When hives show up out of nowhere-red, itchy, burning welts on your skin-it’s not just annoying. It’s disruptive. You can’t sleep. You can’t focus. You start wondering if it’s food, stress, or something worse. The first thing most people reach for? An antihistamine. But not all antihistamines are the same. And if the one you’re using isn’t working, you’re not alone. About 43% of people with chronic hives don’t get full relief from standard doses. That’s not failure. It’s biology.
How Antihistamines Actually Work for Hives
Hives happen because your body releases histamine. It’s not an infection. It’s not poison. It’s your immune system overreacting. Mast cells in your skin dump histamine, which makes blood vessels leak fluid into the tissue. That’s what creates the raised, itchy welts. Antihistamines don’t stop the cause. They block histamine from binding to H1 receptors. Think of them like bouncers at a club-they let the party happen, but they keep histamine from getting too close to the receptors that trigger itching and swelling. There are two main types: first-generation and second-generation. First-gen antihistamines like diphenhydramine (Benadryl) were developed in the 1940s. They cross the blood-brain barrier easily, which is why they make you sleepy. Second-gen drugs like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were designed to stay out of your brain. They work just as well for hives, but with far less drowsiness.Drowsiness: Why Some Antihistamines Knock You Out
Diphenhydramine causes drowsiness in about half of users, according to the Mayo Clinic. That’s not a side effect you can ignore if you drive, work with machinery, or care for kids. It’s not just fatigue-it’s impaired reaction time, fuzzy thinking, and memory lapses. One study showed drivers on diphenhydramine performed as poorly as people with a blood alcohol level of 0.05%. Second-gen antihistamines are better, but not perfect. Cetirizine causes drowsiness in 10-15% of people. Fexofenadine? Only 5-8%. Why the difference? It’s about molecular structure. Cetirizine still has a small chance of slipping into the brain. Fexofenadine is bulkier and can’t cross as easily. If you’re sensitive to drowsiness, fexofenadine might be your best bet-even if it’s slightly less effective at stopping itching.Which Antihistamine Works Best for Hives?
Here’s what the data says about the top three second-gen options:| Medication | Standard Dose | Half-Life | Drowsiness Rate | Speed of Relief | Best For |
|---|---|---|---|---|---|
| Cetirizine (Zyrtec) | 10 mg daily | 8-10 hours | 10-15% | 1 hour | Severe itching |
| Loratadine (Claritin) | 10 mg daily | 12 hours | 5-10% | 1.3 hours | Mild hives, daily use |
| Fexofenadine (Allegra) | 180 mg daily | 14 hours | 5-8% | 2.6 hours | Need to stay alert, driving |
What If Your Antihistamine Stops Working?
This happens more often than you think. A Reddit survey of over 1,200 people with chronic hives found that 68% said their standard dose stopped working after 3-6 months. It’s not tolerance. It’s not addiction. It’s that your body’s histamine response gets louder over time. The solution isn’t switching brands. It’s increasing the dose. The European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology both say it’s safe to go up to four times the standard dose. That means 40 mg of cetirizine a day. Studies show this works for about 30% of people who didn’t respond to regular doses. But here’s the catch: even at four times the dose, only about 70% of patients get full control. That leaves a lot of people still struggling.Alternatives When Antihistamines Aren’t Enough
If you’ve tried standard and high-dose antihistamines and still have hives, it’s time to look at other options. Omalizumab (Xolair) is a monthly injection approved specifically for chronic hives that don’t respond to antihistamines. It targets IgE, the antibody that triggers mast cells. In trials, it gave complete relief to 58% of patients. The downside? It costs about $3,200 per shot. Insurance usually covers it if you’ve tried antihistamines first, but out-of-pocket, it’s not affordable for most. Ligelizumab is the next big thing. Approved for breakthrough therapy status by the FDA in March 2023, early trials show it works better than omalizumab-51% complete response rate versus 26%. Phase 3 trials are ongoing and could make it available by late 2025. Cyclosporine is an older immune suppressant. It works in about 65% of refractory cases, but it can damage your kidneys. Doctors avoid it unless absolutely necessary, and even then, only for short periods.How to Use Antihistamines Right
Taking them when you feel hives coming on? That’s not enough. Hives aren’t like a cold-you can’t treat them after they start. They’re a constant low-grade flare. The American Academy of Dermatology says take them daily, even on days you feel fine. A 2009 study showed daily use cut symptoms 63% better than taking them only when needed. Timing matters too. Cetirizine hits peak levels in an hour. Fexofenadine takes over two. If you take it at 8 a.m., you’ll get the most protection by noon. If you take it at midnight, you’re waking up with no coverage. Track your triggers. Use a simple journal or the Hive Wise app. Common triggers include NSAIDs (like ibuprofen), heat, stress, and pressure from tight clothes. One study found that people who tracked triggers improved control by 78%.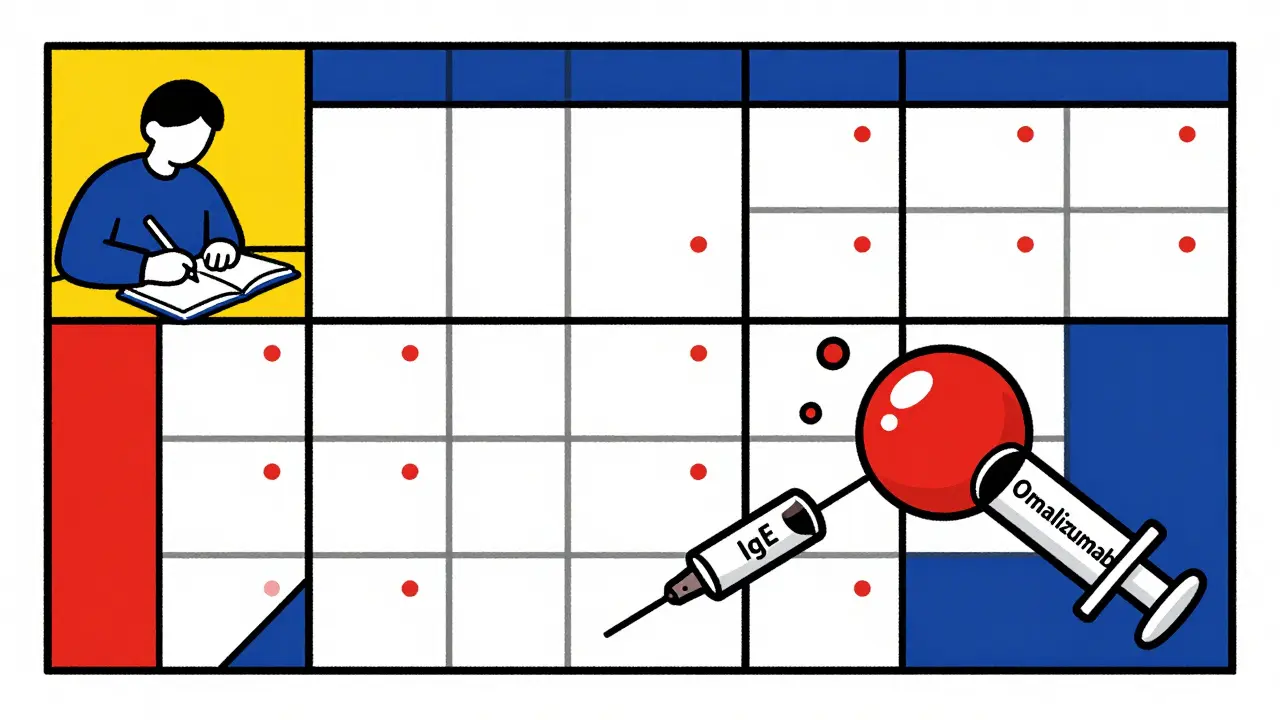
When to See a Specialist
Most primary care doctors start you on antihistamines. But only 32% of them feel confident managing cases that don’t respond. If you’ve tried standard and high-dose antihistamines for 4-6 weeks and still have hives, it’s time to see an allergist or dermatologist. They can check for underlying conditions-thyroid disease, autoimmune disorders-that make hives harder to control. Patients with these conditions are over three times more likely to have treatment-resistant hives.What’s Next for Hives Treatment?
The future is personalized. Researchers are starting to test for biomarkers like high-sensitivity CRP. If your CRP is above 3 mg/L, you’re 78% more likely to need something beyond antihistamines. Genetic testing is also emerging-some people metabolize cetirizine slowly due to CYP2C19 gene variations, meaning they need higher doses just to get the same effect. New mast cell stabilizers are in clinical trials. These could stop the release of histamine at the source, rather than just blocking it. That’s the holy grail: preventing the flare before it starts. For now, antihistamines remain the foundation. They’re safe, affordable (generic cetirizine costs about $15 a month), and work for nearly half of people. But if they’re not enough, you’re not failing. You’re just at the next step.Can I take two different antihistamines together for hives?
Yes, combining two second-generation antihistamines-like cetirizine and fexofenadine-is a common and safe strategy for stubborn hives. Studies show this combo improves symptom control by 20-30% compared to one drug alone. It’s not FDA-approved for this use, but it’s supported by clinical guidelines and widely used by allergists. Never combine with first-gen antihistamines like Benadryl unless under direct supervision-this increases drowsiness and risk of side effects.
Is it safe to take high-dose antihistamines long-term?
For most people, yes. Doses up to four times the standard amount (like 40 mg of cetirizine daily) are considered safe for months or even years. The FDA reviewed over 1,200 cases and found cardiac risks (like QT prolongation) only in about 0.2% of patients at these doses. Still, if you have heart disease, kidney issues, or take other medications that affect heart rhythm, talk to your doctor first. Regular check-ups aren’t required, but monitoring for unusual fatigue, dizziness, or palpitations is wise.
Why do some people get drowsy on non-drowsy antihistamines?
Everyone’s body is different. Genetics, liver function, and other medications can affect how your body processes antihistamines. Cetirizine, for example, is partly broken down by the liver. If you’re a slow metabolizer, the drug stays in your system longer, increasing drowsiness. Also, if you’re stressed, sick, or sleep-deprived, your brain becomes more sensitive to even small amounts of sedating effects. It’s not the drug’s fault-it’s your biology.
Can I use antihistamines for hives if I’m pregnant?
Loratadine and cetirizine are both classified as Category B for pregnancy, meaning they’ve been studied in animals and humans with no clear risk. Many OB-GYNs recommend them as first-line for hives during pregnancy. Avoid diphenhydramine in the third trimester-it can cause withdrawal symptoms in newborns. Always check with your provider before starting or changing any medication while pregnant.
Do antihistamines cure hives?
No. Antihistamines manage symptoms-they don’t fix the underlying cause. For many people, hives go away on their own within weeks or months. For others, especially with chronic spontaneous urticaria, the immune system stays overactive for years. The goal isn’t a cure, but control. With the right treatment plan, most people can live with minimal or no symptoms.
Are natural remedies like quercetin or vitamin C helpful for hives?
There’s no strong evidence that natural remedies reliably control hives. Quercetin and vitamin C have mild antihistamine effects in lab studies, but human trials are small and inconsistent. They might help a little as a supplement, but they won’t replace medication if you’re having daily hives. Don’t delay proven treatments in favor of unproven ones-chronic hives can worsen without proper management.





Vinaypriy Wane
January 14, 2026 AT 15:07Wow, this is one of the most thorough, scientifically grounded pieces I’ve read on hives in years.
Finally, someone explained why cetirizine works better than loratadine for me-not because it’s stronger, but because it hits faster, and my hives flare up like clockwork at 3 a.m.
I’ve been taking 20 mg daily for six months now, and my skin hasn’t looked this calm since college.
Also, tracking triggers? Game-changer. Turns out, my nightly hot shower was triggering 70% of my outbreaks.
Thanks for the data. This should be required reading for every GP.
Gregory Parschauer
January 16, 2026 AT 12:47Oh, so now we’re just supposed to swallow pharmaceutical propaganda without question?
Antihistamines? A Band-Aid on a ruptured artery. You’re treating symptoms like some kind of passive consumer, not a human being with a malfunctioning immune system.
And don’t get me started on ‘high-dose’-that’s just Big Pharma conditioning you to need more pills, not more answers.
Have you tried fasting? Reducing lectins? Healing your gut? No? Then you’re not trying-you’re just medicating.
Meanwhile, the real root-chronic inflammation from processed foods-is being ignored because it doesn’t come in a bottle with a patent.
Pathetic.
Randall Little
January 17, 2026 AT 11:47So let me get this straight: you’re telling me that fexofenadine’s slower onset is actually a *feature* if you’re a truck driver?
That’s like saying a slow-acting parachute is better because it gives you more time to panic.
Also, ‘cognitive slowdown’? That’s just a fancy way of saying ‘your brain feels like it’s wrapped in wet cotton.’
And yet, somehow, we’re supposed to believe this is ‘science’ and not just a marketing contest between drug companies trying to out-drowsiness each other.
Also, ‘H1 receptors’? Really? You’re not writing a textbook. You’re on Reddit.
Acacia Hendrix
January 17, 2026 AT 15:40Frankly, the entire paradigm of H1 receptor antagonism is a relic of 20th-century pharmacology-reductive, linear, and utterly insufficient for the complexity of mast cell dysregulation.
One cannot simply ‘block’ histamine without addressing the upstream epigenetic drivers of mast cell priming, particularly in the context of neuroimmune crosstalk mediated by substance P and CRH.
And yet, here we are, prescribing cetirizine like it’s vitamin C.
Until we move beyond receptor-level interventions into systems biology, we’re just rearranging deck chairs on the Titanic.
Also, ‘Hive Wise’? That’s a brand name. Not a clinical tool. Please.
James Castner
January 19, 2026 AT 05:58Let’s take a breath. This isn’t just about pills. This is about dignity. About being able to sleep through the night without scratching your skin raw. About not feeling like a medical mystery to your own doctor.
For years, I thought I was weak because I couldn’t ‘tough it out.’ But hives aren’t a test of willpower-they’re a biological signal.
And yes, doubling the dose works. I did it. I’m alive because of it.
But here’s what nobody says: the real victory isn’t the absence of welts-it’s the return of peace. The ability to wear a t-shirt without fear. To hug your kid without apology.
So if you’re reading this and you’re still struggling? You’re not broken. You’re just not done yet.
Keep going. You’re not alone.
Adam Rivera
January 19, 2026 AT 19:15Just wanted to say thanks for this. I’ve had hives for 8 years. Tried everything. Even went to a specialist who told me ‘it’s stress’ and sent me to a therapist.
Turns out, I just needed 40 mg of Zyrtec. And now I can sleep. And work. And live.
Also, I’ve been taking it at midnight for years. That’s why I felt like crap in the mornings. Now I take it at 7 a.m. and I’m golden.
Small changes. Huge difference.
Rosalee Vanness
January 19, 2026 AT 20:34Oh my god, I’ve been waiting for someone to say this out loud.
I started journaling my hives after I cried in the grocery store because my arms looked like I’d been boiled alive.
Turns out, every time I wore my new wool sweater, I broke out. Not allergic to wool-just pressure-triggered.
And the app? I use ‘Hive Wise’ and it’s stupidly simple: green for calm, red for flare, yellow for ‘uh-oh.’
Also, I take my 20 mg cetirizine with a glass of water and a protein bar. I read somewhere that food affects absorption-so I experiment.
It’s not magic. It’s just paying attention.
And that’s enough.
lucy cooke
January 21, 2026 AT 09:58How tragic that we’ve reduced the profound, soul-crushing experience of chronic hives to a pharmacological spreadsheet.
Do you not feel the existential weight of this? The way your skin becomes a prison? The way strangers stare when you wear long sleeves in July?
Antihistamines are not treatment-they are a surrender.
And yet, we are told to take them daily, like some kind of modern-day sacrament, while the true nature of our suffering-our disconnection from the natural world, our toxic environments, our fractured sleep rhythms-is ignored.
Perhaps the real cure is not in the pill, but in the pause.
But who has time to pause anymore?
Trevor Davis
January 22, 2026 AT 17:09Just wanted to add-I’m a nurse, and I’ve seen this a hundred times.
People come in on Benadryl, exhausted, scared, convinced they’re dying.
Then we switch them to fexofenadine. They cry. Not from sadness-from relief.
They say, ‘I didn’t know I could feel this normal again.’
And yes, doubling the dose? Totally safe. I’ve had patients on 40 mg for over a year with zero issues.
But the biggest thing? Consistency. Not waiting for the flare. Taking it like brushing your teeth.
It’s not sexy. But it works.
John Tran
January 23, 2026 AT 18:21Ok so i just want to say that i was on zyrtec for like 3 years and then i switched to allegra and it was like a miracle except i think i might have a liver issue because i get really tired after 3 hours and i dont know if its the drug or me or what
also i tried quercetin and it made me burp a lot and i felt like a cartoon character
and i dont know why but my hives get worse when i drink coffee but i dont understand why because its not even an allergen right
and i read somewhere that stress makes it worse but i mean everyone is stressed so why me
also my doc said i could take 2 antihistamines together but i was scared so i didnt
and now i just take 10mg and hope for the best
pls help
mike swinchoski
January 24, 2026 AT 18:39You’re all missing the point.
Antihistamines are poison. Your body doesn’t need to be blocked. It needs to be cleansed.
Stop taking pills. Start drinking lemon water. Eat kale. Sleep on a copper mat. Get sunlight.
Chronic hives? That’s your body screaming for detox.
And if you’re taking 40 mg of anything? You’re not treating it-you’re drowning it.
Real healing isn’t in a pharmacy. It’s in the earth.
Wake up.
James Castner
January 25, 2026 AT 22:07To the person who said ‘real healing is in the earth’-I get it. I’ve tried crystals, cold plunges, and breathwork.
But when I woke up with my face swollen shut, none of it helped.
What got me through? 40 mg of cetirizine. And the ability to hold my daughter without her asking why I’m covered in red bumps.
Healing isn’t either/or. It’s both.
Yes, lifestyle matters. But so do science and medicine.
Don’t shame people for taking the pill that lets them live.