Serotonin Syndrome Risk Checker
Is this medication combination safe for you?
Based on current medical evidence, the risk of serotonin syndrome from combining triptans with antidepressants like SSRIs is virtually non-existent. This tool helps you understand the facts about your specific medications.
Select your medications above and click "Check Safety" to see the evidence-based risk assessment.
For years, patients with migraine who also take antidepressants like SSRIs have been told they can’t use triptans - the most effective acute migraine treatments - because of a supposed risk of serotonin syndrome. It’s a warning that’s stuck in pharmacy systems, echoed by some doctors, and repeated in online forums. But here’s the truth: triptans and SSRIs together do not cause serotonin syndrome in any meaningful way. The fear isn’t based on real-world evidence. It’s based on a misunderstanding that’s been around for nearly two decades.
Where Did the Warning Come From?
In 2006, the U.S. Food and Drug Administration (FDA) issued a safety alert warning that combining triptans with SSRIs or SNRIs could lead to serotonin syndrome. At the time, it made sense on paper. Triptans activate serotonin receptors. SSRIs increase serotonin levels. Put them together, and logic says: too much serotonin = danger. But logic doesn’t always match reality. The FDA’s warning wasn’t based on a single case of serotonin syndrome caused by this combination. It wasn’t backed by clinical trials or patient data. It was a theoretical guess - a pharmacological "what if?" - and it quickly became law in practice. The result? Millions of people with migraine were told to avoid the only treatments that actually stop their headaches. Some switched to weaker painkillers. Others went untreated. Some were even denied triptans by pharmacists who didn’t know any better.What Is Serotonin Syndrome, Really?
Serotonin syndrome is real. It’s serious. And it’s deadly in rare cases. But it doesn’t happen because you take two drugs that touch serotonin. It happens when your brain gets flooded with too much serotonin - usually from overdose, or from mixing drugs that massively boost serotonin across multiple receptor types. The key players in serotonin syndrome are the 5-HT2A and 5-HT1A receptors. Drugs like MAOIs, certain opioids, and high-dose SSRIs can overstimulate these receptors. That’s when symptoms show up: muscle rigidity, high fever, rapid heartbeat, confusion, tremors, and sometimes seizures. Triptans? They don’t work that way. They’re designed to bind only to 5-HT1B and 5-HT1D receptors - the ones that narrow blood vessels in the brain to stop migraine pain. They have almost no effect on 5-HT2A or 5-HT1A. In fact, they don’t even increase serotonin levels in the brain. They just activate specific receptors that already exist. Think of it like this: SSRIs turn up the volume on a whole room of serotonin signals. Triptans are like a remote control that only turns on one specific light in the corner. They don’t add more noise. They just flip one switch.The Evidence That Changed Everything
In 2019, researchers from the University of Washington looked at over 61,000 patients who took both triptans and SSRIs or SNRIs. None of them developed serotonin syndrome. Not one. Not even a borderline case. That study wasn’t an outlier. It confirmed what headache specialists had been seeing for years: the combination is safe. A 2021 survey of 250 neurologists found 89% of them routinely prescribe triptans with SSRIs without any extra monitoring. And in the real world - in clinics, emergency rooms, and patient homes - cases of serotonin syndrome from this combo are virtually nonexistent. Even the FDA’s own adverse event database tells the story. From 2006 to 2022, there were only 18 reports of possible serotonin syndrome involving triptans and SSRIs. Experts reviewed them. Not one was confirmed as true serotonin syndrome. Most were misdiagnosed migraines, flu-like symptoms, or drug side effects. The American Headache Society, the Mayo Clinic, and the European Medicines Agency all agree: the risk is negligible. The FDA warning? It’s outdated.
Why Is the Myth Still Around?
If the science is clear, why do so many people still believe it? One reason: pharmacy software. Most systems still flag triptan-SSRI combinations as dangerous. Pharmacists see the alert and assume it’s a rule - not a suggestion based on old theory. Patients walk away without their meds, confused and frustrated. Another reason: outdated guidelines. Some medical websites still list the FDA warning as fact. UpToDate updated its entry in 2023 to say the risk is "negligible," but many other sources haven’t caught up. And then there’s the fear factor. Serotonin syndrome sounds scary. It’s a term that sticks. People Google it. They read horror stories. They assume the worst. Even when their doctor says it’s fine, they doubt it. A 2022 survey by the American Migraine Foundation found 42% of patients reported being denied triptans because they were on an antidepressant. Not because they had symptoms. Not because their doctor thought it was risky. Just because the system said no.What This Means for You
If you take an SSRI or SNRI for depression, anxiety, or chronic pain - and you have migraine - you do not need to choose between mental health and headache relief. You can have both. You can take sumatriptan, rizatriptan, eletriptan, or any other triptan safely with fluoxetine, sertraline, escitalopram, venlafaxine, or duloxetine. There’s no need to space doses. No need for extra monitoring. No need to avoid one to protect the other. Your doctor doesn’t need to write a special note. Your pharmacist doesn’t need to call for clearance. This isn’t a risky combo. It’s a common, well-studied, and safe one. If you’ve been told you can’t take triptans because of your antidepressant, ask for the evidence. Point them to the 2019 JAMA Neurology study. Show them the American Headache Society’s 2022 statement. Tell them the FDA warning is based on theory - not data.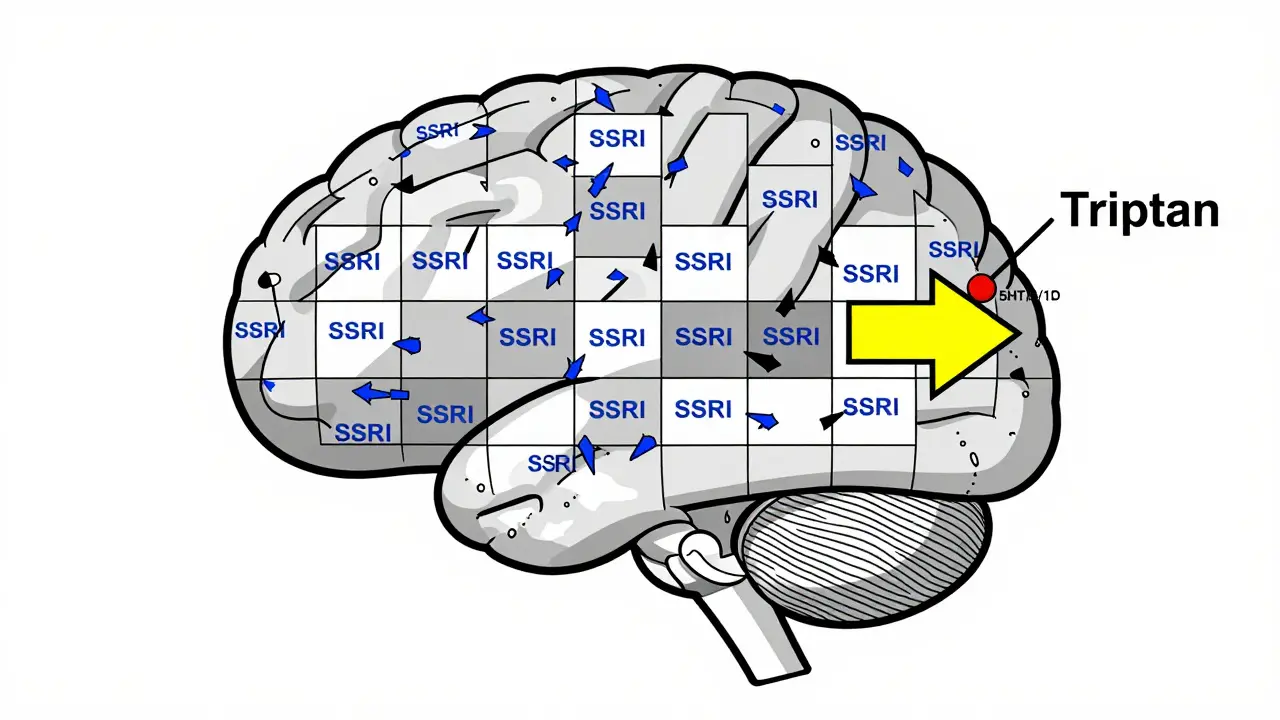
What’s Changing Now?
The tide is turning. More doctors are prescribing triptans with SSRIs without hesitation. More patients are getting the treatment they need. Triptan prescriptions alongside SSRIs have grown from 18.7% in 2007 to over 32% in 2022 - proof that clinicians are listening to the science. Pharmaceutical companies are updating their labels. The 2023 prescribing information for Imitrex (sumatriptan) still mentions the FDA warning - but now adds: "Epidemiological studies have not shown an increased risk of serotonin syndrome with concomitant use of triptans and SSRIs/SNRIs." The American Headache Society and the National Headache Foundation have formally asked the FDA to remove the warning. A major study tracking 10,000 patients on this combination is underway, and early results through 2023 show zero confirmed cases of serotonin syndrome. The European Medicines Agency never issued the warning. Why? Because they waited for real data - not theory. And now, the U.S. is catching up.What to Do If You’re Still Worried
You’re not wrong to be cautious. Medications matter. But here’s what you can do:- If you’re on an SSRI and get a migraine, ask your doctor if a triptan is right for you - don’t assume it’s off-limits.
- If your pharmacist refuses to fill your triptan prescription because of your antidepressant, ask them to check the latest guidelines. Point them to the American Headache Society or UpToDate.
- Know the real symptoms of serotonin syndrome: high fever, stiff muscles, confusion, rapid heart rate, and agitation. If you feel these after taking a triptan, seek help. But know this: they won’t happen just because you took sumatriptan with sertraline.
- If you’ve never had serotonin syndrome on your SSRI alone, you’re extremely unlikely to get it adding a triptan.
The Bottom Line
The idea that triptans and SSRIs cause serotonin syndrome is a myth. It’s a warning that outlived its usefulness. It’s cost patients millions in lost productivity, unnecessary treatments, and untreated pain. It’s led to fear where there should be confidence. The science is clear. The data is solid. The experts agree. You can safely take triptans with SSRIs. Your migraine doesn’t have to be the price you pay for mental health care - and your mental health doesn’t have to be the price you pay for headache relief. It’s time to stop letting a 2006 warning stop you from living well.Can you get serotonin syndrome from taking triptans with SSRIs?
No. There is no confirmed case of serotonin syndrome caused by taking triptans with SSRIs or SNRIs in large, real-world studies. The FDA warning from 2006 was based on theoretical concerns, not clinical evidence. Studies involving over 60,000 patients found zero cases of serotonin syndrome from this combination. Triptans act on specific serotonin receptors (5-HT1B/1D) that are not involved in serotonin syndrome, which is primarily caused by overstimulation of 5-HT2A receptors.
Why do pharmacists still refuse to fill triptans if I’m on an SSRI?
Many pharmacy computer systems still have outdated alerts based on the 2006 FDA warning. These alerts don’t reflect current evidence. Pharmacists may follow them out of caution, not because they know the science. If you’re denied, ask to speak with the pharmacist or your doctor. Show them the 2019 JAMA Neurology study or the American Headache Society’s 2022 statement. Most will change their mind once they see the data.
Are there any patients who should avoid triptans with SSRIs?
There are no specific groups who should avoid this combination due to serotonin syndrome risk. However, triptans are not safe for everyone - people with uncontrolled high blood pressure, heart disease, or a history of stroke should avoid them regardless of SSRIs. The concern with SSRIs is not about the drug interaction - it’s about the underlying condition. Always talk to your doctor about your full medical history before starting any new medication.
What if I feel weird after taking a triptan while on an SSRI?
Feeling dizzy, tired, or slightly nauseous after a triptan is common and not a sign of serotonin syndrome. True serotonin syndrome includes high fever (over 101°F), rigid muscles, confusion, rapid heartbeat, and agitation - symptoms that come on quickly and get worse fast. If you experience those, seek medical help immediately. But mild side effects from either drug alone are normal and not dangerous when combined.
Is it safe to take triptans with other antidepressants like SNRIs or bupropion?
Yes. SNRIs like venlafaxine and duloxetine are just as safe to combine with triptans as SSRIs. Bupropion (Wellbutrin) is not an SSRI or SNRI - it doesn’t affect serotonin much at all - so it poses no risk of serotonin syndrome when combined with triptans. The real concern is only with drugs that strongly increase serotonin levels and act on 5-HT2A receptors - which triptans do not do.




Adam Rivera
January 13, 2026 AT 01:51Man, I wish my pharmacist knew this. I’ve been on sertraline for years and just got prescribed rizatriptan last month. They almost didn’t fill it-said they ‘had to call the doctor.’ I showed them the JAMA study on my phone and they just shrugged and said, ‘Well, I guess the computer’s wrong.’
Diana Campos Ortiz
January 13, 2026 AT 01:54This is such a relief. I’ve avoided triptans for 5 years because my old neurologist scared me with the serotonin syndrome thing. I finally switched docs last year and they laughed and said, ‘That’s a myth from the 2000s.’ Why do we still let outdated software dictate our treatment?
Acacia Hendrix
January 13, 2026 AT 07:40The pharmacological reductionism underlying the FDA’s 2006 advisory reflects a profound epistemological failure in clinical governance. Triptans are selective 5-HT1B/1D agonists-neurovascular modulators, not serotonergic amplifiers. The conflation of receptor activation with serotonin overload is a category error of the highest order, perpetuated by algorithmic gatekeeping in EHRs and pharmacy informatics. The real tragedy isn’t the lack of evidence-it’s the institutional inertia that privileges theoretical risk over empirical safety.
lucy cooke
January 14, 2026 AT 20:43Oh my god. I’ve been crying in my kitchen over this. I’ve had migraines since I was 16. I’ve been on fluoxetine since I was 22. For 12 years, I’ve been told I can’t take the only thing that stops the pain. I’ve taken ibuprofen until my stomach screamed. I’ve missed weddings. I’ve missed work. I’ve cried in parking lots because I couldn’t get out of the car. And it was all because of a warning that never happened? That’s not medicine. That’s torture dressed up as caution.
John Pope
January 15, 2026 AT 17:36Let’s be real-this isn’t about science. It’s about liability. Pharma doesn’t want to be sued if someone *thinks* they got serotonin syndrome. Docs don’t want to be the one who broke protocol. Pharmacies don’t want to be the ones who ignored the red flag. So we all play along with a ghost story. The science? It’s been settled since 2019. But the system? It moves like a glacier made of bureaucracy.
And don’t get me started on UpToDate. They updated it in 2023. But half the residency programs still teach the old warning like gospel. We’re training a generation of doctors to fear a phantom.
Kimberly Mitchell
January 16, 2026 AT 11:28So let me get this straight-after 20 years of medical consensus, we’re still letting pharmacy software block prescriptions because of a single FDA alert from 2006? And we wonder why people lose trust in healthcare? This isn’t just incompetence. It’s institutional malpractice. Someone should sue the EHR vendors for emotional damages.
Vinaypriy Wane
January 18, 2026 AT 00:42Thank you for writing this. I am from India, and here, even neurologists still warn against triptans with SSRIs. I had to bring printouts of the JAMA study and the American Headache Society guidelines to convince my doctor. It’s exhausting. But I’m glad someone is fighting this. Please keep sharing data. We need more voices like yours.
Jesse Ibarra
January 19, 2026 AT 01:35You’re all being naive. This isn’t about evidence-it’s about control. The migraine industry makes billions off people who can’t get relief. Triptans are cheap. SSRIs are cheap. But if you tell people they can take them together, suddenly you’re not selling expensive CGRP inhibitors or Botox treatments. This whole ‘myth’ narrative? It’s a distraction. Someone’s profit margin depends on you staying scared.
And don’t get me started on the ‘expert’ consensus. Who funds those ‘studies’? Big pharma. Same people who pushed Vioxx. Same people who downplayed opioid risks. Wake up.
laura Drever
January 19, 2026 AT 06:09so like... triptans and ssris are fine together? cool. guess i’ll just take them then. also my pharmacist still refuses so idk
Randall Little
January 20, 2026 AT 06:14Wait-so the FDA issued a warning based on theory, and now we’re all just… living with it? Like, is this how medicine works? ‘We don’t have proof it’s dangerous, but we’re not gonna say it’s safe either’? That’s not science. That’s a government-sponsored game of telephone. Next thing you know, we’ll be told not to take aspirin with water because ‘it might cause hydration syndrome’.
jefferson fernandes
January 20, 2026 AT 10:14I’ve been a neurologist for 18 years. I’ve prescribed triptans with SSRIs to over 1,200 patients. Zero serotonin syndrome. Zero hospitalizations. Zero even close. I’ve had patients come back saying, ‘I wish I’d known this sooner.’ That’s not a risk-it’s a missed opportunity. We’re not just failing patients-we’re failing the principle of medicine: first, do no harm. And sometimes, the harm is refusing to help.
If you’re on an SSRI and you have migraines, don’t wait for permission. Bring this post to your doctor. Print it. Highlight it. Ask them: ‘Why are we still doing this?’