Melanoma doesn’t always look like a scary mole. Sometimes it’s a tiny spot that doesn’t fade. Other times, it’s a bump that bleeds without injury. And if you miss it? The chances of survival drop fast. In 2025, the American Cancer Society reports that when melanoma is caught early-before it spreads-more than 99% of patients live at least five years. But if it’s found after spreading to other organs, that number plummets to just 32%. That’s not a statistic. That’s a life-or-death gap. And it’s why early detection and modern immunotherapy are no longer optional. They’re the only things standing between a routine check-up and a death sentence.
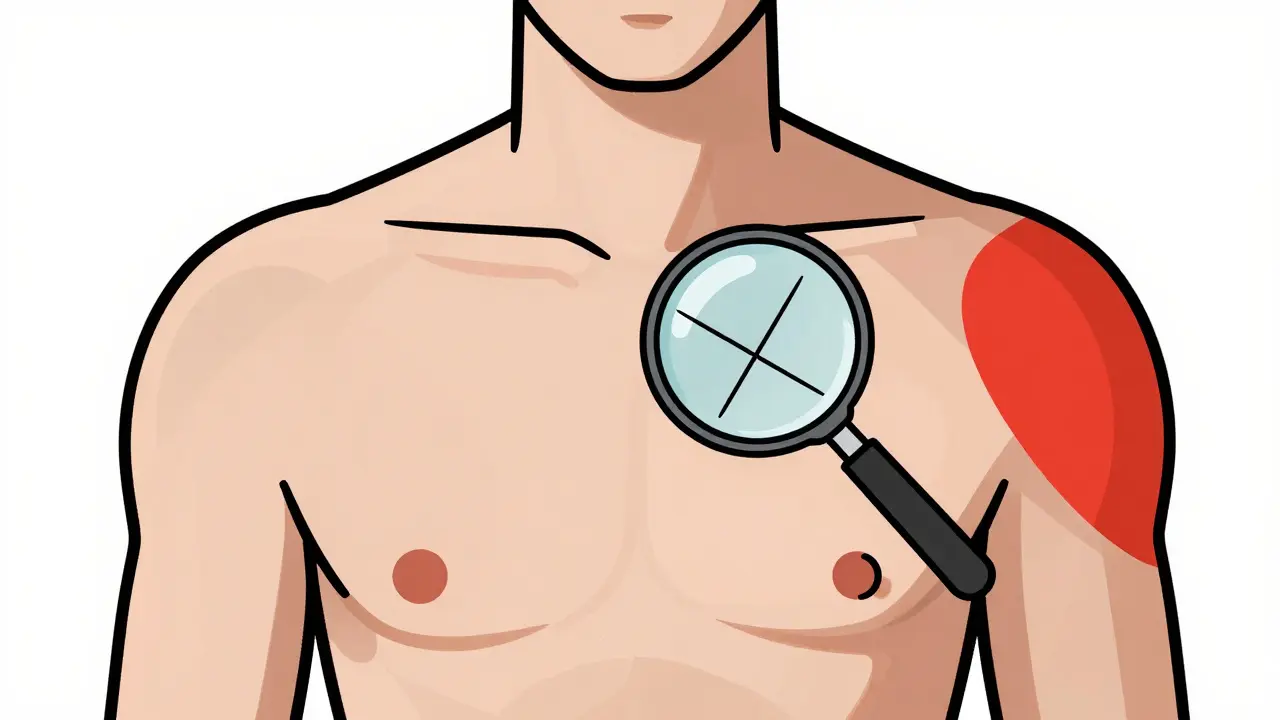
What Melanoma Really Looks Like (And What It Doesn’t)
Most people think melanoma means a dark, uneven mole. That’s true sometimes. But it’s not the whole story. Melanoma can be pink, red, or even skin-colored. It can look like a scar. Or a pimple that won’t go away. The ABCDE rule still holds: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolving size or shape. But even that isn’t enough. Studies show primary care doctors miss up to 40% of melanomas during visual exams. That’s why tools are now stepping in.
One of the biggest breakthroughs isn’t a drug-it’s a camera. Devices like DermaSensor, approved by the FDA in early 2024, use near-infrared light to measure how skin scatters and absorbs energy. Normal skin and cancerous skin react differently. The device picks up those differences in seconds. In trials, it gave primary care providers an 85-95% sensitivity rate-meaning it caught almost all real melanomas. But here’s the catch: its specificity was only 26-40%. That means for every 100 healthy spots it flagged, 60-74 were false alarms. More biopsies. More anxiety. More cost.
AI Is Changing the Game-But It’s Not Perfect
Artificial intelligence is now reading skin images better than most humans. At Northeastern University, researchers built SegFusion, a system that first isolates the exact shape of a mole, then analyzes its texture and color patterns. It hits 99% accuracy. That’s not a guess. That’s from peer-reviewed data published in March 2025. It works by training on thousands of images, including ones from the ISIC 2020 dataset, where melanoma cases made up just 1.8% of the total. The system compensated by artificially boosting those rare cases so the AI wouldn’t ignore them.
Other models like DenseNet-201 and ResNet-50 have hit accuracy rates above 94% on standardized image sets. But real life isn’t a lab. Skin tones vary. Lighting changes. Moles get blurry. And most AI tools were trained mostly on light skin. A March 2025 JAMA Dermatology study found these systems perform 12-15% worse on darker skin tones. That’s not a small gap. It’s a dangerous blind spot.
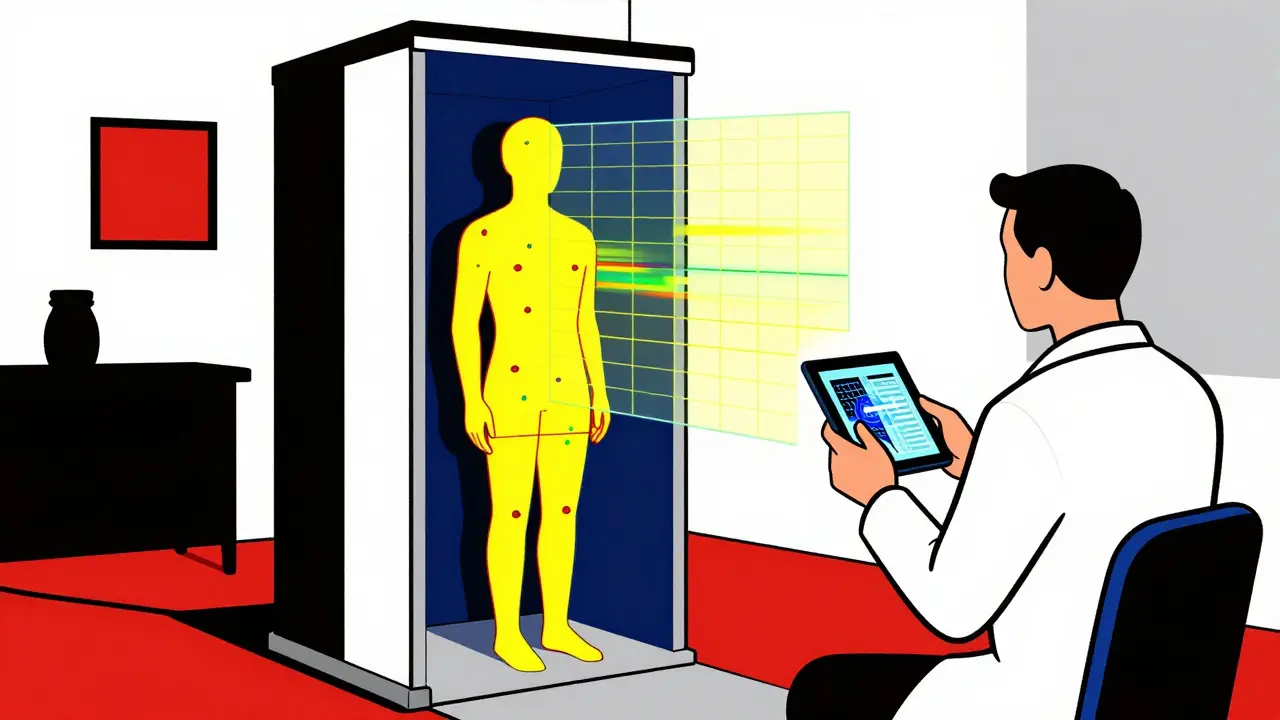
That’s why systems like iToBoS, funded by the EU and led by Fraunhofer Institute, are trying something different. Instead of just looking at one mole, it scans your whole body in six minutes. It maps every spot. It flags anything unusual. And it doesn’t just say “cancer.” It shows the doctor *why*-using explainable AI. You see the heatmap. You see the edge detection. You see the comparison to known melanomas. That transparency builds trust. And trust matters when you’re deciding whether to cut into someone’s skin.
Wearable Patches and At-Home Screening
What if you didn’t have to wait for a doctor? What if your skin could tell you something was wrong-before you even noticed it?
At Wake Forest University, Dr. Mohammad J. Moghimi’s team developed a battery-free, wireless patch that sticks to suspicious moles. It doesn’t take pictures. It measures electrical resistance in the tissue. Cancer cells change how electricity moves through skin. The patch picks that up and sends the data to a small reader. In a pilot with 10 volunteers, the difference between healthy and cancerous tissue was statistically clear. The patch is comfortable. It’s cheap. And it could be used daily at home.
But it’s still early. Only 10 people. No large-scale trials yet. And it can’t tell if a spot is benign or malignant-just that something’s off. Still, for people with dozens of moles, or a family history of melanoma, it could be the early warning they need. The team is now testing conductive hydrogel electrodes to make the contact even better.
Immunotherapy: When Your Immune System Becomes the Weapon
For decades, melanoma that spread was a death sentence. Chemo didn’t work well. Radiation helped only temporarily. Then came immunotherapy.
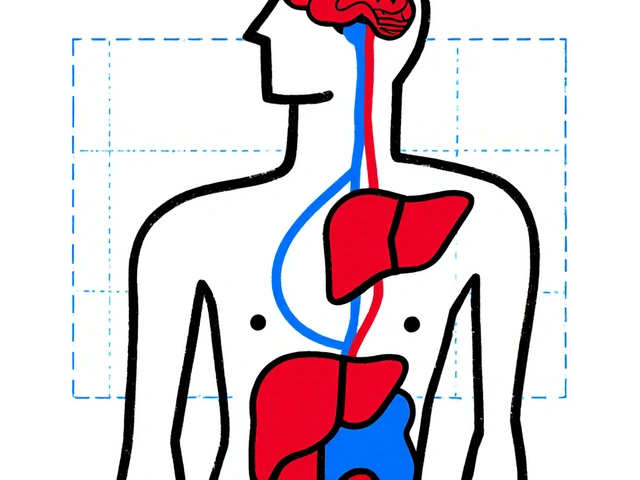
In 2011, the FDA approved ipilimumab-the first drug to show it was possible to make the body’s own immune system attack melanoma. It wasn’t perfect. Side effects were brutal. But it worked. And it opened the door.
Today, the standard is combination therapy. Drugs like pembrolizumab and nivolumab block PD-1, a brake on immune cells. Drugs like relatlimab block LAG-3. And some patients get both PD-1 and CTLA-4 inhibitors together. These aren’t just treatments. They’re life extenders. In clinical trials, over half of patients with advanced melanoma saw their tumors shrink. A third had no signs of cancer after two years. That’s unheard of in the past.
Now, the next wave is coming. Regeneron’s fianlimab, paired with a PD-1 blocker, is showing even stronger results in Phase 3 trials. And IMA203 PRAME cell therapy, currently in the SUPRAME trial, is designed to train a patient’s own immune cells to hunt down melanoma cells with a specific marker. In early tests, 56% of patients had complete responses. That’s not a cure-but it’s close.
The Real Problem: Overdiagnosis and Inequality
More tools mean more detection. But more detection doesn’t always mean better outcomes. A 2025 paper in Taylor & Francis warned that we’re seeing a rise in overdiagnosis. That means finding slow-growing melanomas that would’ve never harmed anyone. We cut them out. We scar them. We stress them. And for what? No survival benefit. Just extra surgery.
And then there’s access. These new AI tools, full-body scanners, and smart patches cost money. Most are still in clinics in the U.S., Germany, and Japan. In rural Australia, or in low-income countries, they’re science fiction. Even in Sydney, not every GP has access to DermaSensor. And insurance doesn’t always cover it. The FDA has cleared 17 AI tools for melanoma since 2022. But getting them into clinics? That takes weeks of training, IT integration, and staff buy-in. One dermatology practice reported 20 hours of training per doctor just to use one system.
Meanwhile, the global melanoma diagnostics market hit $2.87 billion in 2024. Companies like DermTech are thriving. Google Health pulled its AI tool from the market in late 2024-not because it didn’t work, but because insurers wouldn’t pay for it. That’s the real barrier now. Not the tech. The money.

What You Can Do Right Now
You don’t need a scanner. You don’t need AI. You need to look.
- Check your skin monthly. Use a mirror. Take a photo of new or changing spots.
- Don’t ignore spots that bleed, itch, or don’t heal.
- Know your risk: fair skin, sunburns as a kid, family history, over 50-these raise your odds.
- If you’re high risk, ask your doctor about dermoscopy. It’s free or low-cost in most clinics.
- Wear sunscreen. Not just at the beach. Every day. UV damage adds up.
And if you’re worried about a spot? Don’t wait. Don’t Google it. See a dermatologist. Even if you think it’s nothing. Because melanoma doesn’t ask for permission. It grows silently. And when it spreads? It’s too late for most.
The Future Is Here-But It’s Not Fair
By 2030, AI-assisted detection could become standard. Immunotherapy will keep improving. We might even see blood tests that catch melanoma before it shows on the skin. But progress won’t help everyone equally. The tools exist. The science is solid. What’s missing is equity.
For now, the best defense is still you. Know your body. Speak up. Get checked. And if your doctor dismisses you? Find another one. Melanoma doesn’t care if you’re rich or poor. But your survival? That depends on how fast you act.
Can melanoma be detected before it becomes visible?
Not yet with certainty. But emerging tools like wearable bioimpedance patches and blood-based biomarker tests are being tested in clinical trials. The Wake Forest patch measures electrical changes in skin tissue that may signal cancer before a mole looks abnormal. These aren’t available for public use yet, but early results show promise. For now, visual inspection and dermoscopy remain the only proven methods.
Is immunotherapy better than chemotherapy for melanoma?
Yes-for advanced melanoma, immunotherapy is now the first-line treatment. Chemotherapy rarely works well against melanoma and causes more side effects. Immunotherapy drugs like pembrolizumab and nivolumab help the body’s immune system target cancer cells directly. In clinical trials, they’ve doubled survival rates compared to chemotherapy. Some patients have lived for years with no signs of cancer. That’s why chemotherapy is now only used when immunotherapy fails.
Do AI skin scanners replace dermatologists?
No. They assist. AI tools like SegFusion and iToBoS can flag suspicious lesions with high accuracy, but they can’t replace a dermatologist’s judgment. A scan might miss a lesion in a hard-to-image area like the scalp or between toes. It can’t assess symptoms like itching or bleeding. And it doesn’t know your medical history. The best outcome comes when AI highlights a problem, and a human confirms it with a biopsy and clinical context.
Are these new detection tools covered by insurance?
It depends. DermaSensor and similar devices are FDA-approved, but insurance coverage varies. Medicare and some private insurers cover dermoscopy and biopsy, but not always AI-assisted screening. In the U.S., reimbursement is the biggest hurdle. Many clinics can’t afford to buy the tech because insurers won’t pay for it. In Australia, public health systems rarely fund experimental tools. Always check with your provider before assuming coverage.
How often should I get a skin check?
If you have no risk factors, a full-body skin exam every 1-2 years is enough. If you’ve had melanoma before, have many moles, a family history, or fair skin, you should be checked every 6 months. High-risk patients may need dermoscopy or digital monitoring of specific moles. Monthly self-checks are essential for everyone. Don’t wait for symptoms. Melanoma often shows no pain or discomfort until it’s advanced.
Can melanoma come back after immunotherapy?
Yes. Even if the cancer disappears, it can return. Immunotherapy doesn’t always eliminate every cancer cell. Some patients relapse within a year. Others stay in remission for five years or more. That’s why long-term follow-up is critical. Doctors now monitor blood markers and do regular scans for years after treatment. If melanoma returns, new immunotherapy combinations or clinical trials may still offer options.



Tony Du bled
December 22, 2025 AT 05:34Been checking my moles every month since my cousin got diagnosed. Still don’t trust those apps. Saw a spot that looked fine on the AI scan but turned out to be melanoma. Human eyes still win.
Vikrant Sura
December 23, 2025 AT 16:34AI tools are just fancy marketing. Dermatologists make $400/hour. Why would they want you to diagnose yourself with a $20 patch?
Ajay Brahmandam
December 24, 2025 AT 21:54My dad’s a farmer in Kerala. He’s got 12 moles and never seen a dermatologist. Still alive at 72. Sunscreen? He uses coconut oil. Maybe we’re overcomplicating this.
Johnnie R. Bailey
December 25, 2025 AT 04:22There’s a quiet tragedy here: we’ve built machines that can see cancer before the eye can, but we’ve failed to build a system that lets everyone use them. The tech isn’t the barrier-it’s our refusal to treat health as a right, not a privilege. This isn’t innovation. It’s inequality with a Wi-Fi connection.
Aliyu Sani
December 25, 2025 AT 07:39Immunotherapy? Sounds like voodoo science. My cousin took that shit and his immune system went full war mode-got hospitalized for 3 weeks. Now he’s fine, but damn… why not just cut it out like they did in the 90s?
Kathryn Weymouth
December 26, 2025 AT 20:25One of the most concerning gaps in the literature is the lack of longitudinal data on AI-assisted screening in non-Caucasian populations. The JAMA study you cited is critical, but we need to see outcomes over five years-not just accuracy on static images. Otherwise, we’re optimizing for metrics, not lives.
Herman Rousseau
December 28, 2025 AT 01:10My sister’s a dermatologist in Ohio. She says the biggest win isn’t the fancy scanner-it’s the patient who finally says, ‘Hey, this spot’s been there for 3 years and it’s changing.’ Early detection starts with awareness, not AI. Keep checking your skin. You’re your own best tool.
Jeremy Hendriks
December 28, 2025 AT 15:32They’re selling us salvation wrapped in algorithms. But what if the real problem isn’t detection? What if it’s that we’ve normalized death as inevitable unless we pay for the latest gadget? We’ve turned survival into a subscription service.
Sai Keerthan Reddy Proddatoori
December 29, 2025 AT 23:41USA spends billions on AI skin scanners but can’t fix the water in Flint. This is what happens when you let corporations run medicine. They don’t want you healthy-they want you paying forever. The patch? It’s a trap. They’ll charge you $500/month for it. Then bill you for the biopsy it causes.
Gabriella da Silva Mendes
December 30, 2025 AT 14:19OMG I JUST REALIZED MY NECK SPOT IS ASYMMETRIC 😱 I’ve had it for 5 years but now I’m panicking. WHO DO I CALL?? IS THIS IT?? I’M TOO YOUNG TO DIE!! 🥲🩺💔
Art Van Gelder
December 31, 2025 AT 15:44Think about this: we’ve trained neural nets to recognize cancer with 99% accuracy, yet we still can’t get insurance companies to cover a $200 device because it’s ‘not cost-effective.’ We’ve created a world where a machine can save your life, but a spreadsheet decides whether you get to live. The tragedy isn’t the disease-it’s the system that profits from your fear while refusing to fix the access problem.
Cara Hritz
December 31, 2025 AT 23:55Wait, so the AI works better on white skin? That’s wild. So if you’re brown, you’re basically just supposed to hope you don’t get it? Or just die? That’s not science. That’s systemic neglect.
jenny guachamboza
January 1, 2026 AT 01:24Did you know the FDA approved those scanners because Google paid them? It’s all a lie. The real cause of melanoma is 5G radiation + chemtrails. The patches? They’re just tracking your DNA. I saw a guy on TruthSocial say his skin glowed blue after using one. He vanished. 👁️🗨️
Candy Cotton
January 3, 2026 AT 00:31While the technological advancements referenced in this article are indeed noteworthy, it is imperative to acknowledge that the current regulatory and reimbursement frameworks remain woefully inadequate to ensure equitable dissemination. The market-driven paradigm, as evidenced by Google Health’s withdrawal, underscores a fundamental misalignment between clinical utility and fiscal viability. Consequently, the ethical imperative to prioritize public health over corporate profitability remains unmet.