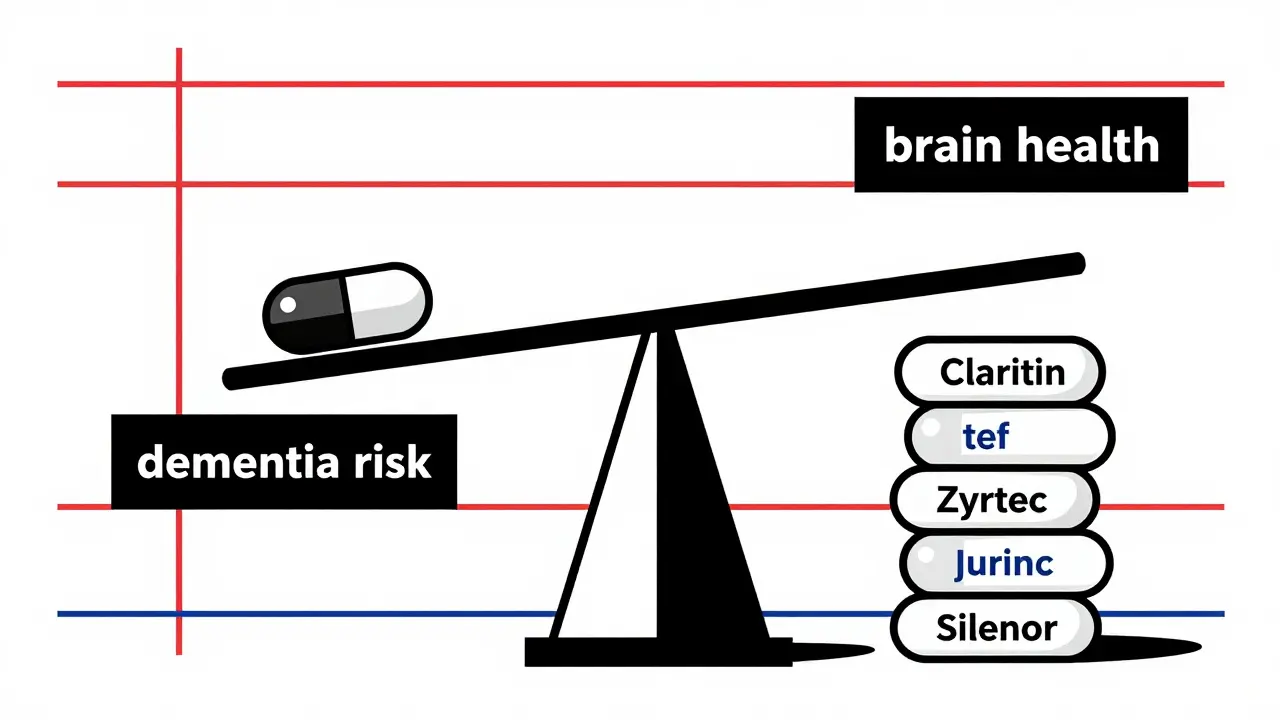
What You Can Do Today
If you or someone you care about is taking diphenhydramine, doxylamine, or chlorpheniramine regularly, here’s what to do:- Check the label. Look for “diphenhydramine,” “doxylamine,” or “chlorpheniramine.” If it’s in a sleep aid, allergy pill, or cold medicine, it’s probably there.
- Switch to a second-generation antihistamine. Choose Claritin, Zyrtec, or Allegra for allergies. They’re just as effective.
- For sleep, try non-drug options first. Cut caffeine after noon. Get sunlight in the morning. Keep your bedroom cool and dark. Try a 10-minute wind-down routine before bed.
- Ask your doctor about CBT-I. It’s not a magic fix, but it’s the most proven long-term solution for sleep problems.
- Review all meds every six months. Bring a list of everything you take-prescription, OTC, supplements-to your doctor. Ask: “Is this still necessary? Could it be harming my brain?”





Mandy Kowitz
January 4, 2026 AT 20:29So let me get this straight-we’re being told to avoid Benadryl like it’s poison, but my grandma’s been taking it since 1998 and still beats me at Scrabble? I’m not saying science is wrong, I’m just saying maybe the real issue is that we’re medicating normal aging into a crisis.
Chris Cantey
January 5, 2026 AT 20:19The brain is not a machine that accumulates wear like a car engine. To reduce cognitive decline to a pharmacological equation is to misunderstand the nature of consciousness. The anticholinergic burden is a metric invented by committees who’ve never held an elderly person’s hand as they forget their own name.
Abhishek Mondal
January 7, 2026 AT 15:01Let’s be precise: the 2022 study you cite had a confounding variable-sleep apnea prevalence-which was not adequately controlled. Moreover, the ACB scale is not validated for polypharmacy interactions in geriatric populations. The meta-analysis you dismiss as ‘misleading’ actually used a standardized effect size metric (Cohen’s d) with 95% CI-unlike the UK Biobank’s observational regression, which is vulnerable to immortal time bias. You’re cherry-picking the weakest studies to support a pre-existing narrative.
Oluwapelumi Yakubu
January 8, 2026 AT 22:34Man, I’ve seen this play out in Lagos-old folks popping Benadryl like candy because the clinic is 30km away and the nurse says ‘take one before bed, no problem.’ You think the FDA’s gonna fix this? Nah. It’s capitalism-profit over prevention. But here’s the real truth: if you can’t afford CBT-I, you don’t get to choose safety. You choose survival.
Terri Gladden
January 9, 2026 AT 16:52OMG I JUST REALIZED MY MOM’S SLEEP PILLS HAVE DIPHENHYDRAMINE IN THEM!! SHE’S BEEN TAKING THEM FOR 12 YEARS!! I’M CRYING RIGHT NOW I CAN’T BELIEVE NO ONE TOLD US THIS IS DANGEROUS!!
Jennifer Glass
January 11, 2026 AT 07:26It’s fascinating how the same science that warns us about anticholinergics also tells us that poor sleep increases dementia risk. So is the drug the problem-or the insomnia that drives people to it? Maybe the real failure is that we treat symptoms instead of root causes. Why isn’t CBT-I covered like insulin or statins?
Joseph Snow
January 11, 2026 AT 19:10Let’s be clear: this is a pharmaceutical industry smear campaign. First-gen antihistamines were cheap, effective, and widely used-until Big Pharma pushed expensive second-gen alternatives with patent protections. The ‘dementia risk’ narrative was quietly amplified to eliminate competition. The studies? Funded by drug manufacturers. The Beers Criteria? Written by consultants with ties to Pfizer. Don’t be fooled.
melissa cucic
January 12, 2026 AT 03:28Thank you for this nuanced, evidence-based breakdown. I especially appreciate the distinction between association and causation-and the acknowledgment that polypharmacy is the true culprit. As a geriatric nurse practitioner, I’ve seen patients taper off diphenhydramine and experience improved cognition within weeks. The problem isn’t the drug alone-it’s the lack of coordinated care.
Akshaya Gandra _ Student - EastCaryMS
January 14, 2026 AT 02:13so like… if i take zyrtec for allergies and benadryl for sleep… is that bad? i mean i only take benadryl like 2x a week? and my grandma died of dementia but she also smoked and never exercised so…
en Max
January 15, 2026 AT 01:21From a clinical pharmacology standpoint, the cumulative anticholinergic burden is quantifiable and clinically significant. Even low-dose, intermittent use contributes to cholinergic deficit over time, particularly in the elderly, where hepatic metabolism is reduced and blood-brain barrier permeability is increased. The absence of statistical significance in some studies does not equate to clinical insignificance. Risk mitigation requires proactive deprescribing.
Angie Rehe
January 16, 2026 AT 08:59Why are we still letting pharmaceutical companies sell brain-damaging drugs like they’re candy? This isn’t a ‘discussion’-it’s negligence. The FDA should have pulled these from shelves in 2010. And don’t even get me started on how pharmacies don’t even flag these interactions. I’ve seen people buy 10 bottles of NyQuil at once. Someone needs to be held accountable.
Jacob Milano
January 17, 2026 AT 05:49I used to take Benadryl every night for years-felt like a zombie by morning. Switched to Zyrtec and a 10-minute meditation before bed. Slept better, woke up clear-headed, and my wife says I stopped talking in my sleep. No magic. Just listening to your body. You don’t need a pill to sleep-you just need to stop fighting your rhythm.
Enrique González
January 17, 2026 AT 21:13Don’t panic. Don’t quit cold turkey. Talk to your doctor. Try one change at a time. Maybe start with cutting out night-time meds for a week and see how you feel. Small steps. Progress, not perfection.
Aaron Mercado
January 18, 2026 AT 18:06They told us smoking was safe. They told us asbestos was fine. They told us lead paint was okay. Now they’re telling us Benadryl is harmless? I’ve seen too many elderly people in nursing homes-zombie-like, drooling, confused-and guess what? Half of them were on diphenhydramine. This isn’t science-it’s a cover-up.
John Wilmerding
January 19, 2026 AT 12:16Thank you for this comprehensive overview. As a pharmacist with 18 years in geriatrics, I routinely screen for anticholinergic burden during medication reconciliation. I’ve seen patients reverse cognitive fog within 30 days of discontinuing first-gen antihistamines. The key is education and access. If we can’t provide CBT-I, we must at least offer safer alternatives-and we must stop treating OTC as ‘harmless.’