When someone struggles with both a mental illness like depression or schizophrenia and a substance use disorder, treating just one part of the problem rarely works. For years, people were sent to separate programs-one for addiction, another for mental health. But this split approach often left patients caught in the middle, confused, and unsupported. The truth is, these conditions don’t live in separate boxes. They feed each other. And the most effective way to break that cycle? Integrated dual diagnosis care.
Why Separate Treatment Fails
Imagine you’re dealing with anxiety and drinking to calm your nerves. You go to a mental health clinic, where your therapist tells you to stop drinking. Then you go to a rehab center, where they tell you to focus only on sobriety and not worry about your anxiety until later. Neither team talks to the other. You get conflicting messages. Your anxiety spikes without alcohol, so you relapse. Then you feel guilty. The cycle repeats. This isn’t hypothetical. It’s what happened to millions. Before integrated care, only about 6% of people with both a mental illness and a substance use disorder got help for both. That means over 15 million adults in the U.S. alone were left to manage two complex conditions on their own. Traditional parallel treatment-where services are delivered separately-isn’t just inefficient. It’s harmful. It increases hospital visits, raises the risk of overdose, and makes recovery feel impossible.What Is Integrated Dual Diagnosis Treatment (IDDT)?
IDDT, or Integrated Dual Disorder Treatment, is the gold standard for treating co-occurring conditions. Developed in the 1990s by researchers at Dartmouth and New Hampshire, it’s not just a new therapy. It’s a complete system change. Instead of two teams, you have one. Instead of two plans, you have one. Instead of choosing between mental health or sobriety, you work on both at the same time. The core idea is simple: your brain doesn’t separate mental illness from addiction. Neither should your care team. IDDT is built on nine proven components:- Motivational interviewing to help you find your own reasons for change
- Substance abuse counseling focused on reducing harm, not just demanding abstinence
- Group therapy that includes peers with similar struggles
- Family education so loved ones understand how both conditions interact
- Medication management that considers both psychiatric and addiction needs
- Connection to self-help groups like Alcoholics Anonymous or SMART Recovery
- Health promotion-nutrition, sleep, exercise-because physical health affects mental health
- Specialized strategies for those who don’t respond to initial treatment
- Relapse prevention that plans for setbacks, not just perfection
How IDDT Works in Real Life
A person with bipolar disorder and alcohol dependence doesn’t need to wait until they’re sober to start mood stabilizers. They don’t need to wait until their depression lifts to begin addressing drinking. In IDDT, the same clinician-trained in both mental health and addiction-helps them manage both. Take Maria, a 34-year-old from Sydney. She had PTSD and started using cannabis to numb flashbacks. After years of cycling between crisis centers and outpatient therapy, she joined an IDDT program. Her counselor didn’t demand she quit cannabis right away. Instead, they talked about *why* she used it, how it affected her sleep and mood, and what alternatives might help. Over time, Maria reduced her use, started taking her prescribed medication consistently, and joined a peer support group. She didn’t become ‘perfect’ overnight. But she stopped ending up in the ER. That’s the power of harm reduction-acknowledging that change is a process. You don’t have to be fully sober to start healing. You just have to be willing to try.
What Makes IDDT Different From Other Approaches
In sequential treatment, you treat one condition first, then the other. In parallel treatment, you get two separate services at the same time-but they don’t talk. In integrated treatment, you get one team, one plan, one voice. Here’s how they compare:| Approach | Team Structure | Treatment Plan | Effectiveness |
|---|---|---|---|
| Sequential | Two separate teams, one after the other | Two separate plans | Low-symptoms often worsen while waiting for the next stage |
| Parallel | Two teams working at the same time, but independently | Two separate plans | Moderate-reduces confusion but lacks coordination |
| Integrated (IDDT) | One team trained in both mental health and addiction | One unified plan addressing both conditions | High-proven to reduce substance use days and improve engagement |
Barriers to Getting IDDT
Even though IDDT works, most people still can’t access it. Why? First, funding. Most insurance systems still pay for mental health and addiction services separately. That makes it hard for clinics to combine them financially. Second, training. Not all therapists know how to treat both conditions. A counselor trained in CBT for depression might not know how to handle cravings in someone with schizophrenia. Third, stigma. Some providers still believe addiction is a moral failure, not a medical condition. A 2018 study found that even after a three-day IDDT training, many clinicians didn’t improve their skills in motivational interviewing. That’s a red flag. You can’t just hand out a manual and expect change. Real integration requires ongoing supervision, coaching, and organizational support.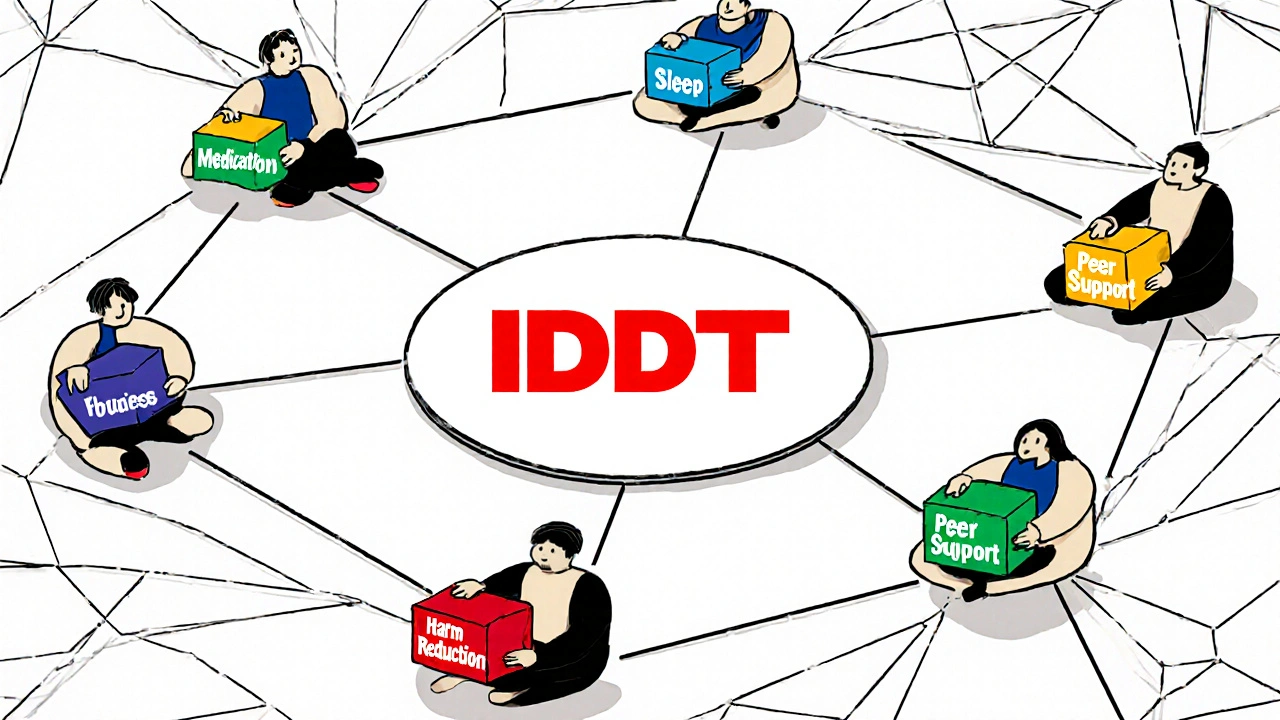
Who Benefits Most From IDDT?
IDDT isn’t just for people with severe mental illness. It helps anyone with a co-occurring disorder:- Someone with depression and opioid use
- A veteran with PTSD and alcohol dependence
- A young adult with ADHD and stimulant misuse
- A person with bipolar disorder and cannabis use
What’s Next for Integrated Care?
The need is growing. In 2023, an estimated 20.4 million U.S. adults had a dual diagnosis. Yet only 6% received integrated care. That gap is massive. Organizations like SAMHSA are pushing states to adopt IDDT through grants and technical support. Medicaid programs are starting to reimburse for integrated services. But real change needs more than policy-it needs investment in training, better data systems, and a cultural shift in how we view addiction. The future of mental health care isn’t about choosing between therapy and rehab. It’s about bringing them together. And that’s exactly what IDDT does.How to Find an Integrated Treatment Program
If you or someone you know needs help, here’s how to start:- Ask your current provider: “Do you offer integrated care for co-occurring mental health and substance use disorders?”
- Look for programs that mention “dual diagnosis,” “co-occurring disorders,” or “IDDT” on their website.
- Call and ask if the same clinician treats both conditions-or if there’s a team that coordinates care.
- Check if they use motivational interviewing and harm reduction principles.
- Ask about staff training: Are clinicians certified in both mental health and addiction treatment?
What is the difference between dual diagnosis and co-occurring disorders?
They mean the same thing. "Dual diagnosis" is an older term often used in clinical settings, while "co-occurring disorders" is the more modern, preferred term because it avoids implying that one condition is the "primary" diagnosis. Both refer to having a mental health disorder and a substance use disorder at the same time.
Can you recover from both conditions at the same time?
Yes. Recovery doesn’t mean being perfect. It means learning to manage both conditions so they don’t control your life. Many people in IDDT programs reduce substance use, stabilize their mood, rebuild relationships, and return to work or school-even if they still use substances occasionally. Progress, not perfection, is the goal.
Does IDDT require complete abstinence from drugs or alcohol?
No. IDDT uses a harm reduction approach. That means the focus is on reducing the negative consequences of substance use-not forcing immediate abstinence. For some, cutting back is the first step. For others, stopping completely happens later. The team meets you where you are, not where they think you should be.
Is IDDT covered by insurance?
It depends. Many private insurers and Medicaid programs now cover integrated services, especially as evidence grows. But you’ll need to ask. Call your provider and say: "Do you offer integrated treatment for mental health and substance use disorders under my plan?" If they say no, ask for a referral to a program that does.
How long does IDDT treatment last?
There’s no fixed timeline. Some people get intensive support for 6-12 months. Others stay connected to the team for years, adjusting care as their needs change. IDDT is designed to be flexible. It’s not a short-term fix-it’s long-term support built around your life.
What if I don’t trust my therapist?
Trust is essential. If you don’t feel heard or respected, it’s okay to ask for a different clinician. Integrated care only works if you feel safe. Ask for a different provider within the same program, or look for another program that better matches your needs. Your recovery depends on the relationship, not just the treatment model.





Shawn Daughhetee
November 24, 2025 AT 08:47Finally someone gets it. I've been stuck in that loop where my therapist told me to quit drinking and my rehab guy told me to stop obsessing over my anxiety. Neither helped. I relapsed twice. Integrated care saved my life.
Miruna Alexandru
November 24, 2025 AT 15:25While the concept of integration is theoretically sound, one must interrogate the epistemological foundations of this model. Is the conflation of psychiatric pathology with behavioral dependency not a reductive anthropological imposition? The binary of 'mental illness' versus 'addiction' may itself be a construct of neoliberal biopower, and to integrate them without deconstructing their ideological underpinnings risks perpetuating the very systems that pathologize suffering.
Justin Daniel
November 26, 2025 AT 03:26Wow, Miruna, you just turned a lifesaving treatment model into a thesis defense. 😅
Meanwhile, real people like Maria? They just want someone who won't tell them to 'get it together' while they're barely holding on. Integration isn't philosophy-it's compassion with a paycheck.
Melvina Zelee
November 27, 2025 AT 05:02im so glad this is getting talked about. i had bipolar and was using coke to feel 'normal' and every doc i saw was like 'fix your mood first' or 'get clean first' and i just felt like a broken toy being passed between repair shops. when i finally found a team that treated both at once? i cried. not because i was fixed, but because i felt seen. no more choosing between being a junkie or a crazy person. just me.
ann smith
November 27, 2025 AT 21:17This gives me so much hope 💛
Too many people are told they have to be 'perfect' before they can heal. But healing isn't about perfection-it's about progress. Thank you for sharing Maria's story. She's proof that small steps matter. You're not alone.
Latonya Elarms-Radford
November 29, 2025 AT 05:43Oh, how quaint. We now have a bureaucratic ballet of 'integrated care'-a sanitized, insurance-approved version of human suffering dressed in clinical jargon. Tell me, does the therapist take notes while the patient weeps? Does the chart have a checkbox for 'existential despair'? We have turned the sacred, messy, soul-crushing journey of recovery into a compliance matrix with nine bullet points. And we call this progress? We have not healed the wounded-we have merely cataloged their wounds for reimbursement.
Mark Williams
November 30, 2025 AT 03:30From a systems perspective, IDDT aligns with the biopsychosocial model, but implementation fidelity remains a critical variable. The 2018 study you cited on clinician skill retention post-training suggests a significant competency gap in motivational interviewing and harm reduction protocols. Without standardized competency-based credentialing for dual-diagnosis clinicians, we risk institutionalizing a model that's theoretically robust but operationally inconsistent.
manish chaturvedi
December 1, 2025 AT 18:46In India, we rarely talk about mental health, let alone addiction. But I’ve seen it-my cousin, brilliant artist, bipolar, drank to silence the voices. He was sent to a rehab center, told to 'pray harder.' Then to a psychiatrist, told to 'stop drinking.' No one connected the dots. Integrated care? It’s not just better-it’s the only way. We need this here. Not just in the West.
Ravi Kumar Gupta
December 3, 2025 AT 04:48THIS IS THE FUTURE! 🇮🇳🔥
Why are we still playing doctor roulette?! My brother died waiting for someone to 'choose' his illness. Now I fight for IDDT in rural clinics. We don't need more paperwork-we need more hearts who know: one soul, two battles, one team. No more silence. No more shame. Just care.