Every year, millions of people reach for ibuprofen or naproxen to ease a headache, back pain, or arthritis flare-up. It’s quick, it’s easy, and it’s available over the counter. But what most users don’t realize is that these common painkillers carry hidden dangers-especially to the stomach and kidneys. NSAID safety isn’t just about taking the right dose; it’s about understanding who’s at risk and how to spot trouble before it becomes life-threatening.
How NSAIDs Damage the Gut
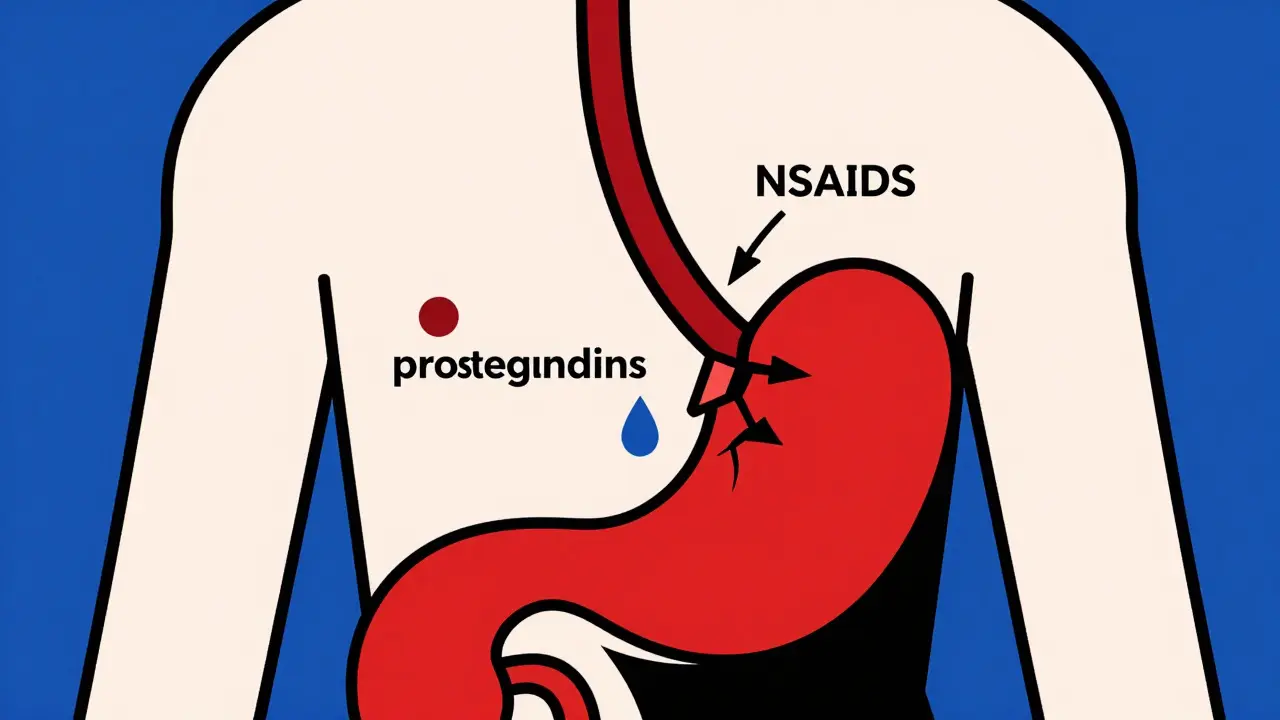
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 is involved in inflammation and pain, so blocking it helps reduce swelling. But COX-1? That’s the enzyme that protects your stomach lining by producing prostaglandins-natural chemicals that keep the mucus barrier thick and blood flow steady. When NSAIDs shut down COX-1, that protective layer thins out. The result? Acid starts eating away at the stomach or duodenum.This isn’t just about heartburn. About 15% of people who take NSAIDs long-term develop peptic ulcers. And here’s the scary part: half of those ulcers show up with zero warning. No pain. No nausea. Just sudden bleeding-sometimes so slow it only shows up as iron-deficiency anemia, or so fast it causes black, tarry stools or vomiting blood. The American College of Gastroenterology reports NSAIDs cause over 100,000 hospitalizations and 16,500 deaths in the U.S. each year. Most of these are preventable.
Lower GI damage is even harder to catch. NSAIDs can cause tiny tears and inflammation in the small intestine, leading to chronic bleeding, protein loss, and even perforation. Unlike stomach ulcers, there’s no reliable test to screen for this damage. No endoscopy, no blood work-it’s a silent thief.
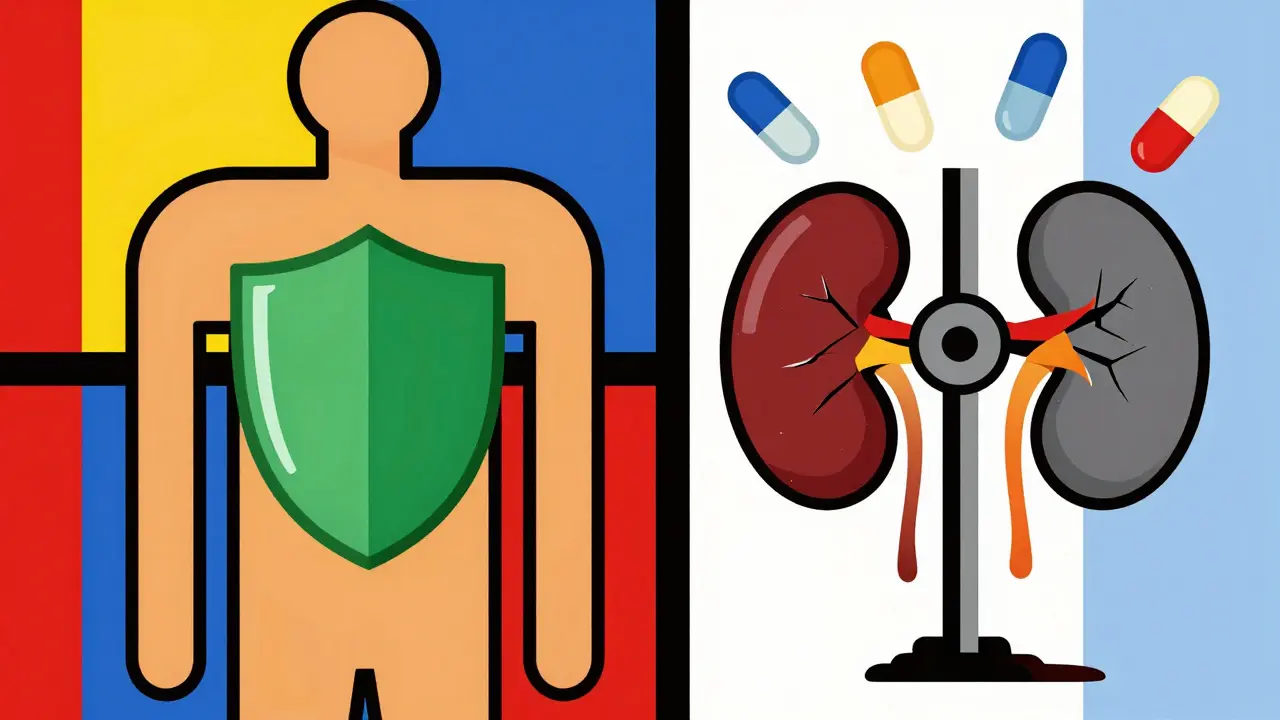
Kidney Risks You Can’t Ignore
Your kidneys rely on prostaglandins to maintain blood flow, especially when you’re dehydrated, sick, or have high blood pressure. NSAIDs block those signals. When that happens, your kidneys get less blood, and filtration drops. That’s how you get acute kidney injury-even if you’ve never had kidney problems before.Studies show 1% to 5% of NSAID users develop sudden kidney damage. In older adults or those with existing kidney disease, that number jumps. Chronic use can lead to interstitial nephritis, papillary necrosis, or even permanent loss of function. The FDA now requires a boxed warning on all prescription NSAIDs for kidney risks in people over 65. And it’s not just about the dose-it’s about duration. Each extra week of use raises the risk by 3% to 5%.
People with heart failure, diabetes, or high blood pressure are at highest risk. If you’re on diuretics or ACE inhibitors, combining them with NSAIDs is like pouring gasoline on a fire. Your kidneys can’t handle the double hit.
Which NSAIDs Are Safer? The Real Differences
Not all NSAIDs are created equal. Naproxen, for example, carries a 4.2 times higher risk of upper GI bleeding than someone not taking NSAIDs. Ibuprofen? It’s 2.7 times riskier than celecoxib. Celecoxib, a COX-2 selective inhibitor, was designed to spare the stomach-and it does. But it’s not risk-free. In patients with heart disease, it can raise the risk of heart attack or stroke.Here’s the trade-off: COX-2 inhibitors like celecoxib are gentler on the stomach, but harder on the heart. Non-selective NSAIDs like ibuprofen and naproxen are easier on the heart but brutal on the gut. And don’t assume OTC means safe. Taking 800 mg of ibuprofen three times a day for weeks is the same as a prescription dose-and just as dangerous.
One study found that 31% of celecoxib users reported leg swelling-signs of fluid retention that can stress the kidneys. Meanwhile, 42% of ibuprofen users on WebMD cited “stomach bleeding without warning” as their biggest fear. There’s no perfect option. Only the least risky one-for your body.
Who’s at Highest Risk?
Some people shouldn’t touch NSAIDs at all. The American College of Gastroenterology has a simple scoring system:- Age 65 or older: +2 points
- History of peptic ulcer: +3 points
- Taking blood thinners (warfarin, apixaban): +2 points
- Using corticosteroids: +1 point
If you score 4 or more, you’re high risk. That means even a single dose could trigger bleeding. Age 75 or older? History of ulcers? On multiple meds? You need an endoscopy before starting NSAIDs-not after symptoms appear.
Also watch for drug combos. Taking NSAIDs with SSRIs (like fluoxetine or sertraline) increases bleeding risk by over 3 times. Same goes with corticosteroids. Even a low-dose prednisone pill can turn a safe NSAID into a danger zone.
Monitoring: What Doctors Should Check-and Often Don’t
Most patients start NSAIDs with no follow-up. That’s a mistake. Here’s what should happen:- Baseline blood test: creatinine and BUN to check kidney function
- Complete blood count: to catch early signs of anemia from hidden bleeding
- Fecal occult blood test: every 6 months for high-risk users
- Repeat creatinine: within 30 days of starting, then every 3-6 months if used long-term
But here’s the truth: only 52% of NSAID users have their creatinine checked within 90 days. That’s according to a 2023 Medicare analysis. Doctors often forget. Patients don’t know to ask. And pharmacies don’t flag it.
That’s why some health systems now use automated alerts in electronic records. If a patient over 70 with diabetes gets a new NSAID prescription, the system pops up: “Check renal function. Consider PPI.” These tools cut complications by over 30% in veteran populations.
The PPI Paradox: Protecting the Stomach, Hurting the Gut
Many doctors automatically prescribe proton pump inhibitors (PPIs) like omeprazole alongside NSAIDs. It makes sense-PPIs reduce stomach acid, so ulcers are less likely. And yes, they cut ulcer risk by 70-90%.But here’s the catch: PPIs don’t protect the small intestine. And they create new problems. A 2022 study found that using NSAIDs with PPIs for 4-12 months increases the risk of microscopic colitis by over 6 times. That’s chronic, watery diarrhea that can last for months. It’s not rare. It’s not minor. And it’s often misdiagnosed as IBS.
Dr. Kenneth Mahaffey calls this the “therapeutic paradox.” We’re trading one problem for another. And for many, the trade isn’t worth it.
What Should You Do?
If you’re on NSAIDs long-term, here’s your action plan:- Ask: “Is this really necessary?” Sometimes physical therapy, weight loss, or heat therapy works just as well.
- Use the lowest dose for the shortest time. Never take more than 1200 mg of ibuprofen per day unless directed.
- Get a baseline blood test before starting. Ask for creatinine and CBC.
- Watch for signs: dark stools, fatigue, swelling in legs, unexplained diarrhea.
- If you’re over 65, have a history of ulcers, or take blood thinners, insist on a gastroprotection plan-and ask if it includes a PPI or if an alternative exists.
- Don’t assume OTC is safe. Four pills a day for two weeks is still chronic use.
And if you’ve been taking NSAIDs for months without a check-up? Schedule one. Now. Don’t wait for pain. Don’t wait for bleeding. Because by then, it might be too late.
What’s Next? New Tools and Hope
There’s progress. In 2023, the FDA approved naproxcinod-a new NSAID that releases nitric oxide to protect blood vessels and the gut lining. In trials, it caused 58% fewer ulcers than naproxen. And in 2024, a new fecal test (FIT) specifically designed for NSAID users hit the market. It detects hidden bleeding with 92% accuracy.AI is also stepping in. European researchers are training algorithms to spot early signs of intestinal damage during routine colonoscopies. And with celecoxib’s patent expiring in 2025, cheaper, safer alternatives may soon become available.
But until then, the safest NSAID is the one you don’t take. And the smartest move? Know your risks. Monitor your body. Ask questions. Because pain relief shouldn’t cost you your stomach-or your kidneys.
Can I take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and reduce the effectiveness of blood pressure medications like ACE inhibitors or diuretics. If you have high blood pressure, avoid long-term NSAID use. If you must use them, monitor your blood pressure closely and check kidney function every 30 days. Naproxen may be slightly safer than ibuprofen for blood pressure, but it’s still risky. Talk to your doctor before starting.
Is it safe to take ibuprofen every day for arthritis?
No. Daily use of ibuprofen-even at OTC doses-increases the risk of ulcers, kidney damage, and heart problems over time. The American College of Rheumatology recommends limiting NSAID use to the shortest duration possible. For chronic arthritis, consider alternatives like physical therapy, weight management, or acetaminophen (if liver function is normal). If NSAIDs are unavoidable, use the lowest effective dose and combine with a PPI only if you’re high risk.
Do NSAIDs cause kidney damage in healthy people?
Yes. Even healthy people can develop acute kidney injury from NSAIDs, especially if they’re dehydrated, exercising intensely, or taking them during illness. The risk is low for occasional use, but rises sharply with daily or prolonged use. One study found 1% of healthy NSAID users developed sudden kidney failure. If you’re using NSAIDs regularly, get a basic kidney blood test once a year.
What are the signs of NSAID-induced bleeding?
Signs include black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, unexplained fatigue or dizziness (from anemia), and pale skin. Sometimes bleeding is silent-only found through blood tests showing low hemoglobin or iron. If you’re on NSAIDs and notice any of these, stop the medication and see a doctor immediately. Don’t wait.
Can I take a PPI with NSAIDs to prevent stomach problems?
PPIs reduce the risk of stomach ulcers by 70-90%, so they’re often recommended for high-risk patients. But they don’t protect the small intestine, and long-term use (over 4 months) can increase the risk of microscopic colitis, a condition causing chronic diarrhea. PPIs also interfere with nutrient absorption and may raise the risk of bone fractures and infections. Use them only if you’re at high risk for ulcers, and only for the shortest time needed.