Medication-Fiber Timing Calculator
How to Use This Tool
Enter your medication name to see the recommended timing window for taking fiber supplements. This tool is based on medical guidelines from the Mayo Clinic, FDA, and American Pharmacists Association.
Many people take fiber supplements to feel better, manage cholesterol, or keep things moving regularly. But if you’re also on medications, taking fiber at the wrong time can make your pills less effective-or even dangerous. It’s not just a myth. Fiber supplements can physically block or bind to drugs in your gut, cutting their absorption by up to half. And if you don’t know when to take them, you might be doing more harm than good.
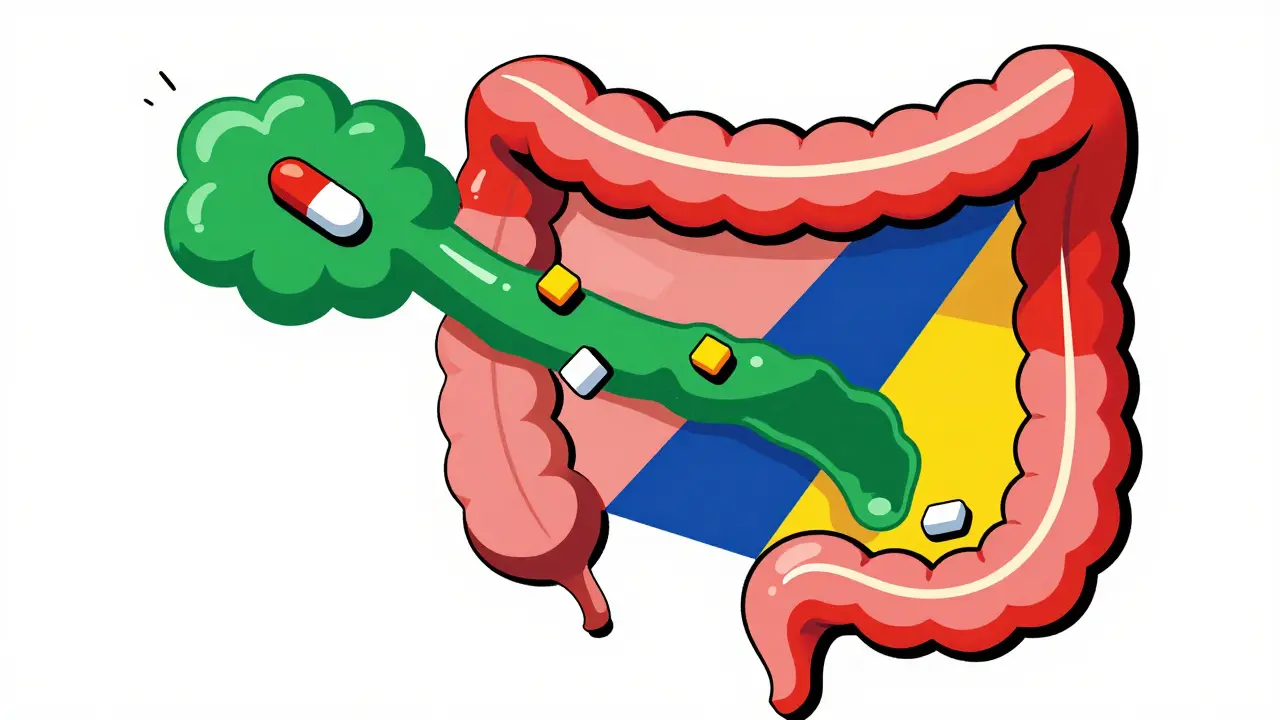
How Fiber Interferes with Medications
Fiber supplements like psyllium (Metamucil), methylcellulose, and inulin work by absorbing water and forming a thick gel in your digestive tract. That’s great for easing constipation and stabilizing blood sugar. But that same gel can trap medications as they try to pass through your small intestine, where most drugs get absorbed. The result? Less medicine enters your bloodstream, and your treatment doesn’t work as it should.
Studies show this isn’t theoretical. One 2020 study found that when people took levothyroxine (a thyroid hormone) at the same time as psyllium, their body absorbed 28.7% less of the drug. That’s enough to throw thyroid levels out of balance, causing fatigue, weight gain, or worse. Another study in the Journal of Clinical Lipidology showed psyllium could reduce absorption of certain medications by 30-50%. This isn’t rare. It happens with common prescriptions you might not even think about.
Medications That Definitely Don’t Mix with Fiber
Not all drugs are affected equally. Some are much more vulnerable to fiber’s gel-forming power. Here are the big ones:
- Levothyroxine - Used for hypothyroidism. Fiber can drop absorption by nearly 30%.
- Warfarin - A blood thinner. Fiber can interfere with how your body processes it, changing your INR levels and raising your risk of clots or bleeding.
- Metformin - A diabetes drug. Fiber may delay or reduce its effect, making blood sugar harder to control.
- Tetracycline and other antibiotics - Fiber binds to these drugs like a magnet, stopping them from working.
- Blood pressure meds - Especially beta-blockers and ACE inhibitors. Patients have reported their pressure spiking after starting fiber without adjusting timing.
And it’s not just prescription drugs. Some over-the-counter pills, like certain pain relievers or antacids, can also be affected. If you’re unsure, check the drug’s label or ask your pharmacist. Most will list fiber as a potential interaction.
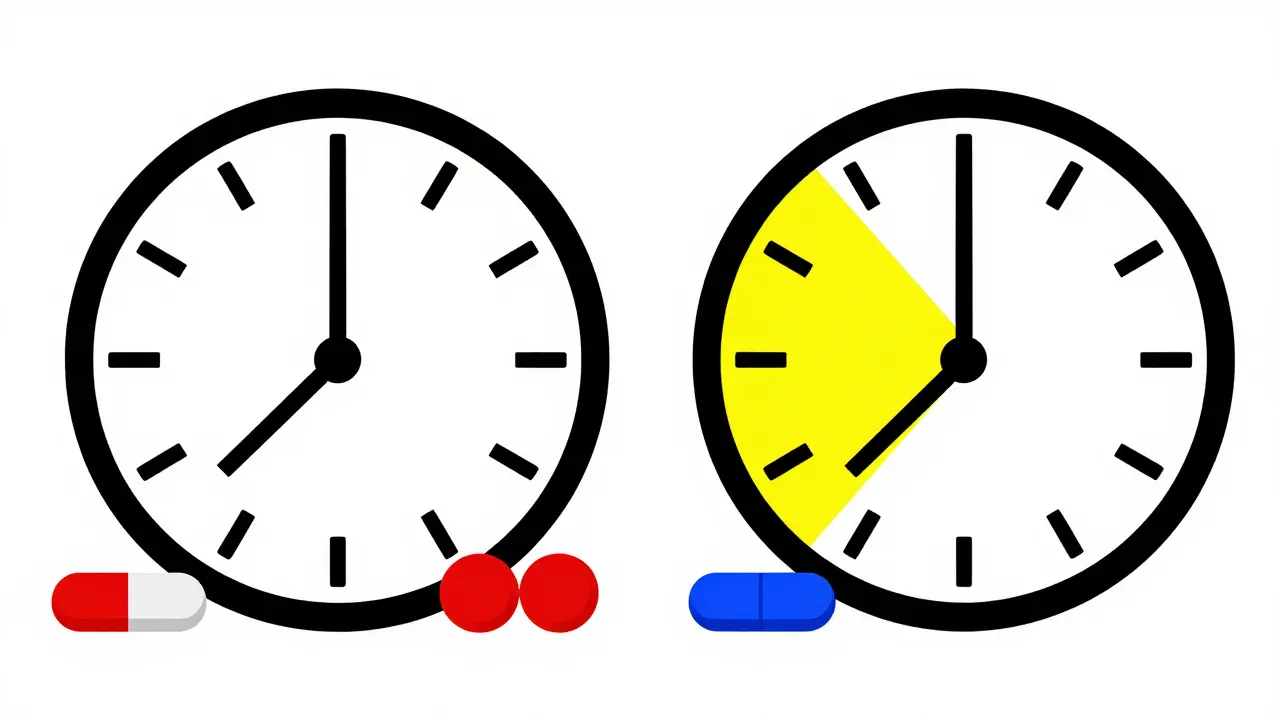
The Right Timing: 1 Hour Before or 2-4 Hours After
The fix isn’t quitting fiber. It’s timing it right. Every major health organization-Mayo Clinic, Cleveland Clinic, FDA, American Pharmacists Association-agrees: separate fiber from medications by at least one hour before or two to four hours after.
Why that range? Because the gel takes time to form and then slowly breaks down. Taking fiber just 30 minutes before your pill might still be too close. Waiting four hours gives your body enough time to absorb the drug before the fiber gel starts clogging the pipes.
Here’s how to make it work in real life:
- If you take your meds in the morning on an empty stomach (like levothyroxine), take fiber at lunch or dinner.
- If you take meds at night, take fiber in the morning-ideally 20-30 minutes before breakfast to help with appetite control.
- Never take fiber right before bed. Research shows 68% of people who do experience bloating, gas, or cramps that ruin their sleep.
One Reddit user shared a story that’s common: their thyroid levels stayed high even after increasing their levothyroxine dose. Turns out, they were taking Metamucil with their morning coffee. Once they moved fiber to midday, their TSH normalized in six weeks.
Special Cases: Bariatric Surgery, IBS, and Statins
Not everyone follows the same rules. Some people need extra caution.
After bariatric surgery: Your stomach is smaller, and digestion moves faster. Taking fiber too close to meds can cause blockages or poor absorption. Experts recommend waiting at least one hour before or two to four hours after meds-start with just 1-2 grams of fiber and increase slowly.
With IBS: About 42% of people with irritable bowel syndrome find that taking fiber on an empty stomach makes bloating and cramps worse. If that’s you, take fiber with a meal instead of before it. Stick to soluble fibers like oats or psyllium-they’re gentler than insoluble types like wheat bran.
With statins: Here’s the exception that proves the rule. A 2015 study found that taking psyllium with a low dose of simvastatin actually improved cholesterol-lowering results. The fiber didn’t block absorption-it helped the drug work better. But this only works when both are taken together before meals. Don’t assume this applies to all meds. Only do this under your doctor’s supervision.
How to Stay Consistent (Without Forgetting)
Knowing the rule is one thing. Following it every day is another. Life gets busy. Pills get mixed up. That’s why simple systems matter.
Start by writing out your daily schedule:
- List all your medications and when you take them.
- List all your supplements, including fiber.
- Mark the 2-4 hour windows around each pill where fiber is safe.
- Choose the simplest window-maybe lunch or bedtime (but not right before sleep).
Use phone alarms. Set one for your pill time, and another for your fiber time. Apps like Medisafe or MyTherapy can send reminders and track interactions. One user on Amazon said: “I used to forget and take them together. Now I have a 3 p.m. reminder for fiber. My blood pressure meds work again.”
Hydration is just as important. Fiber needs water to work safely. Always drink at least 8 ounces with each dose. Aim for 64-80 ounces total daily. Without enough water, fiber can cause constipation or even intestinal blockages.

What to Do If You’ve Been Taking Them Together
If you’ve been taking fiber and meds at the same time for weeks or months, don’t panic-but don’t ignore it either.
Look for signs your meds aren’t working:
- Thyroid symptoms returning (fatigue, weight gain, cold intolerance)
- Blood sugar spikes despite taking metformin
- Unexplained bruising or bleeding (warfarin issue)
- High blood pressure despite taking your meds
Call your doctor or pharmacist. They can check blood levels-like TSH, INR, or glucose-to see if your meds are still effective. You might need a dose adjustment. Don’t change your meds on your own.
Also, check your fiber supplement. Not all are the same. Psyllium is the most likely to cause problems. Methylcellulose is less gel-forming and may be safer. But still-timing matters.
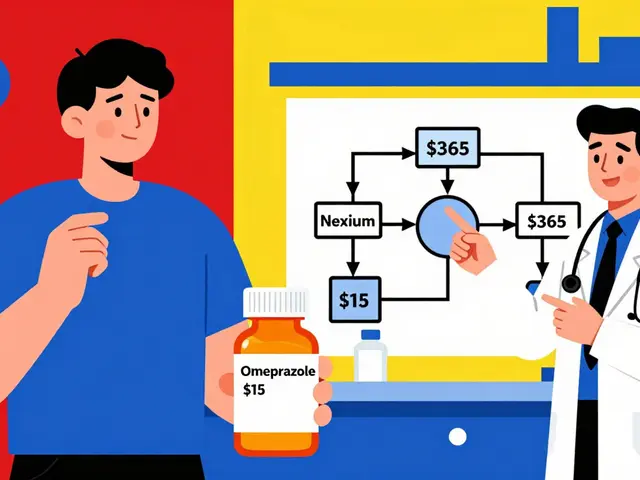
What’s Next? New Fiber Formulas in the Works
Pharmaceutical companies are working on solutions. There are already time-release fiber formulas in Phase 2 clinical trials. These are designed to release fiber slowly, so the gel forms later in the gut-after most drugs have been absorbed. That could change everything.
But until then, the old advice still holds: separate fiber from meds by at least two hours. It’s simple, proven, and life-saving.
The fiber supplement market is growing fast-projected to hit $3.7 billion by 2030. More people are using it than ever. But only 39% of patients get clear timing instructions from their pharmacist. Don’t be one of them. Ask. Write it down. Set a reminder. Your meds depend on it.
Can I take fiber and vitamins at the same time?
It’s safer to separate them. Fiber can bind to minerals like iron, zinc, calcium, and magnesium, reducing how much your body absorbs. Take vitamins at least two hours before or after your fiber supplement. If you take a multivitamin in the morning with breakfast, take fiber at lunch or dinner.
Is psyllium the worst fiber for medication interactions?
Yes, psyllium is the most problematic because it forms the thickest, stickiest gel. Methylcellulose and calcium polycarbophil are less likely to interfere because they don’t gel as much. But even these should be separated from meds by at least one hour. Don’t assume a different fiber is safe just because it’s labeled “gentle.”
What if I forget and take them together?
One mistake won’t ruin your treatment, but it shouldn’t become a habit. If it happens once, don’t double your next dose. Just go back to your regular schedule. If it happens often, your meds may not be working as well. Talk to your doctor about checking blood levels or adjusting your timing.
Can I take fiber at bedtime if I take meds in the morning?
Technically, yes-if your meds are gone from your system by then. But practically, no. Fiber taken before bed causes bloating and gas in 68% of users, according to clinical reports. It can disrupt sleep and make you feel worse. Better to take fiber in the morning after your meds, or at lunchtime.
Do fiber gummies or powders interact differently?
No. The form doesn’t matter-it’s the fiber type and amount that counts. A gummy with 3 grams of psyllium acts the same as a powder with the same amount. Check the ingredient label. If it says “psyllium husk,” treat it like any other fiber supplement and separate it from your meds.



Janice Holmes
December 28, 2025 AT 19:38This is the most important post I’ve read all year. I was taking Metamucil with my levothyroxine like a dumbass-now my TSH is finally normal. I almost died from fatigue. I mean, I was sleeping 12 hours a day and still felt like a zombie. My endocrinologist didn’t even mention fiber. The system is broken. Someone needs to sue the pharmaceutical industry for not labeling this on every bottle. I’m not mad-I’m just… devastated. And also, I’m telling everyone. Everyone. This is a public health crisis.
Olivia Goolsby
December 29, 2025 AT 20:31Let me guess-this is all part of the Big Pharma, Big Fiber, Big Gummy Bear Conspiracy™. Who really benefits from you spacing out your meds? The corporations. They want you to buy MORE supplements, MORE pills, MORE apps to track your ‘timing.’ Did you know psyllium is patented by three different pharmaceutical giants? And the FDA? They’re owned by the same lobbyists who wrote the Dietary Supplement Health and Education Act-back in 1994, when they also allowed aspartame to be classified as ‘generally recognized as safe.’ The 2-hour rule? A distraction. The real issue? Your gut is being poisoned by glyphosate-laced fiber. I’ve been taking methylcellulose with my meds for 17 years-my INR is perfect. They just don’t want you to know the truth.
Gerald Tardif
December 31, 2025 AT 18:19Man, I’ve been there. Took fiber with my metformin for months-blood sugar went nuts. Started setting alarms: 7 a.m. pill, 10 a.m. fiber. No more spikes. No more panic. I didn’t even know this was a thing until I read this. Honestly? This post saved my health. You don’t need a PhD to get it: separate them. Simple. Clean. Effective. If you’re reading this and you’re on meds-do yourself a favor. Write it down. Set the damn alarm. You’ll thank yourself in six weeks.
Monika Naumann
December 31, 2025 AT 20:57It is deeply concerning that Western medical practices continue to neglect the foundational wisdom of Ayurvedic and Traditional Chinese Medicine, which have, for millennia, emphasized the importance of temporal separation between medicinal herbs and dietary fibers. In India, we have always taken Triphala after meals, never with allopathic drugs. This is not new science-it is ancient science, ignored by those who profit from confusion. The American healthcare system must cease its obsession with pharmaceutical convenience and return to disciplined, patient-centered timing protocols. Your body is not a vending machine.
Elizabeth Ganak
January 2, 2026 AT 06:42Thank you so much for this! I’ve been taking fiber with my blood pressure meds and didn’t realize why my readings were all over the place. I just moved my fiber to lunch and my BP is finally stable. I used to feel so guilty for forgetting, but now I know it’s not me-it’s the system. I’m gonna print this out and give it to my mom. She’s on warfarin and takes Metamucil every night. She’s gonna be so relieved.
Raushan Richardson
January 4, 2026 AT 01:19Y’all, I just told my whole book club about this. We’re all on something-thyroid, diabetes, cholesterol-and NONE of us knew this. I’m making a little cheat sheet: ‘Fiber = 2 hours away.’ I taped it to my pill organizer. My life is so much calmer now. Also-hydration. Drink water. Like, a lot. I thought I was fine until I started getting cramps. Now I carry a bottle everywhere. Small changes, huge impact. You got this.
Liz Tanner
January 4, 2026 AT 06:37I’m a pharmacist, and I’ve seen this too many times. Patients come in with ‘unexplained’ lab abnormalities-TSH up, INR erratic, glucose out of range-and when I ask about supplements, they say, ‘Oh, I just take my fiber with my morning coffee.’ It’s heartbreaking. The truth? Most of them were never told. Not by their doctor. Not by their pharmacist. Not even by the supplement bottle. This isn’t about being perfect-it’s about being aware. One hour isn’t enough. Two to four is the gold standard. And if you’re on statins? Talk to your provider. Don’t assume psyllium helps-it’s not universal. Knowledge is power. Share this.
Nikki Thames
January 4, 2026 AT 17:05Let us not be fooled by this superficially rational facade. You believe you are exercising agency by ‘timing’ your fiber-but in truth, you are submitting to a new orthodoxy. The body is not a machine to be calibrated. The gut is a sacred, ancient ecosystem. To impose rigid temporal divisions upon digestion is to reject the natural rhythm of life. Why not let the body decide? Why not take your pills and fiber together, and let your intuition guide you? The medical establishment fears this. They fear chaos. They fear the unknown. But I? I embrace the mystery. And so should you.
James Bowers
January 6, 2026 AT 13:40According to the 2020 Journal of Clinical Pharmacology meta-analysis, psyllium reduces levothyroxine absorption by 28.7% (95% CI: 24.1–33.3%; p < 0.001). Methylcellulose reduces it by 9.2% (CI: 5.8–12.6%). The clinical significance of this is non-trivial. Furthermore, the pharmacokinetic half-life of levothyroxine is 7 days. A single ingestion error does not immediately alter TSH. However, chronic co-administration results in cumulative subtherapeutic exposure. Therefore, the recommended separation window of 2–4 hours is evidence-based, not anecdotal. This is not opinion. This is pharmacology.
Will Neitzer
January 8, 2026 AT 10:25Just want to say thank you to the OP. This is exactly the kind of practical, life-saving info we need more of. I used to take fiber at night because it ‘helped me sleep.’ Turns out, it was wrecking my blood pressure meds. I switched to lunchtime fiber, started drinking more water, and my BP dropped 15 points. No new meds. No side effects. Just timing. I’m not a genius-I just listened. If you’re reading this and you’re on meds? Please, don’t wait until you feel sick. Check your labels. Ask your pharmacist. Write it down. Your future self will cry happy tears.
Babe Addict
January 8, 2026 AT 11:15Everyone’s overcomplicating this. You know what really blocks absorption? Sugar. And processed carbs. And gluten. Fiber? Nah. It’s just a placebo for people who don’t trust their own digestion. I take psyllium with my metformin and my thyroid med and my statin and my multivitamin-and I’ve never felt better. My blood work? Perfect. My energy? Sky-high. The science? Correlation isn’t causation. You’re all falling for the medical-industrial complex’s fear-mongering. Real men don’t time their fiber. Real men eat, take pills, and live.