When an employee gets hurt on the job, the workers' compensation system steps in to cover medical care-including prescription drugs. But here’s the thing: generic substitution isn’t just a cost-saving trick. It’s now the standard of care in most states, and it works just as well as brand-name drugs. Yet many injured workers, and even some doctors, still hesitate. Why? Because they’re misinformed.
What Generic Substitution Actually Means
Generic substitution means replacing a brand-name drug with a chemically identical version that’s been approved by the FDA. It’s not a cheaper knockoff. It’s the same active ingredient, same strength, same way of being absorbed by the body. The FDA requires generics to meet the same strict standards as brand-name drugs. In fact, the same factories often make both-the only difference is the label and the price. In workers’ compensation, this isn’t optional in most places. As of 2025, 44 states and Washington, D.C., have laws that either require or strongly encourage pharmacists to substitute generics unless a doctor specifically writes "dispense as written" or documents medical necessity. Tennessee’s 2023 Medical Fee Schedule says it plainly: "An injured employee should receive only generic drugs... unless the authorized treating physician documents medical necessity for the brand-name product."Why It Matters for Cost and Care
Drug costs make up about 20% of total workers’ compensation medical spending. And brand-name drugs? Their prices have exploded. Between 2014 and 2019, the list price of the most common brand-name drugs used in workers’ comp rose by 65.5%. Meanwhile, the price of generic versions dropped by 35%. That’s not a typo. One drug that cost $100 as a brand-name product now costs about $20 as a generic-according to myMatrixx data. That’s an 80% savings. These savings add up fast. In 2016, 85.7% of all managed prescriptions in workers’ comp were generics. By 2023, that number jumped to 89.2%. In California, where formularies are tightly managed, generic use hit 92.7% in 2022. Colorado just passed a rule requiring 95% generic use on its state formulary, effective January 2024. That’s not just policy-it’s a financial lifeline for employers and insurers.How It Works in Practice
It’s not as simple as swapping a pill at the pharmacy. Pharmacy Benefit Managers (PBMs)-companies like OptumRx, Express Scripts, and Prime Therapeutics-run the show. They create formularies: lists of approved drugs. If a drug has a generic version on the formulary, the pharmacist must substitute it unless the doctor overrides it with a valid medical reason. Doctors don’t just pick drugs randomly. They follow state-specific rules. In states with strong formularies, like Tennessee or California, prescribing a brand-name drug means filling out extra paperwork. You can’t just say, "I prefer it." You need clinical justification: "The patient had an allergic reaction to the inactive ingredients in the generic," or "The generic caused a documented drop in therapeutic effect." Patient preference doesn’t count. The FDA doesn’t allow it. Neither do most state laws.Why Some People Still Doubt Generics
Here’s the biggest barrier: perception. A 2019 survey by Reduce Your Workers’ Comp Blog found that 68% of injured workers believed brand-name drugs were better. Even after using generics, 82% said they worked just as well-but the doubt stuck. Many think "generic" means "lower quality." It doesn’t. The FDA requires generics to be bioequivalent. That means they deliver the same amount of medicine into the bloodstream at the same rate as the brand-name version. Nurse practitioners in occupational health clinics hear the same thing over and over: "My doctor said I need the name brand." But in reality, most doctors aren’t trained in pharmacy cost dynamics. They learned about drugs in medical school, where brand names were the default. It takes time to unlearn that.When Generics Might Not Work
There are exceptions. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-small differences in absorption can matter. Even then, studies show that switching between generic and brand versions of these drugs rarely causes problems when done properly. Less than 2% of cases involve therapeutic failure, according to Coventry’s 2016 data. The bigger issue isn’t clinical-it’s market-related. A 2022 Enlyte report found that some generic manufacturers are accused of anti-competitive behavior: colluding to raise prices instead of competing. This has led to sudden spikes in the cost of certain generics, like digoxin or doxycycline. So while generics are still far cheaper than brands, the savings aren’t always as dramatic as they used to be.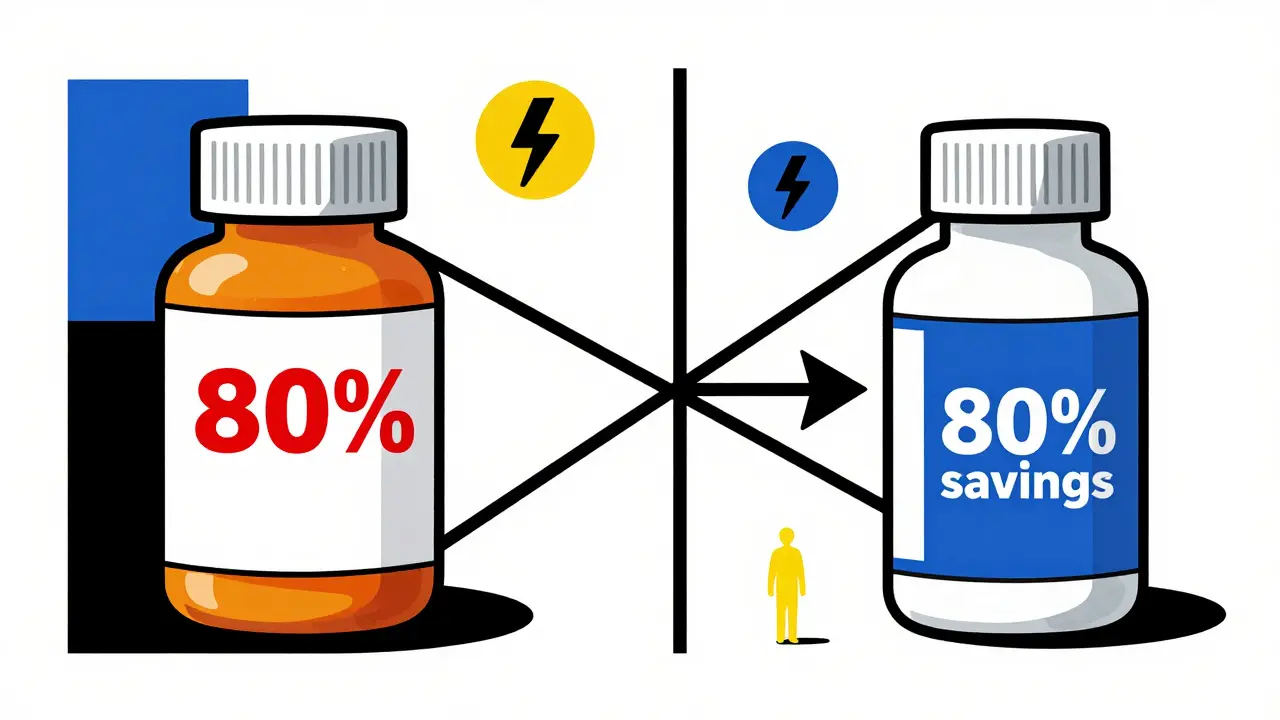
What Providers and Patients Need to Do
For doctors: Know your state’s formulary. Check the FDA’s Orange Book for therapeutic equivalence ratings. Don’t default to brand names. If you must prescribe one, document why-clearly and specifically. For patients: Ask your pharmacist if a generic is available. Ask your doctor why they’re prescribing a brand-name drug. Most of the time, the answer will be: "It’s cheaper and just as effective." For employers and insurers: Push for state-level formulary adoption. Support education campaigns. Train claims adjusters and case managers to recognize when brand-name drugs are being overused.The Future of Generic Substitution
The trend is clear: generics are winning. By 2025, experts predict generic use in workers’ comp will hit 93.5%. New challenges are emerging, though. Biosimilars-generic versions of complex biologic drugs-are starting to appear. Texas began allowing them in 2022. And as specialty drugs grow (they now make up 12.7% of pharmacy costs), the lack of generic alternatives is becoming a problem. Only 4.3% of specialty drugs have generic equivalents. The next frontier? Pharmacogenomics. Testing how a person’s genes affect their response to drugs could one day make substitution smarter-not just cheaper. Imagine knowing ahead of time that a patient won’t respond to a certain generic version of a painkiller. That’s not science fiction. It’s already being tested in pilot programs.Bottom Line
Generic substitution in workers’ compensation isn’t about cutting corners. It’s about using proven, safe, and affordable medicine. The data doesn’t lie: generics work. They save money. They don’t reduce outcomes. And with 44 states mandating or encouraging their use, the system is built around them. If you’re an injured worker, don’t assume brand-name means better. If you’re a provider, don’t default to the more expensive option without a real reason. And if you’re part of the system-employer, insurer, or administrator-support policies that make generics the standard. Because in workers’ compensation, the goal isn’t just to treat injuries. It’s to do it right, without wasting resources.Are generic drugs really as effective as brand-name drugs in workers’ compensation cases?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and bioequivalence as their brand-name counterparts. Studies consistently show no difference in clinical outcomes for the vast majority of medications used in workers’ compensation, including pain relievers, anti-inflammatories, and muscle relaxants. Over 89% of prescriptions in the system are now generic, and outcomes haven’t declined.
Can a doctor refuse to use a generic drug?
Yes, but only if they document medical necessity. In most states, simply saying "I prefer the brand" or "the patient asked for it" isn’t enough. The doctor must provide a clinical reason-like a documented allergic reaction to an inactive ingredient in the generic, or evidence that the patient previously failed to respond to the generic version. Without this documentation, the claim may be denied or the drug won’t be covered.
Why do some pharmacies still dispense brand-name drugs even when generics are available?
Sometimes it’s because the prescription was written as "dispense as written" or "no substitution." Other times, it’s due to outdated systems or lack of awareness. In rare cases, there may be a shortage of the generic version. But under state laws, pharmacists are required to substitute unless explicitly told not to. If you’re unsure, ask the pharmacist why they’re giving you the brand-name version.
Do generic drugs have more side effects than brand-name drugs?
No. The FDA requires generics to meet the same safety standards as brand-name drugs. The only differences are in inactive ingredients-like fillers or dyes-which rarely cause issues. If someone experiences side effects after switching, it’s more likely due to changes in dosage timing, underlying health conditions, or psychological expectations than the drug itself.
Which states don’t allow generic substitution in workers’ compensation?
As of 2025, 6 states do not have mandatory or strongly encouraged generic substitution laws. These include Virginia, which has more permissive language, and a few others with no formal formulary. However, even in these states, most insurers and PBMs still push for generics because of cost savings. The trend is moving toward universal adoption.
What should I do if my workers’ comp claim is denied because I took a generic drug?
If your claim was denied because you took a generic drug, that’s a mistake. Generics are approved for use in workers’ comp across the country. Contact your claims administrator and ask for a written explanation. If they claim the generic wasn’t covered, request a copy of the state’s drug formulary. In nearly every case, the denial can be overturned with a simple correction.






linda permata sari
December 31, 2025 AT 19:13Okay but can we talk about how wild it is that people still think generics are ‘cheap junk’? 🤦♀️ I had a back injury last year and got the generic version of my pain med-same pill, same effect, saved my employer $80 a month. My doctor didn’t even blink. The only thing different? The label. And yeah, I still got my life back. 🙌
Brandon Boyd
January 2, 2026 AT 15:43Look, I used to be the guy who’d beg for the brand name because ‘it just feels better.’ Then I did the math. $100 vs $20? For the same chemical? That’s not frugality-that’s common sense. And yeah, the system’s rigged sometimes with PBMs playing games, but that’s not the generic’s fault. It’s the system. Fix the system, not the medicine. Generics aren’t the enemy. Greed is.
Branden Temew
January 3, 2026 AT 12:24So let me get this straight-we’ve got a healthcare system that’s so broken, the only thing we can agree on is that pills with different colored dots are magically the same? 🤔 I mean, if two drugs are chemically identical, why do we even have brand names? Why not just call them ‘Drug A’ and ‘Drug B’ and be done with the marketing circus? The FDA says they’re the same. The data says they’re the same. But we still pay $100 for a pill because someone in a suit decided ‘BrandX’ sounds more trustworthy than ‘GenericY.’ That’s not science. That’s theater.
Frank SSS
January 4, 2026 AT 18:59Yeah, sure, generics are cheaper. But have you ever had one that just… didn’t work? Like, you take it, feel nothing, then switch back to the brand and boom-pain gone? It happens. Not often, but it happens. And now they’re forcing it? No room for nuance? No empathy? Just ‘take the cheap one.’ I get the savings, but people aren’t numbers. Some of us aren’t lab rats.
Paul Huppert
January 5, 2026 AT 18:08Just curious-when a doctor writes ‘dispense as written,’ how often is it actually for medical reasons vs just habit? I’ve seen it so many times and never heard a real explanation. Feels like inertia more than intent.
Hanna Spittel
January 7, 2026 AT 06:55⚠️ BIG RED FLAG: PBMs are secretly hoarding generics to jack up prices. 🚨 I read a leak-some companies are buying up all the generic versions of a drug just to make them scarce. Then they sell them at 3x. It’s not a conspiracy… it’s capitalism. 🤫💸
Brady K.
January 7, 2026 AT 20:58Let’s cut through the jargon: 92% generic use? That’s not a win-it’s a mandate disguised as efficiency. We’re optimizing for balance sheets, not outcomes. And now we’re talking about pharmacogenomics? Cool. But if we can’t even get doctors to stop defaulting to brand names because they’re lazy or uninformed, how the hell are we gonna roll out gene-based prescribing? We’re building a Tesla while still using horse cart roads. The infrastructure’s not ready. The policy is ahead of the practice. Again.
Kayla Kliphardt
January 8, 2026 AT 22:39Thanks for laying this out so clearly. I’ve been hesitant to ask my doctor about generics because I didn’t want to sound like I was trying to save money. But now I feel like I can actually have the conversation. Really helpful.