Let’s be honest: taking medicine every day is hard. Not because you’re lazy or forgetful - but because the pills make you feel worse. Nausea. Dizziness. Fatigue. Dry mouth. Sleepless nights. These aren’t just inconveniences. For many people, they’re the reason they stop taking their meds altogether. And it’s happening more than you think.
Why People Stop Taking Their Medication
One in two people with chronic conditions like high blood pressure, diabetes, or depression don’t take their medicine as prescribed. That’s not because they don’t care. It’s because the side effects are real, and they’re overwhelming.
Imagine you’re prescribed a new statin for cholesterol. Your doctor says it’ll cut your risk of a heart attack. But after a week, you’re so tired you can’t get out of bed. You skip a dose. Then another. You tell yourself you’ll start again tomorrow. But tomorrow never comes. You’re not alone. Studies show that side effects are the top reason people stop taking meds - even when they know it’s dangerous.
It’s worse for mental health drugs. People with depression are twice as likely to skip their antidepressants if they feel worse at first. And once they stop, they often stop all their meds - not just the one causing trouble. That’s called medication adherence failure. It’s not about willpower. It’s about feeling trapped between the disease and the drug.
The Hidden Cost of Skipping Pills
Skipping your meds doesn’t just mean your condition gets worse. It means hospitals. Emergency rooms. Lost workdays. Even death.
In the U.S. alone, nonadherence causes around 125,000 preventable deaths every year. That’s more than traffic accidents. It leads to up to 69% of medication-related hospital stays. And the financial toll? Up to $44,000 per person annually in extra care costs.
But here’s the kicker: most of these costs are avoidable. If you’re taking your meds right, you’re less likely to end up in the hospital. Your doctor can adjust your dose. Switch your drug. Or add something to help with side effects. But none of that works if you’re not talking about it.
Side Effects Aren’t Always Listed - and That’s the Problem
Drug labels list common side effects. But they don’t tell you how bad they might feel. Or how long they last. Or that they might get better after a few weeks - if you stick with it.
One patient I know stopped her blood pressure med because she felt dizzy. She didn’t know dizziness often fades after 10-14 days. She thought the drug was making her sick. She wasn’t wrong - but she didn’t have the full picture.
Doctors don’t always bring it up either. Nurses document nonadherence 85% of the time. Pharmacists? Only 52%. That gap means your side effects might be slipping through the cracks. If you don’t mention them, no one will fix them.

What Actually Works to Keep You on Track
There’s no magic pill for adherence. But there are proven ways to stay on track - even when the meds feel rough.
1. Talk to your pharmacist - not just your doctor. Pharmacists are the hidden heroes of adherence. They know your full med list. They’ve seen what works. And they can help you manage side effects without stopping your treatment. Studies show pharmacist-led support can boost adherence by up to 40% in just 90 days.
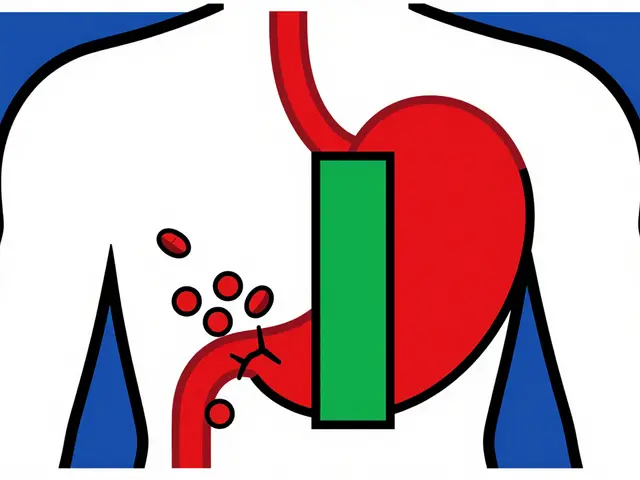
2. Don’t stop cold. Adjust smart. If you’re having side effects, don’t quit. Call your pharmacist or doctor. Ask: “Can we lower the dose?” “Can I take it with food?” “Is there another drug that’s less likely to cause this?” Sometimes, switching from a once-daily pill to a liquid form, or from a brand to a generic, makes all the difference.
3. Use reminders that work for you. Phone alarms? Pill boxes? Apps? Find what sticks. Some people use a simple paper calendar. Others use smart pill dispensers that text when it’s time. The goal isn’t perfection - it’s consistency. Even missing one day a week can lower your treatment’s effectiveness.
4. Track your symptoms. Keep a short log: “Day 3: Headache after pill. Took with breakfast. Felt better.” This helps your provider spot patterns. Maybe the side effect only happens on an empty stomach. Maybe it’s worse when you’re stressed. You can’t fix what you don’t measure.
5. Ask about cost. If you’re skipping doses because the prescription is too expensive, say so. Many pharmacies offer discount programs. Some drugmakers have patient assistance plans. A $50 monthly copay can become $5. That’s not a small thing - it’s the difference between staying on track and giving up.
When Side Effects Are a Red Flag
Not all side effects are minor. Some mean you need to stop immediately.
If you have:
- Swelling of the face, lips, or throat
- Severe rash or blistering skin
- Chest pain or irregular heartbeat
- Unexplained bruising or bleeding
- Thoughts of self-harm or suicide
- call your doctor or go to the ER. These aren’t things to wait out. But for most other side effects - the fatigue, the nausea, the dry mouth - there’s a workaround. You just need to speak up.
It’s Not Just About Taking Pills - It’s About Trust
The biggest barrier to adherence isn’t forgetfulness. It’s fear. Fear that the drug is hurting you more than helping. Fear that no one understands. Fear that you’re being asked to suffer for a benefit you can’t see.
Good care doesn’t just prescribe. It listens. It adjusts. It partners with you.
When pharmacists work with patients to manage side effects, adherence jumps from 74% to 89%. That’s not a miracle. That’s good communication. That’s someone saying: “I hear you. Let’s fix this together.”
And that’s what you deserve.
What You Can Do Today
You don’t need to wait for your next appointment. Start now:
- Write down every side effect you’ve had - even if you think it’s minor.
- Call your pharmacy. Ask: “Can we review my meds and see if any of these side effects can be reduced?”
- Set a reminder to take your pill at the same time every day - even if it’s just for one week.
- Ask yourself: “If I stop this, what’s the risk? And if I keep going, is there a way to make it easier?”
Medication adherence isn’t about being perfect. It’s about staying in the game. And you’re not alone in this. Millions of people are trying to do the same thing - and there are real, practical ways to make it work.
Why do people stop taking their medication even when they know it’s important?
People often stop because of side effects - things like nausea, fatigue, dizziness, or mood changes. Even if they understand the long-term benefits, the daily discomfort feels worse than the risk of not taking the drug. Fear of interactions, lack of clear guidance, and not knowing side effects can improve over time also play a big role.
How common is medication nonadherence due to side effects?
Side effects are the leading cause of nonadherence. Up to 50% of people with chronic conditions don’t take their meds as prescribed, and side effects are the top reason for stopping after the first few weeks. In mental health, patients are twice as likely to skip treatment if side effects are present.
Can side effects be managed without stopping the medication?
Yes. Many side effects can be reduced by changing the time of day you take the pill, taking it with food, lowering the dose, or switching to a different drug in the same class. Pharmacists can help identify these options. For example, switching from a morning statin to an evening one can reduce muscle aches. Sometimes, adding a second, low-dose medication helps manage side effects without losing the benefit.
What role do pharmacists play in improving medication adherence?
Pharmacists are key. They review all your medications, spot interactions, and help manage side effects. Studies show pharmacist-led support increases adherence by up to 40% in 90 days. Face-to-face consultations are the most effective - they’re 83% successful compared to phone calls at 38%. They also help with cost barriers and refill reminders.
Are there tools or apps that help with medication adherence?
Yes. Simple tools like pill boxes with alarms, smartphone apps (like Medisafe or MyTherapy), or smart pill dispensers that send texts work well. The best tool is the one you’ll actually use. Some people prefer paper charts. Others like automated calls. The goal isn’t complexity - it’s consistency. Even a daily alarm set for the same time can make a big difference.
When should I call my doctor about side effects?
Call immediately if you have swelling, trouble breathing, chest pain, severe rash, unexplained bleeding, or thoughts of self-harm. For milder side effects like fatigue, dry mouth, or mild nausea, call within a few days. Don’t wait until your next appointment. Many side effects can be fixed quickly - but only if you speak up.
Is it true that side effects get better over time?
Often, yes. Many side effects - especially from antidepressants, blood pressure meds, and cholesterol drugs - peak in the first week or two and then fade. But you have to keep taking them to find out. That’s why it’s so important to talk to your pharmacist before quitting. They can tell you if what you’re feeling is temporary or something that needs attention.
How much does nonadherence cost the healthcare system?
Nonadherence costs the U.S. healthcare system an estimated $300 billion a year. That includes hospital stays, ER visits, and extra doctor appointments caused by uncontrolled conditions. For individuals, it can mean $1,200 or more in avoidable annual costs. The good news? Improving adherence saves money - and lives.





Cassie Widders
January 12, 2026 AT 10:43Been there. Took my blood pressure med for three days, felt like a zombie, quit. Turns out the dizziness faded after a week. Should’ve called my pharmacist first.
Windie Wilson
January 12, 2026 AT 22:58Oh sweetie, you think this is new? In America we turn pills into a religion and then act shocked when people bail because they feel like garbage. 🤦♀️
Monica Puglia
January 14, 2026 AT 11:30Y’all need to talk to your pharmacist like it’s your BFF 🤗 I did and they switched me to a generic that didn’t wreck my stomach. Also gave me a free pill organizer. Love my pharmacist more than my doctor lol 💊❤️
Rebekah Cobbson
January 16, 2026 AT 08:08Consistency > perfection. Even if you’re late by 2 hours, take it. Your body needs the rhythm. I use a sticky note on my mirror. Works better than any app.
Rinky Tandon
January 17, 2026 AT 15:13Nonadherence is a symptom of Western decadence. In India we take our meds like warriors. No excuses. You feel nauseous? Drink ginger tea. Dizzy? Do pranayama. Stop being weak. Your body is not a fragile porcelain doll. You need discipline not dopamine-driven apps. This is why your healthcare costs are astronomical. You’ve outsourced responsibility to technology and pharmacists. Pathetic.
Darryl Perry
January 18, 2026 AT 18:32Studies show 50% nonadherence yet we keep treating patients like children. The solution isn’t apps or pill boxes. It’s accountability. If you can’t take a pill, you shouldn’t be on the drug. Period. Stop infantilizing adults with behavioral hacks.
Ben Kono
January 19, 2026 AT 10:53My doc prescribed me this new antihypertensive and I felt like I was slowly turning into a ghost. Told him. He said 'it'll pass' so I waited two weeks. It didn't. I switched meds. No drama. No guilt. Just a different pill. Why is this so hard
jordan shiyangeni
January 20, 2026 AT 16:14Let me be clear: the pharmaceutical industry is not your friend. They profit from your nonadherence because it creates downstream medical costs that generate revenue for hospitals, insurers, and specialists. They don’t care if you feel nauseous-they care if you end up in the ER. The fact that pharmacists are the only ones who actually care about your quality of life speaks volumes about the brokenness of the system. We’ve turned healthcare into a transactional nightmare where the patient’s lived experience is secondary to billing codes. This is not medicine. This is corporate logistics with a stethoscope.
Faith Wright
January 20, 2026 AT 17:54My sister stopped her antidepressants because she felt 'numb.' She thought it meant the drug wasn't working. Turns out it meant it was working-she hadn't felt emotionally neutral in years. She cried when she realized. Sometimes the side effect is the antidote to your old pain. We need to reframe this.
Lelia Battle
January 22, 2026 AT 05:54There’s a philosophical paradox here: we are told to trust science, yet when science makes us feel worse, we distrust it. We are asked to surrender control to a pill that may harm us, yet we are blamed for not taking it. The real failure isn’t adherence-it’s a medical system that treats side effects as collateral damage rather than data points. If a drug causes more suffering than relief in the short term, perhaps the problem isn’t the patient’s willpower, but the assumption that all benefits are equal and all harms are negotiable. We need a framework that weighs lived experience as heavily as statistical outcomes.
Abner San Diego
January 23, 2026 AT 10:48Y’all are so obsessed with 'adherence' you forget some people are poor. I take my meds when I can afford them. Sometimes that’s every other day. I don’t have a car to get to the pharmacy. My copay is $45. My rent is $1200. You think I don’t know I’m risking my life? I do. But I’m not a statistic. I’m a human trying to survive. Stop lecturing. Start fixing the system.
Audu ikhlas
January 23, 2026 AT 17:37Why are you listening to Americans about health they dont even know how to eat right. In Nigeria we take herbs and prayer. No pills no apps no nonsense. You think your doctor knows better than our ancestors? Your system is broken. You need to go back to nature not more chemicals. This is why your people are always sick. Too much medicine too little wisdom
Rebekah Cobbson
January 25, 2026 AT 10:52Monica Puglia said she talked to her pharmacist and got a free pill organizer. That’s the kind of care we need. Not more guilt. Not more apps. Just someone who remembers you’re a person, not a chart. Thank you for saying that.