More than 1 in 10 people believe they have a drug allergy. But here’s the truth: most of them don’t. A lot of people walk around thinking they’re allergic to penicillin because they got a rash as a kid, or they avoided a medication after a stomach upset, or they heard a story from a friend. The problem? Many of these aren’t true allergies at all. They’re side effects, not immune reactions. And that misunderstanding is costing lives, money, and treatment options.
Penicillin: The Most Misunderstood Drug Allergy
Penicillin is the number one drug people say they’re allergic to. About 10% of Americans claim it. But when you test them properly-skin test followed by a small oral dose of amoxicillin-over 90% turn out to be fine. That’s not a small number. That’s millions of people who could be safely using one of the safest, cheapest, and most effective antibiotics out there.Why does this matter? Because if you’re labeled penicillin-allergic, doctors reach for stronger, broader-spectrum antibiotics. Those drugs cost more. They cause more side effects. And they contribute to antibiotic resistance. A 2017 study found patients with a penicillin allergy label stayed in the hospital half a day longer and paid over $1,000 more per admission. That’s not just inconvenient. It’s dangerous.
True penicillin allergy is IgE-mediated. That means your body makes antibodies that react within minutes to hours, causing hives, swelling, trouble breathing, or anaphylaxis. But most people who think they’re allergic never had that kind of reaction. A mild rash days after taking the drug? That’s often not IgE. It could be a virus, a reaction to something else, or just a harmless side effect. And here’s the kicker: many people outgrow penicillin allergies. If you haven’t taken penicillin in 10 years, your risk of reaction drops dramatically.
Antibiotics Beyond Penicillin
Penicillin isn’t alone. Other antibiotics are common triggers too. Cephalosporins like cephalexin are often avoided out of fear, but cross-reactivity with penicillin is actually less than 3%-not the 10% many doctors still believe. You don’t need to avoid all antibiotics just because you reacted to one.Sulfa drugs are another big one. Trimethoprim-sulfamethoxazole (Bactrim) is used for urinary infections, sinus infections, and even some pneumonia cases. About 3% of the general population reacts to sulfa antibiotics. But if you have HIV, that number jumps to 60%. The reaction here isn’t always IgE. It’s often a delayed T-cell response, causing rash, fever, or organ inflammation weeks after starting the drug. That’s why it’s easy to miss.
Quinolones like ciprofloxacin and levofloxacin also cause reactions. People report rashes, joint pain, or even tendon rupture. But not all of those are allergic. Some are side effects of the drug’s mechanism. Still, if you’ve had a severe reaction-like blistering skin or trouble breathing-you need to avoid it. And if you’re unsure? Get tested.
NSAIDs: More Than Just a Stomachache
Ibuprofen, naproxen, aspirin-these are everywhere. But they’re also one of the top triggers for hypersensitivity reactions. Unlike penicillin, NSAID reactions aren’t always IgE-mediated. In fact, most are pharmacological. That means the drug directly interferes with your body’s chemistry, not your immune system.Aspirin-exacerbated respiratory disease is a unique form of this. It affects 7% of adults with asthma and 14% with nasal polyps. These people don’t get hives. They get nasal congestion, wheezing, and sometimes full-blown asthma attacks within minutes of taking aspirin or other NSAIDs. It’s not an allergy in the classic sense, but it’s just as dangerous. Avoiding these drugs is necessary. And yes, there’s a treatment: aspirin desensitization, done under medical supervision, can help some people tolerate them again.
One key point: if you react to one NSAID, you might not react to all. Acetaminophen (Tylenol) is usually safe for people with NSAID hypersensitivity. But don’t assume. Test it with your doctor.
Anticonvulsants and the Hidden Genetic Risk
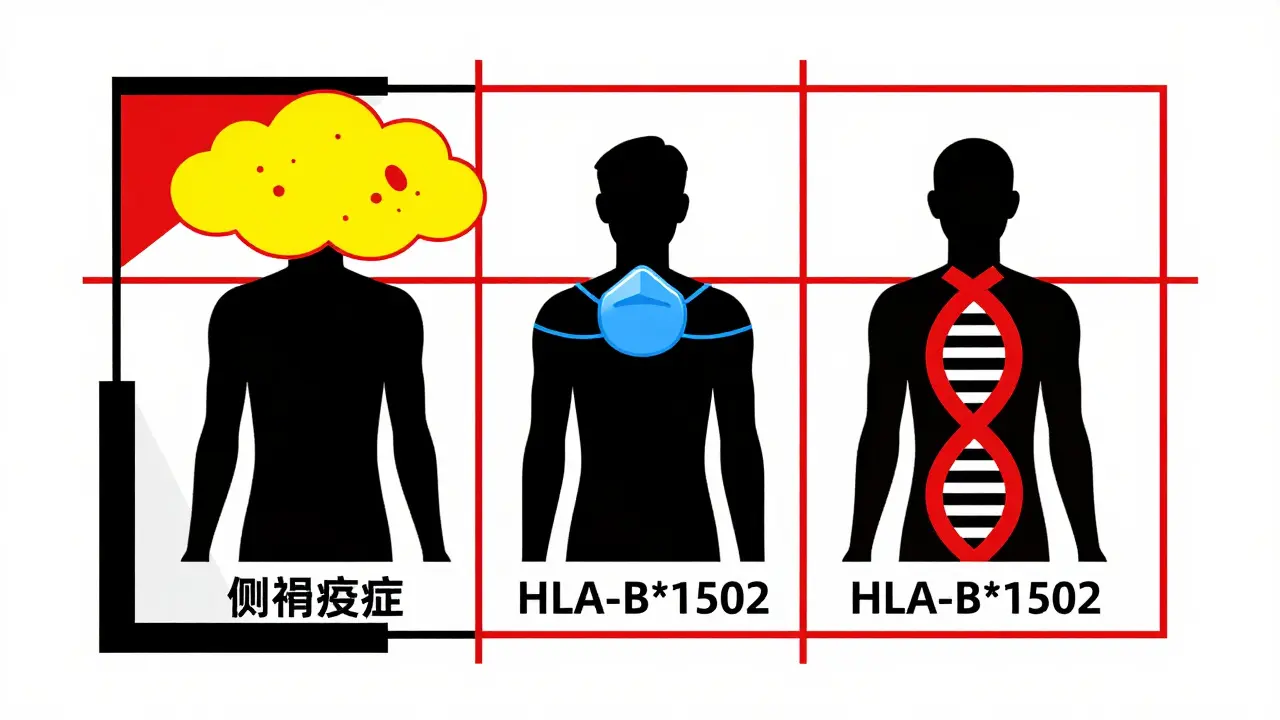
Carbamazepine (Tegretol), lamotrigine (Lamictal), phenytoin-these are life-saving for people with epilepsy and bipolar disorder. But they carry a hidden risk: severe skin reactions like Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). These are rare. But when they happen, they’re deadly.Here’s where it gets personal: genetics. If you carry the HLA-B*1502 gene, your risk of SJS from carbamazepine jumps 100-fold. That gene is common in Southeast Asia-10-15% of people in Thailand, Malaysia, and parts of China carry it. It’s rare in people of European descent. That’s why the FDA now recommends testing for this gene before prescribing carbamazepine in high-risk populations. In Taiwan, after they started screening, SJS cases from carbamazepine dropped by 90%.
Lamotrigine causes rashes in 5-10% of patients. Most are mild. But 1 in 1,000 patients develop a serious reaction. The risk is highest in the first few weeks. That’s why doctors start low and go slow. If you get a rash, don’t ignore it. Call your doctor immediately. Don’t wait to see if it goes away.
Chemotherapy and Biologics: The New Frontier
Cancer drugs are a major source of hypersensitivity. Taxanes like paclitaxel (Taxol) cause reactions in up to 41% of patients. Most are infusion reactions-flushing, chills, low blood pressure-happening during or right after the drip. They’re not always IgE. Often, it’s the drug triggering immune cells directly.Monoclonal antibodies like cetuximab (Erbitux) are even trickier. In some populations, especially in the southern U.S., people have pre-existing IgE antibodies to a sugar molecule in the drug (alpha-gal). That means the first time they get cetuximab, they can go into anaphylaxis. It’s not common, but it’s real. And it’s why premedication with steroids and antihistamines is now standard.
As biologics become more common-used for autoimmune diseases, cancer, and even migraines-these reactions will rise. The demand for allergists is expected to grow 20% by 2030. We’re not ready for it.
Contrast Dyes and Other Surprises
When you get a CT scan, you often get iodine-based contrast dye. About 1-3% of people have a reaction. Most are mild-nausea, itching, a warm feeling. But 0.01-0.04% have severe reactions. That’s rare, but scary.Here’s the myth: if you’re allergic to shellfish, you’re at higher risk. That’s not true. Shellfish allergies are to proteins. Contrast dye is iodine. No connection. But if you’ve had a prior reaction to contrast dye, you’re at higher risk for another. That’s why premedication with steroids and antihistamines cuts severe reactions from 12.7% down to 1%.
How to Know If It’s Really an Allergy
If you think you have a drug allergy, here’s what to do:- Write down exactly what happened. When? How long after? What symptoms? Did you get hives? Swelling? Trouble breathing? Or just a rash that appeared days later?
- Don’t assume. Just because your mom is allergic to penicillin doesn’t mean you are.
- Ask for a referral to an allergist. Skin testing for penicillin is 97-99% accurate. Oral challenge tests are even more reliable.
- If you’ve had a mild rash years ago, you might be able to safely take the drug again.
- Don’t avoid necessary medications out of fear. The risks of untreated infection or disease are often greater.
The bottom line: if you’ve been told you’re allergic to a drug, get it checked. You might be able to use safer, cheaper, more effective treatments. And you might be helping reduce antibiotic resistance in your community.
What to Do If You Have a True Drug Allergy
If testing confirms a true allergy:- Get an emergency medical alert bracelet. It should list the drug and reaction type.
- Keep a written list of your allergies and share it with every doctor, pharmacist, and hospital you visit.
- Ask about alternatives. There’s almost always another option.
- If you need the drug for life (like chemotherapy), ask about desensitization. It’s not a cure, but it lets you safely receive the treatment.
- Teach your family what to do if you have a reaction. Time matters.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as a child lose it after 10 years without exposure. The immune system forgets. That’s why retesting is so important-many people carry outdated labels that limit their care unnecessarily.
Is a rash always a sign of drug allergy?
No. Many rashes from medications are not allergic. Viral infections, heat, or even the medication’s side effects can cause rashes. A true allergic rash usually appears within hours, is itchy, and may be accompanied by swelling, breathing issues, or fever. Delayed rashes (after 3+ days) are often T-cell mediated and still need attention, but they’re not always IgE allergies.
Can I take a different antibiotic if I’m allergic to penicillin?
Yes, but not all alternatives are better. Some are broader-spectrum, which increases risk of side effects and antibiotic resistance. Cephalosporins are often safe if your penicillin reaction was mild. Macrolides like azithromycin or doxycycline are common alternatives. But the best option is to confirm your allergy with testing-many people can safely use penicillin again.
Are there tests for drug allergies?
Yes. For penicillin, skin testing with specific reagents (like Pre-Pen) followed by an oral amoxicillin challenge is the gold standard. It’s 97-99% accurate. For sulfa drugs or anticonvulsants, there’s no reliable skin test. Diagnosis relies on history and sometimes oral challenges under supervision. Genetic testing is available for carbamazepine and abacavir.
What should I do if I have a severe reaction?
If you have trouble breathing, swelling of the throat, dizziness, or a rapid drop in blood pressure, use an epinephrine auto-injector if you have one, call emergency services immediately, and go to the ER. Even if symptoms improve, you still need medical evaluation. Delayed reactions can happen hours later. Never ignore a severe reaction.
Next Steps: What You Can Do Today
If you’ve ever been told you’re allergic to a medication:- Look at your medical records. What was the reaction? Was it tested?
- Call your primary doctor. Ask if you should see an allergist for evaluation.
- If you’re scheduled for surgery or a CT scan, mention your allergy. Ask if testing is available.
- Don’t assume your child’s childhood reaction is still active. Re-evaluation after 10 years is smart.
- Share this info with family. Drug allergies affect more than just you.
Medications save lives. But only if we use them correctly. Don’t let a mislabeled allergy keep you from the best treatment. Get it checked. Your health depends on it.



Marie Fontaine
February 9, 2026 AT 03:00Just got my penicillin skin test done last week and turns out I’m not allergic lol 😅 Been avoiding it since I was 8 because of a rash that was probably poison ivy. My doctor laughed and said I’ve been overpaying for antibiotics for 15 years. Time to finally get that UTI treated right.
Ryan Vargas
February 10, 2026 AT 18:48The systemic implications of mislabeled drug allergies are not merely clinical-they are sociopolitical. The pharmaceutical-industrial complex thrives on diagnostic ambiguity, and the entrenched habit of labeling adverse drug reactions as ‘allergies’ perpetuates a cycle of profit-driven polypharmacy. We are not talking about isolated cases; we are talking about a structural failure in medical epistemology. The 90% false-positive rate for penicillin allergy is not an anomaly-it is a feature. The system benefits from overprescribing broad-spectrum antibiotics because they are more expensive, more patent-protected, and more easily marketed. This is not negligence. This is capitalism.
Ashlyn Ellison
February 12, 2026 AT 15:38My mom’s allergic to sulfa. Got a rash after Bactrim in the 80s. Never got tested. Now she’s on this expensive antibiotic for every little infection. I showed her this article. She’s calling her doctor tomorrow. Small wins.
Scott Conner
February 13, 2026 AT 11:51wait so if i had a rash from amoxicillin when i was 5 and never took it again am i really allergic? or just… unlucky? 🤔
Alex Ogle
February 13, 2026 AT 13:51I used to think I was allergic to ibuprofen because I got a weird rash once after a marathon. Turns out I was dehydrated, had a viral rash, and the timing was just bad. I took naproxen last year for back pain-no problem. But now I’m paranoid every time I take anything. What if the next one is the one? I don’t trust medicine anymore. Not really.
Tatiana Barbosa
February 13, 2026 AT 22:20As someone who’s had two anaphylactic reactions to NSAIDs and now does desensitization therapy-this is life-changing info. If you think you’re allergic, get tested. Don’t let fear rob you of quality of life. I can now take aspirin for my heart without panic. That’s not magic-that’s science. And your body? It remembers less than you think. Trust the data, not the ghost story from 2007.
Random Guy
February 14, 2026 AT 22:51so let me get this straight… the medical industry is scamming us by telling people they’re allergic so they can sell them $200 antibiotics instead of $2 penicillin? wow. i bet the pharma bros are sipping champagne on a yacht right now. 🥂💀
Simon Critchley
February 15, 2026 AT 02:48Interesting how the HLA-B*1502 allele distribution mirrors historical migration patterns. Southeast Asian populations have high prevalence due to selective pressure from endemic malaria-similar to sickle cell trait. The fact that we now have pharmacogenomic screening tools is a triumph of translational medicine. Yet, access remains inequitable. In the UK, only 12% of GP practices offer pre-prescription HLA testing. That’s not progress-it’s negligence. We need policy reform, not just patient education.
Tom Forwood
February 15, 2026 AT 05:41My cousin in Manila got SJS from carbamazepine. Died at 22. They didn’t screen her. No one told her family about the gene. That’s why I push this stuff hard. If you’re Asian or have Asian ancestry? Ask your doc about testing before any anticonvulsant. One question could save your life. Seriously.
John McDonald
February 15, 2026 AT 20:31Just got my penicillin challenge done. Turned out fine. They gave me a tiny dose of amoxicillin in the clinic, watched me for 2 hours. No reaction. I cried. Not because I was scared-I was mad. Mad that I avoided penicillin for 20 years because of a rash I got as a kid. Mad that I paid $1800 extra in hospital bills because of a myth. This article? Should be mandatory reading for every high school health class.
Jacob den Hollander
February 16, 2026 AT 17:41I’ve been telling my sister for years to get tested for her penicillin allergy. She said ‘I don’t wanna be poked with needles.’ I said ‘You’re gonna get poked with a needle every time you get an infection and they give you something that makes you vomit for a week.’ She finally did it. Turned out negative. Now she’s on penicillin for her sinus infection and says it’s ‘way better than the one that made her feel like a zombie.’ I’m so proud. Please, if you think you’re allergic-get it checked. It’s not scary. It’s just… smart.
John Watts
February 17, 2026 AT 13:59My kid had a rash after amoxicillin. We thought it was an allergy. Turned out it was a virus. I’m so glad I read this. Now I’m telling everyone I know. We need to stop treating drug reactions like black-and-white labels. Medicine’s messy. Our bodies are complex. Let’s stop being afraid of the gray area.
Randy Harkins
February 19, 2026 AT 01:36I’m an ER nurse. I’ve seen people die because they were labeled allergic and got a worse antibiotic. I’ve seen people get better faster and pay less when we switched them to penicillin. This isn’t theory. This is daily reality. Please. Get tested. Your life might depend on it. 💙