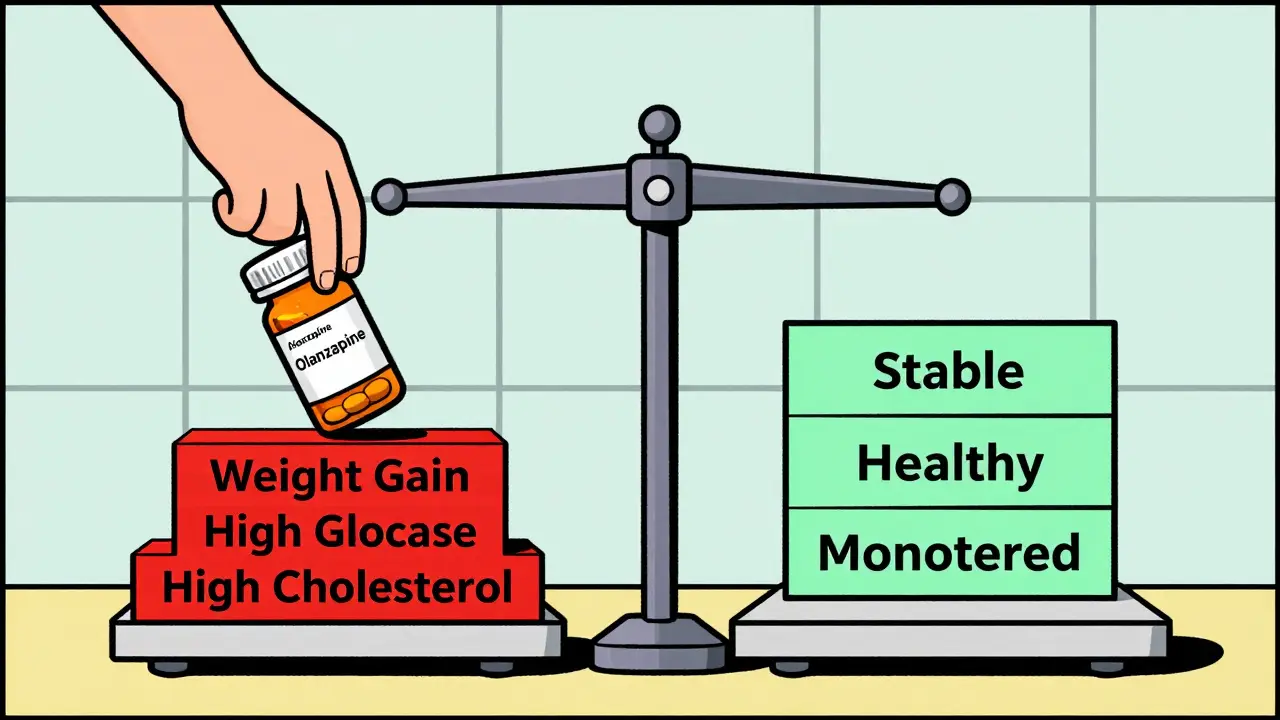
When you’re prescribed an antipsychotic, the goal is clear: reduce hallucinations, calm paranoia, and bring stability back to your life. But for many, the trade-off isn’t just about feeling better mentally-it’s about surviving physically. The most commonly prescribed second-generation antipsychotics, like olanzapine and clozapine, can trigger serious metabolic changes that increase your risk of diabetes, heart disease, and early death. And yet, too many patients aren’t even checked for these dangers.
Why Metabolic Side Effects Are a Silent Crisis
Antipsychotics don’t just affect your brain. They mess with your body’s ability to process sugar, fat, and energy. The result? Rapid weight gain, high blood sugar, abnormal cholesterol, and high blood pressure-all signs of metabolic syndrome. This isn’t a rare side effect. Around 32% to 68% of people taking these medications develop metabolic syndrome, compared to just 3% to 26% of those not on them. That’s a huge jump.And it’s not just about looks. Losing 20 to 25 years of life expectancy isn’t an exaggeration-it’s a documented reality for people with serious mental illness. About 60% of that gap comes from heart disease and diabetes, often worsened by the very drugs meant to help.
Some medications are far worse than others. Olanzapine and clozapine are the biggest offenders. In the first 18 months, patients on olanzapine gain an average of 2 pounds per month. About 30% gain over 7% of their body weight. That’s not a small fluctuation-it’s life-altering. Meanwhile, aripiprazole and ziprasidone cause minimal weight gain, often less than 5% of patients.
The Hidden Mechanisms Behind the Weight Gain
It’s not just that these drugs make you hungry. They actually rewire how your body handles energy. Antipsychotics block certain brain receptors-especially histamine H1 and serotonin 5-HT2C-that control appetite and insulin sensitivity. This means you might feel constantly hungry, even if you’re eating normally. Your body also becomes less responsive to insulin, so glucose builds up in your blood instead of fueling your cells.And here’s the twist: you don’t need to gain weight for your blood sugar to spike. Studies show people on olanzapine and clozapine develop insulin resistance even before they gain a pound. That’s why just tracking weight isn’t enough. You need to check blood sugar and lipids too.
Comparing Antipsychotics: Who’s at Highest Risk?
Not all antipsychotics are created equal when it comes to metabolic harm. Here’s how they stack up, from highest to lowest risk:- High risk: Clozapine, olanzapine
- Moderate risk: Quetiapine, risperidone, paliperidone
- Low risk: Aripiprazole, ziprasidone, lurasidone
That’s not just theory. The CATIE study, one of the largest real-world trials, found olanzapine caused more weight gain and worse cholesterol and glucose levels than any other drug tested. Meanwhile, aripiprazole and ziprasidone had the cleanest metabolic profiles. Even better, lumateperone (Caplyta), approved by the FDA in 2023, showed only 3.5% of patients gained weight-compared to 23.7% on olanzapine.
So why do doctors still prescribe high-risk drugs? Because for treatment-resistant schizophrenia, clozapine can cut mortality by half. It’s the last line of defense. But for many others, a lower-risk option could do the job just as well-with far fewer physical consequences.
What You Need to Monitor (And When)
The American Psychiatric Association and the American Diabetes Association agree: everyone starting an antipsychotic needs a baseline metabolic check-and regular follow-ups. Here’s what you should track:- Weight and waist circumference: Measure at baseline, then every 4 weeks for the first 3 months, then every 3 months.
- Blood pressure: Check at every visit. High blood pressure often flies under the radar.
- Fasting blood glucose: Test before starting, then at 12 weeks, 6 months, and annually.
- Lipid panel: Check cholesterol and triglycerides at baseline and every 6 to 12 months.
Don’t wait for symptoms. By the time you feel tired, thirsty, or out of breath, damage may already be done. Many patients don’t know their blood sugar is rising until they’re diagnosed with prediabetes or type 2 diabetes.
Real Stories: When Monitoring Failed
On Reddit, a user named AnxiousMedUser wrote: “I gained 45 pounds in six months on olanzapine. My doctor never checked my blood sugar. I had to switch to aripiprazole-even though it didn’t control my psychosis as well-because I couldn’t face another year of this.”A UK mental health charity collected similar stories. One patient stopped taking their medication after gaining 30kg in a year and developing prediabetes. “My psychiatrist never asked about my weight or diet,” they said. “I felt like I was being poisoned.”
But it’s not all bad news. Some people accept the trade-off. In a 2022 survey, 82% of clozapine users said their weight gain was “worth it” because their psychosis was finally under control. That’s a deeply personal decision-and one that should be made with full information, not silence.
What Works: Turning Risk Into Control
The good news? You can fight back. Studies show that when metabolic monitoring is built into psychiatric care, weight gain drops by up to 50%. How?- Switching meds: If you’ve gained more than 5% of your body weight, talk about switching to a lower-risk antipsychotic. Even a small change-like from olanzapine to aripiprazole-can make a big difference.
- Lifestyle support: A nutritionist, regular exercise, and sleep hygiene aren’t “nice-to-haves.” They’re part of treatment. Programs that combine psychiatric care with diet and fitness coaching have the best outcomes.
- Medication to help: Metformin, a diabetes drug, has been shown to reduce weight gain and improve insulin sensitivity in people on antipsychotics. It’s not a magic fix, but it’s a proven tool.
Too often, patients are told to “eat less and exercise more” with no support. That’s not care-it’s neglect. Real help means connecting you with resources, not just giving advice.

Why This Keeps Happening
Despite clear guidelines, only 38% of U.S. psychiatrists consistently follow metabolic monitoring protocols. Why? Three big reasons:- Fragmented care: Your psychiatrist doesn’t talk to your GP. Your blood test results sit in a different system.
- Time pressure: A 15-minute appointment isn’t enough to review weight, labs, mood, and side effects.
- Patient fear: Many avoid blood tests because they’re scared of what they’ll find-or feel guilty about their weight gain.
Systems that fix this-like Kaiser Permanente’s integrated model-have cut metabolic complications by 25%. They assign care coordinators, use automated alerts in electronic records, and schedule regular metabolic checkups alongside psychiatric visits.
What’s Next: Better Drugs, Better Systems
The future is starting to change. Lumateperone (Caplyta) is the first new antipsychotic in over a decade with a truly favorable metabolic profile. The National Institute of Mental Health is now funding research to predict who’s genetically at highest risk for weight gain and diabetes before they even start a drug. Imagine knowing your risk before the first pill-so you can choose a safer option from day one.But without systemic change, progress will be slow. Right now, patients are left to navigate this alone. The burden shouldn’t be on them. It’s on the system to protect their physical health as much as their mental health.
What You Can Do Today
If you’re on an antipsychotic, here’s your action plan:- Ask for your baseline labs: Make sure weight, waist, blood pressure, glucose, and lipids were checked before you started.
- Request a copy of your results: Don’t assume your doctor is tracking it. Keep your own record.
- Speak up about weight gain: If you’ve gained more than 5% of your body weight, say so. It’s a red flag.
- Ask about alternatives: Is there a lower-risk medication that could work for you?
- Request a referral: Ask for a dietitian or exercise program through your clinic. You’re not asking for extra care-you’re asking for standard care.
This isn’t about being perfect. It’s about being informed. You deserve to feel stable mentally-and physically alive.
Do all antipsychotics cause weight gain?
No. While many second-generation antipsychotics cause weight gain, the risk varies widely. Olanzapine and clozapine are the worst offenders, with up to 30% of users gaining significant weight. Aripiprazole, ziprasidone, and lurasidone have much lower rates-often under 5%. First-generation antipsychotics like haloperidol carry less metabolic risk but more movement-related side effects.
Can antipsychotics cause diabetes even if I’m not overweight?
Yes. Studies show that olanzapine and clozapine can impair insulin sensitivity and raise blood sugar levels even before weight gain occurs. This means someone with a normal BMI can still develop prediabetes or type 2 diabetes on these medications. That’s why checking blood glucose isn’t optional-it’s essential, no matter your weight.
How often should I get blood tests while on antipsychotics?
Baseline tests (weight, waist, blood pressure, fasting glucose, lipids) should be done before starting the medication. Then repeat at 4, 8, and 12 weeks after starting. After the first year, check at least once a year. If you’re on a high-risk drug like olanzapine or have other risk factors (family history of diabetes, obesity), your doctor should check every 3 to 6 months.
Is it safe to stop my antipsychotic if I’m gaining weight?
Never stop abruptly. Stopping suddenly can trigger psychosis relapse, which can be dangerous. If you’re concerned about weight gain or metabolic changes, talk to your doctor about switching to a lower-risk medication. Many people successfully transition to aripiprazole, lurasidone, or ziprasidone with good symptom control and fewer side effects.
Can lifestyle changes help reduce antipsychotic-related weight gain?
Yes. Research shows that combining healthy eating, regular physical activity, and behavioral support can cut weight gain by up to 50%. Programs that include dietitians, exercise coaches, and counseling integrated into psychiatric care work best. Even small changes-like walking 30 minutes a day or swapping sugary drinks for water-make a measurable difference.
Are there medications that can help counteract antipsychotic weight gain?
Metformin is the most studied and recommended option. It’s a diabetes drug that helps improve insulin sensitivity and can reduce weight gain by 2-5 kg over 6 months in people taking antipsychotics. Other options like topiramate or GLP-1 agonists are being studied but aren’t yet standard. Always discuss this with your doctor-don’t self-prescribe.




Rawlson King
December 15, 2025 AT 07:04Himmat Singh
December 16, 2025 AT 05:58kevin moranga
December 16, 2025 AT 07:13Webster Bull
December 16, 2025 AT 09:39Bruno Janssen
December 17, 2025 AT 20:53Scott Butler
December 18, 2025 AT 20:20Emma Sbarge
December 19, 2025 AT 19:30Shelby Ume
December 19, 2025 AT 21:33Jade Hovet
December 21, 2025 AT 06:47nithin Kuntumadugu
December 21, 2025 AT 11:31John Fred
December 21, 2025 AT 15:03Harriet Wollaston
December 22, 2025 AT 20:18kevin moranga
December 24, 2025 AT 10:44